Dysphagia disease
advertisement
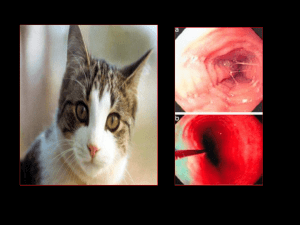
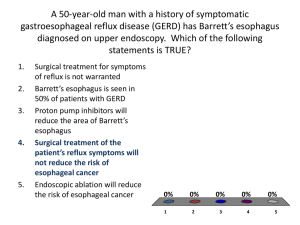
Dysphagia Dr.Krisana Thaitong Dysphagia must be distinguished from globus sensation Globus is a sensation of a lump in the throat in which food transport is not limited globus is not related to swallowing and, in fact, may improve with swallowing Dysphagia Oropharyngeal dysphagia Esophageal dysphagia Dysphagia Dysphagia ↙ Oropharyngeal dysphagia ▼ Neuromuscular dysfunction ▼ •Cerebrovascular accidents •Amyotrophic Lateral Sclerosis (AML) •Parkinson's disease •Myasthenia gravis •Tardive dyskinesia. ↘ Esophageal dysphagia ▼ •Achalasia •Nonachalasia Motility Disorders •Strictures •Rings/Webs •GERD •Extraesophageal GERD •Neoplasia •Esophageal Diverticula •Foreign Bodies •Pill-Induced Injury •Infectious Esophagitis •Caustic Injury Esophageal dysphagia ↙ Solids only ↘ Solids & liquids ▼ ▼ Mechanical obstruction ↙ Intermittent ▼ Motility disorder ↘ progressive ▼ •Rings/Webs •Strictures •Malignancy ↙ Intermittent ▼ •Esophageal spasm ↘ progressive ▼ •Achalasia •Scleroderma Oropharyngeal dysphagia abnormality related to the movement of a food bolus from the hypopharynx to the esophagus arises from disease of the upper esophagus, pharynx, or UES. typically present with difficulty initiating a swallow and immediately experience coughing, choking, gagging, or nasal regurgitation when attempting to swallow most common caused by disruptions in swallowing secondary to neuromuscular dysfunction this setting, the symptoms may be more severe when swallowing liquids The history and physical examination should focus on neurologic signs and symptoms Neuromuscular dysfunction Cerebrovascular accidents Amyotrophic Lateral Sclerosis (AML) Parkinson's disease Myasthenia gravis Tardive dyskinesia. Rarely, structural abnormalities caused such as ♥ cervical osteophytes ♥ hypopharyngeal diverticulum (Zenker's diverticulum) ♥ tumors ♥ postcricoid webs typically note difficulty with a solid food bolus leaving the mouth Oropharyngeal swallow is best assessed by videofluoroscopy, also known as the modified barium swallow Videofluoroscopy not only serves to confirm the presence of oropharyngeal dysfunction It can also assess the degree of aspiration Esophageal dysphagia the difficulty in propagating food down the esophagus arises within the body of the esophagus either due to a mechanical or a motility disturbance. Esophageal Disease States Achalasia Nonachalasia Motility Disorders Strictures Rings/Webs Gastroesophageal Reflux Disease Extraesophageal GERD Neoplasia Esophageal Diverticula Foreign Bodies Pill-Induced Injury Infectious Esophagitis Caustic Injury 1. Achalasia Achalasia a primary esophageal motility of unknown cause characterized by insufficient LES relaxation and loss of esophageal peristalsis hereditary, degenerative, autoimmune, and infectious factors as possible causes Pathologic changes occur in the myenteric plexus consist of a patchy inflammatory infiltrate of T lymphocytes, eosinophils, and mast cells loss of ganglion cells and myenteric neural fibrosis selective loss of post-ganglionic inhibitory neurons, nitric oxide and vasoactive intestinal polypeptide The postganglionic cholinergic neurons are spared, leading to unopposed cholinergic stimulation. This produces high basal LES pressures, and the loss of inhibitory input results in insufficient LES relaxation Aperistalsis along the esophageal body—a process mediated by nitric oxide. m/c symptoms of achalasia include ♥ dysphagia for solid & liquid ♥ regurgitation ♥ chest pain Patients with achalasia localize their dysphagia to the cervical or xiphoid areas. Initially, the dysphagia may be for solids only most patients have dysphagia for solids and liquids at time of presentation Regurgitation occurs in 75% of achalasia and becomes a greater problem as the esophagus dilates with progression of disease Choking and Coughing may awaken the patient from sleep Chest pain 40% Weight loss 60% (minimal loss) barium esophagram with fluoroscopy is the best initial diagnostic study This test will reveal a loss of primary peristalsis in the distal two thirds of the esophagus In the upright position, there will be poor emptying with retained food and saliva producing a heterogeneous air-fluid level at the top of the barium column. Achalasia The esophagus may be dilated (Figure 80- 18). esophagus is dilated with a "bird's beak" tapering of the distal esophagus Retained secretions form the