ENT Emergencies - McMaster University
advertisement

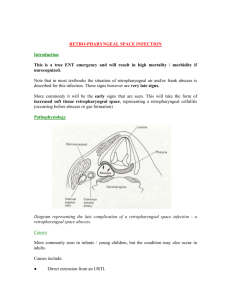
ENT EMERGENCIES McMaster University POS 2009 Overview ENT • Ears = Otologic • Nose = Rhinologic • Throat = Oral/Pharyngeal/Laryngeal –Infections –Facial injuries –Airway Obstruction Otologic Anatomy • Auricle • Ear canal • Tympanic membrane • Middle ear & mastoid • Inner Ear Trauma of the Auricle • Subperichondrial Hematoma – Shear force trauma – Perichondrium lifted & bleeds – Drain before cartilaginous necrosis – Leave drain, Abx, bolster dressing, monitor/24hrs – “Cauliflower” ear asymmetric cartilage formation Aspiration of Auricular Hematoma Middle Ear • Mastoiditis – Venous connection with brain, need aggressive treatment (can lead to brain abscess or meningitis) Epistaxis • 90% (Little’s Area) Kiesselbach’s plexus usually children, young adults • 10% of all epistaxis - usually in the elderly Nasal Septum Lateral Wall LOCALIZATION OF EPISTAXIS POSTERIOR : LATERAL WALL Behind the middle turbinate Entrance of Sphenopalatine artery Epistaxis in elderly and HBP Epistaxis Management • Pain meds, lower BP, calm patient • Prepare ! (gown, mask, suction, speculum, meds and packing ready) • Evacuate clots • Topical vasoconstrictor and anesthetic • Identify source Epistaxis Management • Anterior Sites - Pressure +/- cautery and/or tamponade - all packs require antibiotic prophylaxis Epistaxis Posterior Packing • Need analgesia and sedation • require admission and 02 saturation monitoring Epistaxis Complications • • • • severe bleeding hypoxia, hypercarbia sinusitis, otitis media necrosis of the columella or nasal ala Parotitis • Usually viral -paramyxovirus • Bacterial - elderly, immunosuppressed - associated with dehydration • - Management cover - Staph, anaerobes Hydrate Sialogogues Warm compresses Pain control Peritonsillar Abscess • Cellulitis of the space behind tonsillar capsule extending onto soft palate leading to abscess. The pus is located between the tonsillar bed and the capsule anterosuperior to the anterior pillar. • Complication from acute/chronic tonsillitis vs. Weber’s gland • Unilateral • Most common 10-30 years old Left Peritonsillar Abscess Left Peritonsillar Abcess Left Peritonsillar Abscess CT-SCAN peritonsillar abscess Peritonsillar Abcess • Inferior - medial displacement of tonsil and uvula • dysphagia, ear pain, muffled voice, fever, trismus • Group A strep, Strep pyogenes, Staph aureus, H. influenzae, Anaerobes • Treatment - Antibiotics (clinda), I&D, +/-steroids Epiglottitis Clinical Picture • Acute inflammation causing swelling of the SupraGlottic structures of the larynx • Older children & adults • decrease incidence in children secondary to HIB vaccine • Onset rapid, patients look toxic • prefer to sit, muffled voice, dysphagia, drooling, restlessness Epiglottitis • • • • Avoid agitation Direct visualization if patient allows soft tissue of neck Prepare for emergent airway, best achieved in a controlled setting • Unasyn, +/- steroids Soft tissue X-ray of neck • Anterior-posterior view is normal • Lateral view: ***THUMB PRINT*** – swelling epiglottis/ary epiglottic folds – fullness of the valleculae – ballooned hypopharyx – assess the retropharyngeal space Epiglottitis Acute epiglottitis: swan neck Management • In Children: – Brought in the operating room – Be ready to Intubate – Have a rigid Bronchoscope ready – Have the Tracheostomy tray opened • ***All need to be intubated to secure the airway due to the smaller airway in the child.