File - Dr.Rola Shadid
advertisement
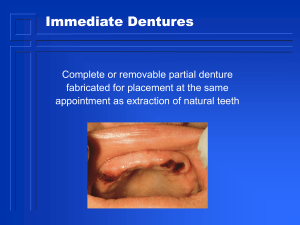
Examination, Diagnosis and Treatment Planning for Edentulous or Partially Edentulous Patients Rola M. Shadid, BDS, MSc Procedures Carried Before Denture Treatment General information Chief complaint & patient expectations Medical history & current medication Dental history Visual & manual examination of the mouth and head and neck Radiographic examination Continue Referring for additional tests or medical consultation Referring for second opinion Making alginate impressions & preparing mounted study models Discussion of diagnosis, treatment planning & prognosis with patient Finalizing the fees & obtaining a signed consent The First Meeting Most important Prior to meeting, you should review general information Your confidence is as important as the treatment itself You should be a good listener Your communication should be in a simple & truthful manner Recording General Information 1. Name 2. Race 3. Occupation 4. Address and telephone no. 5. Previous dentist Age With advancing age*: 1. Decrease capacity of tissue to tolerate stress 2. Tissue takes longer time to heal 3. Many diseases are prevalent in older age 4. Women at postmenopause may have psychological disturbances (exacting or hysterical) 5. Men at this age may be concerned with only comfort & function (indifferent) Psychological Evaluation (House Classification of Denture Patients) Philosophical patient: well motivated, cooperative, calm & composed even in difficult cases. Exacting (critical): likes each step in detail, makes alternative treatment for dentist, makes severe demands.* Continue Indifferent: not very interested in treatment, blames the dentist for any mishap, not follow instructions, been coerced to come by friend, relative….* Continue Hysterical: easily excited, highly apprehensive, unrealistic expectations* Skeptical: bad results from previous treatment, doubtful, often have severely resorbed ridges and poor health, might have psychological disturbances from recent personal trajedy # Chief Complaint & Patient Expectations Patient’s own words Why he is seeking prosthodontic treatment You should assess if patient expectations are realistic or not If not realistic, you should educate pt and scale them down Medical History* Diabetes Mellitus Cardiovascular diseases Diseases of joints: osteoarthritis Diseases of skin: pemphigus ? Neurological disorders (Bells balsy and Parkinson) Sjogren’s syndrome Transmissible diseases Radiation Therapy Vs. Dentures Consequences of Radiation therapy Preprosthetic surgery Wearing of previous denture * Denture Fabrication # Denture Fabrication in Radiation Therapy Patient Avoid impression material that dry tissue (impression plaster) or heavily flavored materials (ZOE) Consider non-anatomic teeth Teeth set in neutral zone Slight reduction in vertical dimension Soft liners are controversial due to porosity and possibility of candida Current Medication Insulin * Anticoagulants Antihypertensive: dryness & postural hypotension Corticosteroids: dryness, confusion & behavioral changes Antiparkinson agents like Norflex and Akineton: dryness, confusion & behavioral changes Dental History History of tooth loss: cause, time* Edentulous period Beware of Patients Who Have A “Bag of Dentures” * Extraoral Examination General appearance (healthy, signs of proper nourishment?) Facial symmetry Skin: color, deep wrinkles Palpation of the head & neck (lymph nodes & muscles) Extraoral Examination Muscle tonus Neuromuscular coordination* TMJ examination Classification of Frontal Face Forms (House, Frush & Fisher) * Classification of Lateral Face Forms Normal Retrognathic prognathic Lips Length* Thickness Mobility Smile line Lip (smile) line * High smile line Normal smile line Intraoral Examination Cheeks, tongue, floor of the mouth (FOM), maxillary tuberosity, hard palate, soft palate, arch relationship, residual ridge form, saliva, undercuts Cheeks Draping of the cheeks over the buccal flanges essential for peripheral seal Opening of Stenson’s duct Location for many lesions (lichen planus, submucosal fibrosis, leukoplakai, malignancies as sqauamous cell carcinoma (SCC)) Leukoplakia The Tongue Favorable tongue is average sized, moves freely, covered by healthy mucosa Normally, it should rest in a relaxed position on lingual flanges, this will retain denture & contributes to denture stability by controlling it during speech, mastication & swallowing. Tongue Size Normal Large * How to Manage Large Tongue? 1. 2. 3. 4. 5. Lower the occlusal plane Use narrower teeth Increase the intermolar distance Grind off the lingual cusps Avoid setting a second molar Tongue Position Normal: normal size and function. Lateral borders rest at level of mandibular occlusal plane while dorsum is raised above it. Apex rests at or slightly below the incisal edges of mandibular anteriors Tongue Position Retruded tongue position deprives pt of border seal of lingual flange in sublingual crescent and also may produce dislodging forces on distal regions of lingual flange Tongue Mucosa The specialized mucosa covering the tongue is said to be a “window” on systemic diseases. * Frenal Attachments Fold of mucosa found at different locations in the sulcus region of upper & lower ridge Classification Class I: sulcal or low attachment Class II: midway betw. sulcus & crest of ridge Class III: crestal attachment (frenectomy) Floor of the Mouth If FOM is near the level of the ridge crest, retention & stability of denture is less. Hyperactive FOM reduces retention & stability If great ridge resorption, FOM in sublingual and mylohyoid regions spills on the ridge Patency of submandibular ducts * Maxillary Tuberosity* If