heterogenous air-fluid level seen at the top of the barium column. chronic disease be massive with sigmoid-like tortuosity sigmoidlike tortuosity with large amount of retained debris. late-stage achalasia smooth tapering of the lower esophagus leading to closed LES, resembling a bird's beak presence of epiphrenie diverticulum may suggest achalasia Bird’s beak deformity at LES Esophageal manometry can be used to diagnosis In the body of the esophagus, aperistalsis is always present all swallows are typically with low contraction amplitudes. Manometry Elevated resting LES pressure (>35 mmHg ) Incomplete LES relaxation Absence of peristalsis Manometry Manometric findings in achalasia The aperistalsis is manifested by isobaric contractions without propagation The LES pressure, which is elevated, shows minimal relaxation with swallowing. Abnormal LES relaxation in all achalasia 70% - 80% of patients absent/ incomplete LES relaxation with swallows baseline LES pressure is usually elevated but may be normal in up to 45% of patients Esophagus is dilated with retained fiuid and debris. Nonrelaxation of LES Asynchronous contraction and Nonperistaltic Fibrotic and atrophic Retention and stagnation of chronic food Retention esophagitis All should upper endoseopy to exclude Pseudoaehalasia arising from a tumor at the GEJ Pseudoaehalasia may mimic with classic achalasia both clinically and manometrically suspected in older age with short duration of symptoms and more significant weight loss Therapy 1.Medical therapy 2.Pneumatic dilation of the LES 3.Surgical myotomy 4.Botulinum toxin injection The two most effective treatments graded pneumatic dilation and surgical myotomy 1.Medical therapy – Nitrates, calcium channel blockers (nifedipine) – Cause smooth muscle relaxation but with limited success 2.Pneumatic dilation of the LES -good short-term results -2% to 5% risk of perforation - performed endoscopy uses air pressure to dilate and disrupt the circular muscle fibers of the LES Balloon dilators,: three diameters (3, 3.5, and 4 cm) are positioned over a guidewire After pneumatic dilation gastrograffin study by barium swallow to exclude esophageal perforation relief of symptoms in 50% to 93% Pneumatic dilation of the LES 3.Surgical myotomy -fail repeated pneumatic dilations -an anterior myotomy across the LES (Heller's myotomy) usually associated with an antire-flux procedure -laparoscopy good-to-excellent response rate of 80% to 94% A potential complication of myotomy is GERD, which occurs in 10% to 20% 4.Botulinum toxin injection -Inhibits release of excitatory acetylcholine from nerve endings (thus causing lower LES pressures) -Good short-term results, but long term efficacy unknow -Effective in about; 85% of patients However, symptoms recur in more than 50% of patients after 6 months do not improve LES relaxation or improve peristalsis do not provide complete symptom relief The clinical response is short acting efficacy decreases with time. 2.Nonachalasia Motility Disorders Nonachalasia Motility Disorders Other described primary motility disorders of the esophagus Defined based on the presence of specific manomctrie criteria Most often noted on manometry in patients with chest pain or dysphagia 2.1 Diffuse esophageal spasm (DES) 2.2 Scleroderma or progressive systemic sclerosis (PSS) 2.3 Other systemic conditions Diffuse Esophageal Spasm Repetitive, high amplitude contractions of smooth muscle portion of the esophagus The striated portion and LES relaxation normally. Histopathology : muscular hypertrophy with lymphocytic infiltration of Auerbach’plexus S&S: dysphagia and chest pain (substernal) or esophageal colic with may occur with or without swallowing. Trigger by emotional stress, hot or cold liquids and GE reflux DES may present with chest pain if the contraction amplitudes are high dysphagia if the contraction amplitudes are low. Investigate: CXR, cardiac evaluation, barium study and manometry LES relaxation is also normal in DES The classic finding on esophagogram is the "corkscrew" esophagus Radiographic – Classic “corkscrew” – Beaklike taper – Increase in esophageal wall thickness Manometrie :simultaneous and repetitive contractions in the esophageal body but in contrast to achalasia, some normal peristalsis is maintained Typical : corkscrew pattern Manometry : prolong, high amplitude nonperistaltic Both UES and LES normal,but elevate LES pressure may be found. "Nutcracker" esophagus is another common manometrie diagnosis in noncardiac chest pain defined by high-amplitude peristalsis distal esophageal contraction amplitude less than 30 mmHg in 30% or more of wet swallows a food bolus may not be effectively transported resulting in dysphagia Treatment 1.Reassuring the disease is not heart disease. 