File - Dr.Rola Shadid
advertisement
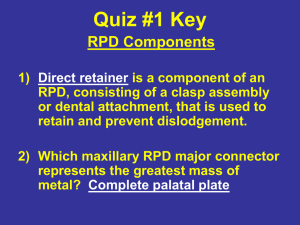
Introduction to Removable Partial Prosthodontics Rola M. Shadid, BDS, MSc Partial Denture A prosthesis that replaces one or more, but not all of the natural teeth and supporting structures. It is supported by the teeth and/or the mucosa. It may be fixed (i.e. a bridge) or removable. Removable Partial Denture (RPD) A partial denture that can be removed and replaced in the mouth by the patient. Can be interim RPD (all-resin) or definitive cast framework RPD Interim Rmovable Partial Denture (Provisional; Temporary) A denture used for a short interval of time to provide: a. esthetics, mastication, occlusal support and convenience. b. conditioning of the patient to accept the final prosthesis. Retention: Resistance to removal from the tissues or teeth Stability: Resistance to movement in a horizontal direction (anterior-posteriorly or mediolaterally Support: Resistance to movement towards the tissues or teeth Abutment: A tooth that supports a partial denture. Retainer: A component of a partial denture that provides both retention and support for the partial denture Classification of Partially Edentulous Arches Major Categories of Partial Tooth Loss Tooth- and tissuesupported space Tooth-supported space Requirements of an Acceptable Classification….. should permit immediate visualization of the type of partially edentulous arch that is being considered. should permit immediate differentiation between the tooth-supported and the tooth- and tissue-supported removable partial denture. should be universally acceptable. Classification of Partially Edentulous Arches To assist our management of partially edentulous patients Many classifications have been proposed but Kennedy classification is the most widely accepted Class II RPD Kennedy classification Was proposed by Dr. Edward Kennedy in 1925 Like Bailyn & Skinner classification, it classifies the partial edentulous arches in a manner that suggests principles of design for a given situation Kennedy classification He classified the partial edentulous arches into four basic classes The other edentulous areas that donot determine the class are considered as modification spaces Kennedy classification Class I: Bilateral edentulous areas located posterior to natural teeth Class II: A unilateral edentulous area located posterior to remaining natural teeth Class III: A unilateral edentulous area with natural teeth remaining anterior and posterior to it Class IV: A single, but bilateral (crossing the midline) edentulous area located anterior to remaining natural teeth Applegate’s Rules for Applying the Kennedy Classification Rule 1: the classification should follow, not precede extractions. Rule 2: if a 3rd molar is missing and not to be replaced, it’s not considered in the classification. Rule 3: if a 3rd molar is present and to be used as an abutment, it’s considered in the classification. Rule 4: if a 2nd molar is missing and not to be replaced, it’s not considered in the classification. Rule 5: the most posterior area always determines the classification. Rule 6: edentulous areas other then those determining the classification are referred to as modifications and are designated by their numbers. Rule 7: the extent of the modification is not considered, only the number of additional edentulous areas. Rule 8: there are no modification areas in a K Class IV. What are the Available Options to Manage This? What are the Available Options to Manage This? What are the Available Options to Manage This? Missing Teeth May Be Replaced By One of Three Prosthesis Types: * 1. An implant-supported fixed partial denture 2. A tooth-supported fixed partial denture (FPD) 3. A removable partial denture (RPD) 4. No replacement Alternatives to RPD (Treatment Options) 1. Implant-supported prosthesis – most costly, closest replacement to natural dentition, less costly over long term 2. Fixed partial denture – requires abutments at opposite ends of edentulous space, more expensive than RPD, must grind down abutments, flexes and can fail if too long 3. No treatment No Treatment If a patient presents with a long-standing edentulous space into which there has been little or no drifting or elongation of the adjacent or opposing teeth, the question of replacement should be left to the patient's wishes. If the patient perceives no functional, occlusal, or esthetic impairment, it would be a dubious service to place a prosthesis.