RBCs and Bleeding Disorders
advertisement

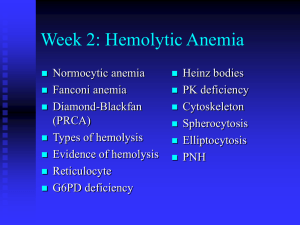
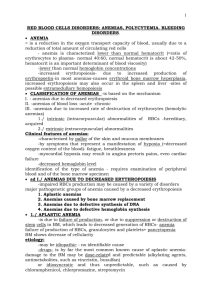
RBCs and Bleeding Disorders Anemias Anemias of blood loss – Acute blood loss – Chronic blood loss Hemolytic anemias – Hereditary spherocytosis (HS) – Hemolytic disease due to red cell enzyme defects: Glucose-6-phosphate dehydrogenase deficiency – Sickle cell disease – Thalassemia syndromes – Paroxysmal nocturnal hemoglobinuria – Immunohemolytic anemia – Hemolytic anemia resulting from trauma to red cells – cardiac valve prostheses, microangiopathic disorders Anemias of diminished erythropoiesis Anemias Anemia = A reduction of the total circulating red cell mass below normal limits, reduces the oxygen-carrying capacity of the blood, leading to tissues hypoxia In practice, usually diagnosed based on a reduction in H/H, correlate with RBC mass, except when changes in plasma volume caused by fluid retention or dehydration RBC indices, Table 14-2, adult reference ranges Clinical – pale, weakness, malaise, fatigue, DOE Anemia of Blood Loss Acute blood loss – mainly effects due to loss of intravascular volume Significant bleeding – predictable changes in the blood involving WBCs and platelets as well as RBCs Chronic blood loss – anemia only if rate of loss exceeds the regenerative capacity of the marrow or iron stores are depleted Hemolytic Anemias Premature destruction of red cells and a shortened red cell life span below the normal 120 days Elevated erythropoietin levels and a compensatory increase in erythropoiesis Accumulation of hemoglobin degradation products released by red cell breakdown derived from hemoglobin Hemolytic Anemias Extravascular hemolysis – Premature destruction also occurs in phagocytes – Hyperplasia of phagocytes leading to splenomegaly – Generally caused by alterations in RBCs that make them less deformable – Principal clinical features – anemia, splenomegaly, jaundice, often benefit from splenectomy, decreased haptoglobin Hemolytic Anemias Intravascular hemolysis – Caused by mechanical injury, complement fixation, intracellular parasites, or exogenous toxic factors – Clinical – anemia, hemoglobinemia, hemoglobinuria, hemosiderinuria, jaundice, no splenomegaly Hereditary Spherocytosis Intrinsic defects in the red cell membrane skeleton that render red cells, spheroid, less deformable, and vulnerable to splenic sequestration and destruction Diverse mutations lead to an insufficiency of membrane skeletal components Compound heterozygosity Deficiency of membrane skeleton reduces the stability of the lipid bilayer, leading to the loss of membrane fragments as red cells age in circulation Hereditary Spherocytosis Spleen has a cardinal role in the premature demise of spherocytes, trapped in splenic cords and phagocytized, erthyrostasis leading to decreased glucose and pH Increased MCHC due to dehydration because of loss of K+ and H2O Anemia, Splenomegaly, jaundice, gall stones, aplastic crises, hemolytic crises, splenectomy is beneficial Glucose-6-phosphate Dehydrogenase Deficiency Abnormalities in the hexose monophosphate shunt or glutathione metabolism resulting from deficient or impaired enzyme function reduce the ability of red cells to protect themselves from oxidative injuries and leads to hemolysis G6PD deficiency is a recessive X-linked trait, G6PD- and G6PD Mediterranean cause most of clinically significant anemias Episodic hemolysis is characteristic caused by exposures that generate oxidant stress, infections, drugs, foods (e.g. fava beans, antimalarials) G6PD Deficiency Heinz bodies removed by spleen , bite cells in peripheral smear Both intravascular and extravascular hemolysis Anemia, hemoglobinemia, hemoglobinuria Self-limited usually Sickle Cell disease Common hereditary hemoglobinopathy that occurs primarily in individuals of African descent, 8-10% of African Americans have HbS trait (heterozygotes) Point mutation in the 6th codon of Betaglobin that leads to replacement of glutamate with valine leading to the HbS molecule undergoing polymerization when deoxygenated, sickle shape Sickle Cell Disease Chronic hemolysis, microvascular occlusions, tissue damage Variables affecting the rate and degree of sickling – Interaction of HbS with other types of hemoglobin in the cell – MCHC – Intracellular pH – Transit time of red cells through the microvascular beds Sickle Cell Disease Peripheral blood – variable numbers of irreversibly sickled cells, reticulocytosis, target cell, Howell-Jolly bodies, pigment gallstones, hyperbilirubinemia, autosplenectomy, infarctions in many tissues Sickle Cell Disease Increased susceptibility to infections Crises – Vaso-oclusive =pain crises – Acute chest syndrome – Sequestration crises – Aplastic crises Thalassemia Syndromes Heterogenous group of disorders caused by inherited mutations that decrease the synthesis of adult hemoglobin, HbA Alpha-globin