2.Medication : nitroglycerine, calcium blocker, anticholinergic, PPI (Rx GERD) (not completely effective) 3.Surgery : – 3.1 Dilation: help only in LES dysfunction, improve dysphagia temporarily – 3.2 Surgical myotomy Scleroderma progressive systemic sclerosis (PSS) Secondary motility disorders arc commonly a result of systemic conditions The most common condition affecting esophageal motility Esophageal motor disturbances occur in several of the collagen vascular diseases – Dermatomyositis – Polymyositis – Lupus erythematosus – Scleroderma (extremely common) Characterized by : Smooth muscle atrophy and collagen deposition in the submucosa Decrease peristalsis and LES resting pressure Refulx esophagitis, ulceration, bleeding Radiography Dilate esophagus with decreased motility (unlike achalasia, persistent patent GE junction and no air fluid level) Scleroderma Endoscopy: Reflux esophagitis Other systemic conditions results in esophageal hypomotility – hypothyroidism – diabetes mellitus – amy-loidosis Investigation Esophageal manometry and intraesophageal pH readings are the most sensitive means of detection Diminished contractions in LES and distal two thirds of the esophagus Treatment Standard antireflux medicine In patients with intractable symptoms gastroesophageal reflux surgery should be considered 3.Strictures . Strictures defined as any loss of lumen area within the esophagus The normal esophagus measures 20 mm in diameter The predominant clinical symptom of strictures is dysphagia, which is usually when the lumenal diameter is less than 15 mm. Even less severe strictures can cause intermittent dysphagia to large food piece ; meat and bread There are multiple intrinsic and extrinsic causes for esophageal strictures Etiology of Esophageal Strictures Intrinsic strictures – – – – – – – – – – – – Acid peptic Pill-induced Chemical/lye Post-nasogastric tube Infectious esophagitis Sclerotherapy Radiation-induced Esophageal/gastric malignancies Surgical anastomotic Congenital Systemic inflammatory disease Epidermolysis bullosa Extrinsic strictures – Pulmonary/mediastinai malignancies – Anomalous vessels and aneurysms – Metastatic submucosal infiltration (breast cancer, mesothelioma, adenoeareinoma of gastric eardia) Intrinsic strictures are most common, with acid/ peptic cause accounting for the majority of cases (60%-70%) Strictures / Caustic Ingestion Treatment esophageal dilation. There are several different types: of dilators, including: (1) mercury-filled, rubber Maloney dilators; (2) wire-guided rigid Savary-Gilliard dilators; (3) balloon dilators that can either be through-the-scope (TT8) or wire guided Maloney bougies are used in uncomplicated, short, straight strictures The wire-guided Savary-Gilliard and TTS balloons are both best suited for long, tight, or tortuous strictures. Complications of esophageal dilation – perforation (0.5%) – bleeding (0.3%) – bacteremia (20%-50% ) Those with radiation-induced or malignant strictures are at higher risk of perforation. To minimize the risk of perforation, the "rule of. threes" applies. That is, no more than three sequential dilators should be performed per session. The goal of esophageal dilation is to obtain an objective diameter of greater than 15 mm Approximately 90% of; patients dilated to 15 mm have no recurrence at; 24 months Refractory esophageal strictures are defined by lack of response to two or more dilations. The causes, for refractory strictures can include ongoing insults from pills or nonsteroida] antiinfkunmatory drugs(NSAlDs) uncontrolled acid reflux inadequate lumen diameter with dilations PPIs are superior to H-2 blockers in preventing the recurrence of acidrelated strictures The treatment of refractory strictures includes the elimination of the offending agents (pills and acid) and gentle dilation to 15 mm. Intralesional steroids injected before dilation are safe and probably effective for refractory strictures Surgery may be considered in those who fail to respond to aggressive medical therapy and dilation. 