*** Management • In Adult: – All need to be admitted – ICU or Step-down Unit – Intubation only if compromise airway – Continuous O2 sat monitoring – Daily examination of their larynx Retropharyngeal Abcess • Anterior to prevertebral space and posterior to pharynx • Usually in children under 4 (lymphoid tissue in space) • pain, dysphagia, dyspnea, fever • swelling of retropharyngeal space on lateral x-ray • Complications - mediastinitis Deep Neck Space Infection Ludwig’s Angina • Rapid bilaterally spreading cellulitis/inflammation with possible abscess formation of superior compartment of the suprahyoid space: – Submandibular, sublingual, submental spaces • usually in elderly debilitated patients and precipitated by dental procedures • massive swelling with impending airway obstruction Ludwig Angina Infectious Spread Ludwig’s Angina • Etiology: – typically from an odontogenic infection • mandibular 2nd or 3rd molar – streptococcus, oral anaerobes Clinical presentation • Very tender swelling under mandible + floor mouth • Usually little or no fluctuance • Severe trismus, drooling of saliva • Gross swelling, elevation, displacement of tongue • Tachypnea and dyspnea may happen • Danger of upper airway obstruction + death Ludwig angina: swelling Ludwig angina: trismus Management • ABC’s – Awake intubation vs tracheostomy if needed • Admit ICU or stepdown unless the airway is totally safe (02 sat monitoring) • Drain the abscess • I.V. ATB: penicillin, clindamycin, flagyl Angioedema • Ocassionally life threatening • Acquired -IgE mediated: vasodilation and increased vascular permeability (ie. insect bites, food, etc) -not IgE mediated (ie. ace inhibitors) • Hereditary • Tx: O2, anti-histamine, steroids, epinephrine • Consider intubation/trach Airway Obstruction • All the previously mentioned airway issues can eventually obstruct the patient: • Note: – Aphonia - complete upper airway – Stridor - incomplete upper airway – Wheezing - incomplete lower airway – Loss of breath sounds- complete lower airway Airway Management • A good rule of thumb about a tracheotomy is if you think about it, you probably should do it. • If you need a surgical airway then a cricothyrotomy is the way to go Complications of acute sinusitis • Orbital: – preseptal:periorbital cellulitis – postseptal: orbital cellulitis – subperiosteal abscess – orbital abscess • Intracranial: – meningitis – brain abscess – cavernous sinus thrombosis • Osteomyelitis frontal bone: – Pott’s Puffy tumor Periorbital cellulitis Orbital cellulitis Subperiostal orbital abscess Cavernous sinus thrombosis • Absence of valves in the orbital veins allows the blood to flow to the cavernous sinus • • • • • Rapidly progressive chemosis, ophthalmoplegia Severe retinal engorgement High fever Prostation May progress to vision loss, meningitis, death Intracranial complications • • • • • • • Headache Fever N/V Focal neurological deficits Lethargy Nuchal rigidity Deterioration of level consciousness Management of Complications of Acute Sinusitis • • • • • ENT, opht, ID, & neurosx consult CT , MRI I.V. ATB usually prolonged course Drainage of any abscess Orbital decompression if visual acuity decreased • Heparinization (Cavernous Sinus Thrombosis) Questions and Answers Question? • You are seeing a 50 yr old male in the ER for query epiglottitis? During your physical exam the patient stops making any airway sounds, turns blue, grasping at neck & collapses in bed. How do you manage this patient? • A) immediately place a chest tube b/c patient most likely has a tension pnemothorax • B) immediately place an oxygen mask on patient at fi02 100% • C) immediately call for surgeon on call to come place a tracheostomy tube • D) immediately perform a cricothyrotomy • E) immediately call for a CXR and place a central line Question? • What is the name of the sign for epiglottitis seen on soft tissue neck X-ray? • A) Steeple sign on AP neck films • B) Birds beak sign on Lat neck films • C) Thumb printing sign on AP neck films • D) Hour glass sign on Lat neck films • E) Thumb printing sign on Lat neck films Question? • What is the name of the sign for epiglottitis seen on soft tissue neck X-ray? • A) Steeple sign on AP neck films • B) Birds beak sign on Lat neck films • C) Thumb printing sign on AP neck films • D) Hour glass sign on Lat neck films • E) Thumb printing sign on Lat neck films Question? • A 65 yr old male patient presents to the ER with severe epistaxis. He has a significant cardiac Hx and is currently taking coumadin and aspirin. He states that it began 6 hrs ago and he has soaked through 3 towels and has vomited what looks like dark blood twice. HR is 125 and BP is 90/70. Manage this patient! What tests/medications should you order? Pick 6 from the following list. Question cont • • • • • • • • • CBC Morphine 5mg IV Metoprolol 5mg IV INR/PTT Large bore IV U/S Serum Calcium Serum lytes Urine lytes • • • • • • • • • 2/3 1/3 IV solution RL IV solution ½ NS IV solution Stat CT scan Cross & type 2 units PRBC Stat CXR Stat ECG Foley Nasal packing Question cont • • • • • • • • • CBC Morphine 5mg IV Metoprolol 5mg IV INR/PTT Large bore IV U/S Serum Calcium Serum lytes Urine lytes • • • • • • • • • 2/3 1/3 IV solution RL IV solution ½ NS IV solution Stat CT scan Cross & type 2 units PRBC Stat CXR Stat ECG Foley Nasal packing Question? • A patient with a peritonsillar abscess usually has: – – – – – A) trismus B) upper airway obstruction C) dysphagia D) Hemoptysis E) Mononucleolus Ans: A only, or A&C, or A&C&E, or D only Question? • A patient with a peritonsillar abscess usually has: – – – – – A) trismus B) upper airway obstruction C) dysphagia D) Hemoptysis E) Mononucleolus Ans: A only, or A&C, or A&C&E, or D only Question? • The vessel most likely to cause significant bleeding following tracheostomy is: – Aorta/carotid – innominate – inferior thyroid – Internal jugular – Subclavian artery Question? • The vessel most likely to cause significant bleeding following tracheostomy is: – Aorta/carotid – innominate – inferior thyroid – Internal jugular – Subclavian artery Question? • Regarding tracheostomies, the following facts are true except: – tracheostomies are commonly indicated for long term ventilation or airway protection – swallowing problems are fairly common in patients with tracheostomies – an appropriately placed tracheostomy with its cuff inflated virtually eliminates the risk of aspiration – tracheostomies should be placed at the level of the second or third cartilaginous ring – a tracheo-innominate fistula may occur with tracheostomies placed too low in the trachea Question? • What is the most common cause of death in patients with tracheostomies. – Increased aspiration – Tube falling out – Bleeding – Tube becoming obstructed – Infection Question? • What is the most common cause of death in patients with tracheostomies. – Increased aspiration – Tube falling out – Bleeding – Tube becoming obstructed – Infection Question? • To avoid the complications of tracheostomy: Which of the following are True? – a tracheostomy tube of appropriate size, length and curvature must be used – two tracheal rings must be removed – judicious suctioning to avoid aspiration of blood during the procedure – the skin must be closed tightly around the tracheostomy tube Question? • To avoid the complications of tracheostomy: Which of the following are True? – a tracheostomy tube of appropriate size, length and curvature must be used – two tracheal rings must be removed – judicious suctioning to avoid aspiration of blood during the procedure – the skin must be closed tightly around the tracheostomy tube Question? • In a patient requiring a cuffed tracheostomy tube for prolonged closed ventilation, tracheal injury can be best prevented by? – Frequent cuff deflation. – Use of a non-reactive cuff. – Use of an alternating double cuff tube. – Use of a wide cuff. – Use of a minimal cuff volume to effect adequate seal. Question? • In a patient requiring a cuffed tracheostomy tube for prolonged closed ventilation, tracheal injury can be best prevented by? – Frequent cuff deflation. – Use of a non-reactive cuff. – Use of an alternating double cuff tube. – Use of a wide cuff. – Use of a minimal cuff volume to effect adequate seal.