genes on chromosome 16 Beta-globin gene on chromosome 11 Table 14-3 – clinical and genetic classification of thalassemias Beta-Thalassemias Mutations that diminish the synthesis of beta-globin chains – Beta0 mutations – absent beta-globin synthesis Chain terminator mutations – Beta+ mutations – reduced beta-globin synthesis Splicing mutations Promoter region mutations Beta-Thalassemias Two mechanisms leading to anemia – Hypochromic, microcytic anemia with decreased oxygen transport capacity – Diminished survival of red cells and precursors Membrane damage Ineffective erythropoiesis Extravascular hemolysis Extramedullary hematopoiesis Excessive absorption of iron Beta-Thalassemias Clinical syndromes – Beta-thalassemia major – Beta-thalassemia minor or trait – Beta-thalassemia intermedia Alpha-Thalassemias Inherited deletions that result in reduced or absent synthesis of alpha-globin chains Clinical syndromes – determined and classified by the number of alpha-globin genes that are deleted – Silent carrier – deletion of one gene – Alpha-thalassemia trait – deletion of two genes – Hemoglobin H disease – deletion of three genes – Hydrops fetalis – deletion of all four genes Paroxysmal Nocturnal Hemoglobinuria Acquired mutations in the phosphatidylinositol glycan complementation group A gene ( PIGA), an enzyme that is essential for the synthesis of certain cell surface proteins Intravascular hemolysis caused by the C5b-C9 membrane attack complex Thrombosis is the leading cause of diseaserelated death because of dysfunction of platelets 5-10% develop AML or myelodysplastic syndromes Immunohemolytic Anemia Caused by antibodies that bind to red cells, leading to their premature destruction Direct Coombs antiglobulin test Indirect Coombs antiglobulin test Table 14-4 Classification – Warm Antibody type – Cold agglutinin type – Cold hemolysin type Anemias of Diminshed Erythropoiesis Megaloblastic anemias Iron deficiency anemia Anemia of chronic disease Aplastic anemia Pure red cell aplasia Other forms of marrow failure Megaloblastic Anemias Caused by an impairment of DNA synthesis that leads to distinctive morphologic changes, including abnormally large erythroid precursors and red cells Table 14-5 Causes of megaloblastic anemias Macrocytic oval cells, hypersegmented neutrophils, giant metamyelocytes and band forms Vitamin B12 Deficiency Pernicious anemia – Autoimmune gastritis leading to failure of intrinsic factor production leading to vitamin B12 deficiency – Atrophy of the fundic glands, intestinalization, atrophic glossitis, CNS – demyelination of the dorsal and lateral tracts leading to spastic paraparesis, sensory ataxia, severe paresthesias in the lower limbs Folate Deficiency Three major causes – Decreased intake – chronic alcoholics, elderly, indigent – Increased requirements – pregnancy, infancy – Impaired utilization – folic acid antagonists Iron Deficiency anemia Most common nutritional disorder in the world Iron in the body is recycled extensively between the functional and storage pools – Transferrin – Ferritin Iron balance is maintained largely by regulating the absorption of dietary iron in the proximal duodenum, hepcidin Iron Deficiency Causes – Dietary lack Infants, impoverished,elderly, teenagers – Impaired absorption – Increased requirements – Chronic blood loss-most common cause in the Western world – GI bleed until proven otherwise Iron Deficiency Hypochromic, microcytic anemia Low serum iron and ferritin Elevated TIBC Disappearance of stainable iron in the macrophages of the bone marrow Anemia of Chronic Disease Chronic microbial infections, such as osteomyelitis, endocarditis, lung abscess Chronic immune disorders, such as RA Neoplasms, lung and breast, non-Hodgkin lymphomas Iron sequestration Increase iron in marrow macrophages, high ferritin, decreased TIBC Aplastic Anemias Chronic primary hematopoietic failure and attendant pancytopenia Major causes – table 14-7 Most common known etiology drugs and chemicals also infections, whole body irradiation, Fanconi anemia Pure red cell aplasia Other forms – myelophthisic anemia, chronic renal failure, hepatocellular liver disease, endocrine disorders ( hypothyroidism) Polycythemias Table 14-8 Bleeding Disorders Increased fragility of the vessels Platelet deficiency or dysfunction Derangement of coagulation Laboratory Screening Tests in Selected Hemorrhagic Disorders Disorder Bleeding time Platelet Count PT PTT Thrombin Time Fibrinogen Assay Vascular Bleeding Usually prolonged Normal Normal Normal Normal Thrombocytopenia Prolonged Decreased Normal Normal Normal Qualitative Platelet Defects Prolonged Normal Normal Normal Normal Platelet Aggregation/sp ecial studies Classic Hemophilia Normal Normal Normal Prolonged Normal Factor VIII Assay Christmas Disease Normal Normal Normal Normal Factor IX Assay Von Willebrand Disease Prolonged Normal Normal Prolonged Normal vWF