4.Rings/Webs Rings/Webs common findings on upper endoscopy, many are asymptomatic Symptoms can include intermittent solid food dysphagia, aspiration, and regurgitation. Rings are circumferential, can consist of mucosa or muscle, and most commonly occur in the distal esophagus Esophageal webs occupy only part of the esophageal lumen, are always mucosal, and are usually located in the proximal esophagus. Esophageal webs can be found as 5% of asymptomatic individuals When symptomatic, usually dysphagia iron deficiency was noted by gastroenterologists Plummer and Vinson in the United States, as well as otolaryngologists Paterson and Kelly in the United Kingdom. Plummer-Vinson or Paterson-Kclly syndrome to the triad of proximal esophageal webs, iron deficiency anemia, and dysphagia Barium radiography is the most sensitive test to diagnose esophageal webs endoscopic visualization, web will appear as a thin, eccentric lesion with normal-appuaring mucosa Some webs are located so proximally that routine passage of the endoscope through the UES with fracture the web Treatment of symptomatic esophageal webs consists of mechanical disruption This can be accomplished with bougie or balloon dilators. Schatzki's ring (B ring) occurs at the GEJ at the distal margin of the LES most common cause of intermittent solid food dysphagia and food impaction The presence of symptoms depends on the luminal diameter If the ring diameter is less than 13 mm, the patient will have symptoms If greater than 20 mm the patient will almost never have symptoms Between 13 and 20 mm, which accounts for the majority of Sehatzki's rings, symptoms are variable The pathogenesis of esophageal rings is controversial Recurrent symptoms requiring repeat dilation is not uncommon, and some authors recommend maintaining the patient on acid suppression given the possible association with GERD The second type of esophageal ring is the A ring", which is a muscular ring most commonly detected on barium swallow This lower esophageal muscular ring rarely symptomatic and occurs at the proximal margin of the LES approximately 2 cm proximal to SGM. "Ringed" esophagus is a rare condition that occurs in young men The syndrome consists of endoscopie findings of multiple esophageal rings in patients with dysphagia The cause is unclear GERD. congenital abnormality, and possible allergic conditions have been implicated Esophageal Webs and Rings Treatment Treatment consists of dilation with bougienage and possibly acid suppression Many of these patients require more than one treatment session to obtain a desired esophageal lumen of 15 mm They are also at higher risk of painful deep mucosal tears 5. Gastroesophageal Reflux Disease Gastroesophageal Reflux Disease chronic symptoms or mucosal damage caused by the abnormal reflux of gastric contents into the esophagus. Reflux esophagitis refers to a subgroup of GERD that involves histopathologically characteristic changes in the esophageal mucosa Nonerosive reflux disease (NERD) refers to endoseopy-negative patients with typical GERD symptoms NERD accounts for approximately 50% of patients Reflux esophagitis for 30% to 40% Barrett's esophagus in the remaining 10% to 20% Barrett’s esophagus Barrett’s esophagus with ulceration Barrett’s esophagus Pathophysiology Transient relaxation of the GE sphincter Esophageal motility disorders Delayed gastric emptying Hiatal hernia Acidic gastric contents Bile acids (more severe eophagitis ) normal antireflux barrier between the stomach and the esophagus is impaired transient / permanently defects in the esophagogastric barrier such as LES incompetence, TLESR, and hiatal hernia in the development of GERD TLESRs are short relaxations of the LES that do not occur in response to swallow TLESRs are the primary mechanism for gastroesophageal reflux in healthy persons and in those with mild GERD severe GERD and related complications have a permanent structural alteration – low LES pressure – a large hiatal hernia Symptoms develop when the offensive factors in the gastroduodenal contents overcome several lines of esophageal defense As more components of esophageal defense break down, the severity of reflux increases Classic symptoms of GERD are heartburn defined as a retrosternal burning discomfort, and acid regurgitation Symptoms often occur after meals Other in typical reflux are dysphagia, odynophagia, and belching Atypical GERD symptoms include asthma, chest pain, cough, laryngitis, and dental erosions. There is no diagnostic gold .standard for detecting GERD Classic symptoms of acid regurgitation and heartburn are specific but not sensitive for the diagnosis of GERD as determined by