* No Treatment (Shortened Dental Arch) Most patients can function with a shortened dental arch (SDA) RPD doesn’t usually improve function in shortened dental arch cases Shortened Dental Arch Requires anterior teeth + 4 occlusal units (symmetric loss) or 6 occlusal units (asymmetric loss) for acceptable function Opposing PM =1 unit, opposing molars = 2 units Indications of RPD A removable partial denture should be considered only when a fixed restoration (either tooth-supported or implant-supported) is contraindicated Indications of RPD * (Span Length) Edentulous spaces greater than two posterior teeth, anterior spaces greater than four incisors, or spaces that include a canine and two other contiguous teeth; i.e, central incisor, lateral incisor, and canine; lateral incisor, canine, and first premolar; or the canine and both premolars. Indications of RPD (Distal Extension Situations) An edentulous space with no distal abutment will usually require an RPD, especially when implant treatment is not feasible for the patient. * Distal Extension Situations To minimize the leverage effect, the pontic should be kept as small as possible, more nearly representing a premolar than a molar . There should be light occlusal contact with absolutely no contact in any excursion. The pontic should possess maximum occlusogingival height to ensure a rigid prosthesis. Indications of RPD (After Recent Extractions) Replacement of teeth after recent extractions often cannot be accomplished satisfactorily with a fixed restoration. When relining will be required later or when a fixed restoration using natural teeth or implants will be constructed later, a temporary RPD can be used. Indications of RPD (Abutment Alignment) Tipped teeth adjoining edentulous spaces and prospective abutments with divergent alignments may lend themselves more readily to utilization as RPD rather than FPD abutments, if implant therapy is not amenable. Indications of RPD (Need for Effect of Bilateral Stabilization) Periodontally weakened primary abutments may serve better in retaining a well designed removable partial denture than in bearing the load of a fixed partial denture. * Avoid Unilateral RPD Indications of RPD (Abutment condition) Teeth with short clinical crowns or teeth that are just generally short usually will not be good FPD abutments. Unusually sound abutment teeth Indications of RPD (Abutment Condition) An insufficient number of abutments may also be a reason for selecting a removable rather than FPD, if implant therapy is not amenable. Indications of RPD (Excessive Loss of Residual Bone) If there has been a severe loss of tissue in the edentulous ridge, an RPD can more easily be used to restore the space both functionally and esthetically. Gingival Reconstruction with FPD Indications of RPD ( Economic Considerations) Economics should not be the sole criterion in arriving at a method of treatment. When for economic reasons, complete treatment is out of the question and yet replacement of missing teeth is indicated, the restorative procedures dictated by these considerations must be described clearly to the patient as a compromise and not representative of the best that modern dentistry has to offer. * Combination of RPD and FPD Usually, any missing anterior teeth in a partially edentulous arch are best replaced by means of a fixed restoration. Then, the replacement of missing posterior teeth is made with an RPD .* Combination of RPD and FPD When an edentulous space that is a modification of either a Class I or Class II arch exists anterior to a lone-standing abutment tooth, the splinting of this abutment to the nearest tooth by FPD is mandatory. * Combination of RPD and FPD Eliminate all but one posterior edentulous space per quadrant by using an FPD to simplify the RPD design. Removable Partial Denture Dry mouth poor RPD risk Limited patient finances Acceptable oral hygiene Reliable recall candidate Treatment simplification Advanced age Systemic health problems More adaptable to dentition in transition to edentulous state Conventional Tooth-Supported FPD Dry mouth high caries risk Muscular discoordination Mandibular tori Palatal soft tissue lesions Large tongue Exaggerated gag reflex Unfavorable attitude toward RPD Patient can't cope with aging, tooth loss Favorable opposing occlusion Periodontally weakened natural dentition may permit FPD in less than optimal situations Components of a Typical RPD Major connectors Minor connectors Direct retainers Indirect retainers (if the prosthesis has distal extension bases) One or more bases, each supporting one to several replacement teeth (a) Major Connector: The unit of an RPD that connects the parts of one side of the dental arch to those of the other side. Its principal functions are to provide unification and rigidity to the denture. (b) Minor Connector: A unit of a partial denture that connects other components (i.e. direct retainer, indirect retainer, denture base, etc.) to the major connector. The principle functions of minor connectors are to provide unification and rigidity to the denture. (c) Direct Retainer: A unit of a partial denture that provides retention against dislodging forces. A direct retainer is commonly called a 'clasp' or 'clasp unit' and is composed of four elements, a rest, a retentive arm, a reciprocal arm and a minor connector. (d) Indirect Retainer: A unit of a Class I or II partial denture that prevents or resists movement or rotation of the base(s) away from the residual ridge. The indirect retainer is usually composed of one component, a rest. (e) Denture Base: The unit of a partial denture that covers the residual ridges and supports the denture teeth. References McCracken’s Removable Prosthodontics, 11th Edition 2005 by McGivney GP, Carr AB. Chapter 2 and 3 McCracken’s Removable Prosthodontics, 11th Edition 2005 by McGivney GP, Carr AB. Chapter 12 Diagnosis and Treatment Planning P 215-220