assay DIC Prolonged Decreased Prolonged Prolonged Prolonged Fibrin and FDP Prolonged Confirmatory Testing Coagulation Cascade PTT PT Coagulation Cascade www.hopkinsmedicine.org/hematology/coag ulation.swf Bleeding Disorders: Hemorrhagic Diatheses Bleeding disorders caused by vessel wall abnormalities Bleeding related to platelet number: thrombocytopenia – Chronic immune thrombocytopenia purpura – Acute immune thrombocytopenia purpura – Drug-induced thrombocytopenia – HIV-associated thrombocytopenia – Thrombotic microangiopathies Thrombotic thrombocytopenic purpura (TTP) and hemolytic uremia syndrome (HUS) Bleeding disorders related to defective platelet functions Hemorrhagic Diatheses related to abnormalities in clotting factors – The factor VIII-vWF complex – Von Willebrand disease – Hemophilia A (factor VIII deficiency) – Hemophilia B (Christmas disease, Factor IX deficiency Disseminated intravascular coagulation Vessel Wall Abnormalities Infections (e.g. meningococcemia) Drug reactions Scurvy, Ehlers-Danlos, Cushing HSP Hereditary hemorrhagic telangiestasia (Weber-Osler-Rendu) Perivascular amyloidosis Thrombocytopenia Count <20,000 = spontaneous bleeding Decreased production = bone marrow issue Decreased platelet survival = immunologic or nonimmunologic Sequestration = hypersplenism Dilution = transfusions Table 14-9 Causes of Thrombocytopenia Chronic Immune Thrombocytopenic Purpura ( ITP) Cause – autoantibodies to platelets act as opsonins, primary (diagnosis of exclusion) or secondary ( e.g SLE, HIV, B-cell neoplasms) Spenectomy helps – site of removal of opsonized platelets, site of plasma cells that produce autoantibodies Megakaryocytes – increased number and size in marrow Most common – women over 40 years of age, petechiae, echymoses, risk of intracranial bleeds Other Causes of Thrombocytopenia Acute ITP – children, following a viral illness, usually self-limited Drug-induced – heparin-induced (HIT)severe form – thrombosis, even in setting of low platelets HIV-associated – megakarocytes infected Thrombotic Microangiopathies Caused by insults that lead to excessive activation of platelets, which deposit as thrombi in microcirculatory beds – microangiopathic hemolytic anemia, organ dysfunction, thrombocytopenia – Table 14-10 Thrombotic thrombocytopenic purpura (TTP) Hemolytic-uremic syndrome (HUS) Defective Platelet Dysfunctions Defects of adhesion – Bernard-Soulier syndrome – inherited deficiency of platelet membrane glycoprotein complex (receptor for vWF) Defective platelet aggregation – Glanzmann thrombasthenia – AR - deficiency or dysfunction of glycoprotein Iib-IIIa (integrin that participates in “bridge formation” between platelets) Defects of platelet secretion – storage pool disorders Acquired – aspirin and other NSAIDs, uremia Abnormalities in Clotting Factors Most commonly manifest as large posttraumatic ecchymoses or hematomas or prolonged bleeding after a laceration or surgical procedure Hereditary – usually single clotting factor Acquired – usually multiple factors simultaneously (e.g. vitamin K deficiency) Von Willebrand Disease Most common inherited bleeding disorder of humans ( 1% of adults in US) 20 variants Type 1 and Type 3 are associated with a reduced quantity of circulating vWF Type 2 is characterized by qualitative defects in vWF Defects in platelet function despite a normal platelet count leading to secondary abnormalties in platelet adhesion and clot formation Clinically – Epistaxis, excessive bleeding from wounds, menorrhagia Hemophilia A (Factor VIII Deficiency) Most common hereditary disease associated with life-threatening bleeding X-linked recessive Clinical severity correlates well with level of factor VIII activity Petechiae are characteristically absent Prolonged PTT, normal PT Hemophilia B (Christmas Disease, Factor IX Deficiency) Clinically indistinguishable from hemophilia A – factors VIII and IX function together to activate factor X Disseminated Intravascular Coagulation (DIC) Acute, subacute, or chronic thrombohemorrhagic disorder characterized by the excessive activation of coagulation, which leads to the formation of thrombi in the microvasculature of the body Consumption of platelets, fibrin, and coagulation factors and activation of fibrinolysis Not a primary disease DIC Two major mechanisms trigger DIC - Table 14-27 – Release of tissue factor or thromboplastic substances into the circulation – Widespread injury to endothelial cells Most likely associated with: – Obstetric complications – Malignant neoplasms – Sepsis – Major trauma Possible consequences – Widespread deposition of fibrin – ischemia, microangiopathic hemolytic anemia – Hemorrhagic diathesis Clinical Features – Microangiopathic hemolytic anemia – Dyspnea, cyanosis, respiratory failure – Convulsions and coma – Oliguria and renal failure – Shock – Only definitive treatment is to remove or treat the inciting cause