abnormal 24-hour pH monitoring. initial empiric trial of antisecretory therapy in a patient with classic GERD symptoms Further diagnostic should be done – if there is a failure to respond to an empiric course – if alarm signs such as dysphagia, odynophagia, weight loss, chest pain, or choking are present. Atypical symptoms Atypical chest pain Globus sensation Hoarseness Onset after age 45 Nausea Recurrent laryngitis Cough Recurrent sore Odynophagia throat Subglottic stenosis Dental enamel loss Asthma Endoscopy is the technique of choice to evaluate GERD Reflux esophagitis is present when erosions or ulcerations are present at SCM There are many grading systems to characterize the severity of esophagitis, the most common of which is the Los Angeles classification The presence of esophagitis and the finding of Barrett's esophagus are diagnostic of GERD 24-hour pH monitoring has long been thought to be the gold standard for the diagnosis of GERD limitations that remain underappreciated. Results are normal in 25% of patients with erosive esophagitis and 33% of patients with nonerosive reflux disease Radiologic Finding Only 1/3 of patients have radiologic findings – Erosions – Ulcerations – Strictures – Hiatal hernia – Thickening of mucosal folds Not the test of choice for diagnosis Esophagogram Extensive linear superficial ulcerations and erosions involving the distal 1/3 of the esophagus. Endoscopy Useful for diagnosing complications of GERD – Barrett’s – Esophagitis – Strictures Not sensitive for GERD itself Only 50% of patients manifest evidence on endoscopy Gastroesophageal Reflux Disease Esophagoscopy Ambulatory pH Mornitoring Diagnostic gold standard pH monitor placed in esophagus above sphincter Patient symptom log Correlate symptoms with low pH TREATMENT Lifestyle modifications Antacids Histamine H2 receptor antagonists Prokinetic Agents Proton Pump inhibitors Anti-reflux surgery Newer endoscopic treatments LIFESTYLE MODIFICATION Head of bed elevated six inches Decreased fat intake Smoking cessation Weight loss Avoidance of recumbency for 3 hours post- prandially Avoidance of large meals and trigger foods Avoidance of exacerbating medications The goals of treatment in GERD are to – relieve symptoms – heal esophagitis – prevent recurrence of symtoms – prevent complications A variety of lifestyle modifications are recommended in the treatment off GERD. These include – avoidance of precipitating foods(fatty foods, alcohol, caffeine) – avoidance of recumbency for 3 hours postprandially – elevation of the head of the bed – smoking cessation – weight loss Histamine receptor antagonists (H2RAs) in standard doses achieve complete symptom relief in 60% of patients and heal esophagitis in bout 50% PPIs are superior to H2RAs in both healing rosive esophagitis and symptoms relief, with healing 90% GERD is a chronic relapsing disease with almost universal recurence of symptoms after treatment withdrawal requires maintenance therapy in many patients longterm therapy with PPIs is again superior to H2RAs, with remission maintained in 80% and 50% of patients, respectively "step-down" therapy is recommended Antireflux surgery, now laparoscopie approach, remains an option for carefully selected patients with well documented GERD Surgical Treatment Nissen fundoplication – Total or partial Their aim is to: – Restore normal anatomy (intra-abdominal segment of esophagus) – Re-creating an appropriate high-pressure sound at the esophagogastric junction – Maintaining this repair in the normal anatomic position 6.Extraesophageal GERD Extraesophageal GERD Patients with GERD may present with symptoms other heartburn and regurgitation This includes asthma, chest pain, chronic cough, laryngitis, and dental erosions lack of the classic heartburn and regurgitation symptoms Esophagitis/Barrett's esophagus is usually not present an empiric trial of bid PPIs is indicated as initial treatment because there is no definitive diagnostic gold standard for GERD. If treatment fails – full investigation – ambulatory pH testing Confirm diagnosis of GERD when – symptoms relieve by specific antireflux therapy Extraesophageal GERD Laryngitis Asthma Chest pain Chronic cough Dental erosions 7.Neoplasia Neoplasia uncommon when present is typically malignant. The two main culprits are – esophageal squamous cell carcinoma – esophageal adenocarcinoma. Benign Esophageal Tumors and Cysts Benign tumors are rare (< 1 %) Classified in two groups – Mucosal – Extramucosal (intramural) More