enlarged: the posterior occlusal plane may be placed too low no enough space to set all molars Maxillary Tuberosity Palpate for undercuts if extreme, denture might not seat The Hard Palate Class I: U shaped, most favorable for retention & stability Class II : V shaped: Not very favorable* Class III: Flat or shallow vault: Not very favorable, accompanied by resorbed ridges, poor resistance to lateral forces V-shaped hard palate Tori * Palatal torus Mandibular tori Bony Prominences Midpalatal raphe Sharp ridge crest Sharp mylohyoid ridge Prominent genial tubercles Bony fragments & fractured root pieces Tori The Soft Palate (Palatal Throat Form) House’s classification * Class I: the soft palate is almost horizontal curving gently downwards Class II: the soft palate turns downward at about 45 angle from the hard palte Class III: the palate turns downward sharply at about 70 angle to the hard palate. Palatal Throat Form Maxilla I II III Undercuts The contour of a cross section of a residual ridge that would prevent the placement of a denture or other prosthesis Undercuts Unilateral or bilateral; labial or lingual; mild, moderate or severe Common locations: a) b) c) d) Labial portion of maxillary anterior ridge Buccal to maxillary tuberosity Retromylohyoid area of residual ridge Labial or lingual slopes of mandibular anterior ridge Undercuts Management 1. Isolated anterior undercut- not present any problem 2. Unilateral posterior undercut- may not present much of a problem as path of insertion is varied 3. Bilateral undercut-surgical removal of the more severe one is indicated Residual Alveolar Ridge Arch form (House’s classification) Class I: square Class II: tapered (V-shaped), associated with high arched palate, less retention & stability Class III: ovoid (less common) Residual Alveolar Ridge (Cross Sectional Contour) * a. b. c. d. e. f. U shaped V shaped Knife edged Flat Inverted Undercut Soft Tissue Support of the Ridge Firm & resilient Flappy and hypermobile: poor support because denture base shifts during masticatory function Management of flappy ridge ranges from modified impression techniques to surgery Anterior Arch Relationships * Intraoral Examination Posterior arch relationships Interridge space Residual ridge size Saliva * Consistency: Thin serous: provides an insufficient film for denture retention. Thick mucus: thick ropy saliva tends to displace denture. Mixed Amount: Normal: ideal for denture retention Excessive: make denture const. messy Reduced: reduced retention and increased soreness; salivary substitutes may be prescribed Drugs Causing Xerostomia * Diuretics Antihistamines Atropine Anticholinergic Antihypertensive Antiparkinson (Norflex) Corticosteroids Examination of an Old Denture Wearer o Esthetics, lip fullness, symmetry, amount of display during smiling, phonetics, teeth position, size, excessive wear o Fracture, cracks, porosity, denture hygiene o Occlusal vertical dimension (due to excessive occlusal wear, OVD may have reduced) Reduced vertical dimension Examination of an Old Denture Wearer Epulis fissuratum Angular cheilitis Papillary hyperplasia Flappy hyperplastic ridge* Combination syndrome Epulis Fissuratum Inflammatory Papillary Hyperplasia Angular Cheilitis (Perleche) Combination (Kelly’s) Syndrome * Radiographic Examination A routine radiographic exam. must be ordered to rule out any bony conditions that could affect the treatment Panomaric radiograph is usually ordered for denture cases Radiographic Examination Fractured roots or roots lying close to the surface should be removed if pt is fit for surgery; deep seated retained teeth or root fragments may be left if they are asymptomatic Supplemental radiographs may be prescribed if required such as periapical, occlusal, and lateral cephalometric Panoramic Radiograph Additional Tests & Medical Consultation Routine blood test, blood & urine sugar levels Medical consultation Dental consultation Diagnosis A specific evaluation of existing conditions Involves thorough examination of all factors which are bound to affect the success of treatment This includes both systemic & local factors & the mental condition of the patient Treatment Plan The sequence of procedures planned for the treatment of a patient following diagnosis Explained to the patient in a simple and straightforward manner including all of the factors that might complicate the treatment Alternate Treatment Plan May be less than ideal but is often necessary for various reasons Refusal of Treatment The patient’s demand may be unreasonable or against professional judgment or ethics; so may refuse treatment or refer him (“bag of dentures”) Prognosis A forecast to the probable result of a disease or a course of therapy After considering all the factors, you should be able to predict the degree of success that can be expected & the patient should know of what can and cannot be achieved. Fees & Signed Consent When patient agreed on treatment including fees , he must sign a written consent to prevent later misunderstanding Prescription, Nutritional Supplements, & Tissue Conditioning Assess if nutritional deficiency Recommend finger massage of oral tissues If old denture wearer, tissue conditioner placed to condition abused soft tissue Instruct patient to discontinue wearing denture 48 hrs prior making final impression A good clinician is one who is able to diagnose potential problems during the initial examination & suggest the best possible treatment plan compatible with the age, physical, mental & financial status of the patient References I. Complete Denture Prosthodontics, 1st Edition, 2006 by John Joy Manappallil, Chapter 2. II. Zarb. Prosthodontic Treatment for Edentulous Patients, 12th edition. Chapter 7.