useful classification: – 60% of benign neoplasms are leiomyomas – 20% are cysts – 5% are polyps – Others (< 2 percent) Leiomyomas Most common benign tumor of the esophagus Intramural Occur between 20-50 years of age with no gender preponderance 80% occur in the middle and lower third of the esophagus, rare in the cervical region Obstruction and regurgitation may occur in large lesions Bleeding is a more common symptom of the malignant form of the tumor: leiomyosarcoma Cancer Malignant Tumors of the Esophagus Usually are in advanced stages at the time of diagnosis (involving the muscular wall and extending into adjacent tissues) Alcohol consumption and cigarette smoking seem to be the most consistent risk factors Esophageal squamous cell carcinoma – Esophageal squamous cell carcinoma (95% of all esophageal cancers) is a disease of men (5: 1) – most often in the upper and midthoracic segments – least frequently in the cervical esophagus Adenocarcinoma – approximate 8% of primary esophageal cancers – Most often occur in the distal third of the esophagus in the 6th decade of life. – Male to female ratio is 3:1 – Patients with Barretts metaplasia are 40 times more likely to develop adenocarcinoma Clinical Presentation Dysphagia is the presenting complaint in 80-90% of patients with esophageal carcinoma Early symptoms are sometimes nonspecific retrosternal discomfort or indigestion As the tumor enlarges, dysphagia becomes more progressive. Later symptoms include weight loss, odynophagia, chest pain and hematemesis Diagnosis Barium swallow Esophagoscopy Esophageal biopsy Brushings for cytologic evaluation Barium Barium Cancer: apple core appearance Current AJCC 2002 staging Treatment Surgical resection is the standard treatment for early esophageal cancer in Stages I, II and most cases of III During the past decade, outcomes with surgery have improved resulting in a better 5 year survival due to: – Better staging techniques – Increased rate of curative resection – A decreased rate of postoperative death – Palliative endoscopic measures Palliative endoscopic measures include – repeated dilation, – laser/photo dynamic therapy ablation – esophageal stent placement – percutaneous gastrostomy tube placement Neoadjuvant /adjuvant therapy Neo-adjuvant Chemotherapy Neo-adjuvant Radiation Neo-adjuvant Chemo-Radiation Adjuvant Chemotherapy Adjuvant Radiation Adjuvant chemoradiation 8.Esophageal Diverticula Esophageal Diverticula is a sac that protrudes from the esophageal wall As in the rest of the Gl tract a true diverticulum is one that contains all layers of the wall. Esophageal diverticula are most practically classified, based on anatomy, into four categories: – Zenker's diverticula – midesophageal diverticula – epiphrenic diverticula – intramural pseudodiverticulosis. Zenker's divertieulum referred to as an esophageal diverticulum its location is proximal to the esophagus, above the UES, and it should be considered a hypopharyngeal diverticulum. believed to form as a result of an area of weakness Killian's triangle, which exists between the cricopharyngeal sphincter and the inferior pharyngeal constrictor muscle Zenker’s diverticulum Occurs in Killian’s area. Associated with failure of cricopharyngeal dilatation. Symptoms: regurgitation, dysphagia, weight loss. Symptoms include – oropharyngeal dysphagia – regurgitation – halitosis – cough – aspiration pneumonia Barium swallow is an excellent test Many small diverticula are asymptomatic patients with large diverticula should be offered treatment The classic treatment – open surgical resection of the diverticulum with division of the cricopharyngcus muscles Another option for extremely large diverticula – diverticulopexy – suspension of the diverticulum in a cranial direction. Midesophageal diverticula are most commonly asymptomatic, occur in the midesophagus Traction diverticuli form as a result of external pulling of the esophageal wall from neighboring inflammatory or fibrotic tissue, such as adjacent tuberculous mediastinitis Traction diverticuli are located in the middle third of the esophagus. Midesophageal traction diverticula are the only true diverticula in the esophagus Epiphrenic diverticula, located near the diaphragmatic hiatus, occur in the distal esophagus near the LES These diverticula are often the result of a motility disorder such as achalasia or DES manometric studies in patients with epiphrenic diverticulum to rule out an associated motility disorder Most diverticula are asymptomatic, but occasionally chest pain or regurgitation can be prominent symptoms Midesophageal Diverticula Epiphrenic Diverticula Treatment Treatment consists of • managing the underlying motility disorder • diverticulotomy with/without myotomy for symptomatic diverticula 9.Foreign Bodies Foreign Bodies Foreign Bodies The esophagus is one of the locations where intervention is often required Underlying alterations in the lumen of the esophagus play an important role in the risk of a swallowed object becoming lodged The esophagus has several areas of physiologic narrowing – the upper esophageal sphincter – the level of the aortic arch – the diaphragmatic hiatus/LES where a foreign body can become impacted. The key to the management of foreign bodies is understanding that different foreign bodies require different interventions It is important to distinguish a true foreign body from a food impaction. A trial of pharmacologic therapy with .1 to 2 mg of glucagon given intravenously, which relaxes the LES, can be given but is rarely successful in relieving a food' impaction. 10.Pill-Induced Injury Pill-Induced Injury Pill-induced injury to the esophagus is an underappreciated entity. over 70 drugs are capable of producing injury to the esophagus Drugs commonly associated with pill- induced injury include potassium chloride tablets, doxycycline, quuudine, NSAIDs. iron, and alendronate Pills can damage the esophagus by various mechanisms such as acidity, size, and contact time with esophageal mucosa There is a wide spectrum of injury from acute self-limited esophagitis to refractory strictures The typical sites of pill-induced injury are at the level of the aortic arch and the distal esophagus, where there is anatomic narrowing. 11.Infectious Esophagitis Infectious Esophagitis Infectious esophagitis is common, especially in immunosuppressed hosts such as patients with human immunodeficiency virus (HIV), transplant patients, and chemotherapy patients. The cardinal symptom of infectious esophagitis is – odynophagia – pain – swallowing immunodeficient patients can present with a variety of symptoms including heartburn, nausea, fever, or bleeding. The three most common causes of infectious esophagitis are – Candida albicans – cytomegalo virus (CMV) – herpes simplex virus (HSV) Treatment consists of antifungal therapy, most commonly with fluconazole100 to 200 mg/day for10 to 14 days In patients with only mild immunologic deficiencies, the topical antifungal agents clotrimazole and nystatm are reasonable alternatives 12.Caustic Injury Caustic Ingestion Esophagus, pharynx, larynx Bases ( most severe injuries ) – Drain cleaners – Electric dishwasher soap – Hair relaxant Acids Bleaches Mechanism of injury Alkalis – pH > 7 – Liquefaction necrosis Acids – pH < 7 – Coagulation necrosis Bleaches – pH = 7 – Irritants Severity of burn Type Amount Concentration Time of contact Stricture formation Signs and symptoms Pharyngeal or laryngeal – Odynophagia – Mucosal erythema, ulceration – Drooling – Tongue edema – Stridor – Hoarseness Esophageal – Dysphagia – Odynophagia – Chest or back pain Gastric – Epigastric pain or tenderness – Vomiting – Hematemesis Radiography Radiologic exam – Chest & neck radiographs Barium swallow – Will not reveal 1st and 2nd degree injuries Esophagoscopy Esophagoscopy in virtually all patients at 24-48 hours post-ingestion < 24 hours – underestimation of injury > 48-72 hours with risk of iatrogenic perforation – barium swallow Rigid vs. flexible debatable Endoscopy to upper limit of severe burn Management 1. Stable airway • dexamethasone (adult 20 to 30 mg intravenous bolus, pediatric 0.5 to 1 mg/kg) can help prevent further deterioration 2. Acute airway obstruction • Blind nasotracheal intubation should be avoided • If direct visualization of the larynx for intubation is not possible because of edema and exudate, emergent cricothyrotomy or tracheotomy is a safer choice Therapy Choice of therapy depends on the degree of injury. 1. First-degree burns of the esophageal mucosa require no further therapy 2. Second- and localized third-degree injuries without transmural necrosis: • pharmacologic reduction or prevention of stricture formation and to maintain a conduit from the hypopharynx to the stomach by esophageal dilation, stenting, or reconstruction 3. Fourth-degree and even selected extensive third-degree esophageal burns: • thoracotomy for direct examination of the esophageal wall esophagectomy Thank You