6 - American Academy of Pediatrics
advertisement
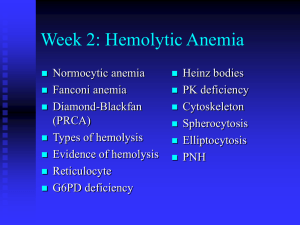
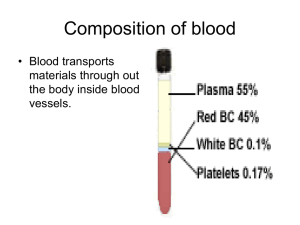
Pediatric Board Review Course Pediatric Hematology/Oncology Kusum Viswanathan, MD Chair, Department of Pediatrics Director, Divn of Pediatric Hematology/Oncology Brookdale Univ Hospital and Medical Center Question 6 week old term infant referred for anemia. Hb 7.5, Retic 2 %. Mother O+, Baby A -, Direct Coombs + Cord blood Hb 14.2 g/dL. Jaundice of 15mg/dL at 48 hours of life, recd photo Rx and discharged at 5 days. No complaints, pale, Bili 3.5, Direct 0.5. Blood smear shows spherocytes Most likely explanation for the anemia 1. G 6 PD deficiency 2. Hereditary He r y m ol y tic di se ib ilt pa t Rh he in O AB 0% as e 0% co m ca ne m ia 0% lo gi sp he r oc yt os is 0% Ph ys io ed it a ry 6 PD de fic i en cy 0% G spherocytosis 3. Physiologic anemia 4. ABO incompatibilty 5. Rh hemolytic disease 6 Newborn –anemia- important Hemoglobin at birth is 17 g/dl, MCV over 100. Falls to 11-12 by 6 weeks of age- nadir of physiologic anemia Anemia at birth could be : – Hemorrhage, may not have had time to mount a retic response – Acute hemorrhage- pallor and tachypnea – Look at MCV- low MCV-suggestive of chronic feto-maternal hemorrhage Alpha Thalassemia trait. – Kleihauer-Betke- Hb F resistance to acid elution The treatment of choice for alloimune neonatal thrombocytopenia is 1. random platelet pl a te le ts n 0% at er na l tra m ge W as he d Ex ch an 0% ns fu sio oi ds 0% St er IV IG n ns fu sio 0% tra et el 5. 0% pl at 4. nd om 3. ra 2. transfusion IVIG Steroids Exchange transfusion Washed maternal platelets 6 Immune thrombocytopenia Auto-immune: Pregnant women with ITP/Hx of ITP – – – – Passive transfer of antibodies (IgG) from mother. Even when mother has a normal platelet count (Splenectomy) Nadir-few days; Platelets < 50,00 have 1% risk of ICH. IVIG to mother, Fetal platelet counts, C sec, US, IVGG to baby Allo or Iso-Immune: Normal platelet count in mother – – – – – – – Similar to Rh disease; PL A1 antigen/ Zw-a negative mother. 97% of population is PL A1 positive Sensitization early in pregnancy Plt function defect because Anti-PL-A1 interferes w/aggregation. Severe bleeding more likely; first born affected Recovery in 2-3 weeks Mother’s washed (PLA1 neg) platelets; IVIG; Ultrasound; Steroids Kasabach- Merritt, TAR 15 months old girl presented in ER with h/o URI, and scattered petechiae and ecchymoses over the body and lower extremities. Physical exam normal, no hepatosplenomegaly. WBC-14,000, Hb 12.8, Plts-5,000, Diff: Normal - Next step nj ur y; s 0% Ad m in tre at m en tw ith ta li 0% ei th er IV ist I .. er . pl at el et tra ns . .. 0% k. .. ... ro w ac c id en em ar No n- bo n a 4. m 3. 0% rfo r 2. perform a bone marrow aspirate to confirm the diagnosis Non-accidental injury; skeletal survey to rule out bony fractures treatment with either IVIG or anti-D Administer platelet transfusion pe 1. 6 Acute ITP Usually acute onset; immune mediated; post viral Peak 2-5 years of age, PE –no lymphadenopathy (LN), hepatosplenomegaly. CBC- other cell lines normal, large plts on smear Treat if plt< 10,000 or wet ITP, Treat- IVIG best response, 48-72 hours; blocks Fc receptors,SE – Anti-D (WInRho)- Rh+ ,hemolysis, quick response – Steroids good response, block phagocytosis, reduces antibodies, SE, inexpensive, need BM BM- Increased megakaryocytes, otherwise normal Chronic- If >6 months, F>M, older, unpredictable prognosis Petechiae, HSP A 2 year old boy presents for evaluation of a chronic pruritic eruption. H/o recurrent epistaxis, otitis media, and pneumonia P/E reveals erythematous, slightly scaling patches on the trunk and in the antecubital and popliteal fossae. Petechiae too- most suggestive of isk ot t- om sy nd r Al dr ic h cy t at it i lh is t io W 0% e 0% os is s 0% m de r rh an ng e La te ia At ax At op ic lan gie ct a ... op a nt er se at it i m de r Ac ro 0% sia 0% sc el 1. Acrodermatitis enteropathica 2. Ataxia telangiectasia 3. Atopic dermatitis 4. Langerhans cell histiocytosis 5. Wiskott-Aldrich syndrome 6 Large platelets Normal platelet 7-10 days Large platelets: – ITP – May Hegglin (Dohle bodies in neutrophils, Plt function normal). – Bernard Soulier syndrome (AR, Plat function disorder). Small platelets: Wiskott Aldrich syndrome ( X-linked, recurrent infections, eczematoid rash, platelet dysfunction) Platelet function defects Normal platelet number Abnormal aggregation – Glanzmann thrombasthenia--- AR, Bleeding disorder, check h/o consanguinity – afibrinogenemia Abnormal adhesion- Bernard-Soulier, VWD Ineffective Thrombopoiesis – MayHegglin Anomaly (Large platelets) Disorders of Secretion: Storage pool, gray platelet syndrome Hermansky Pudlak Syndrome: – AR, Decreased dense granules, In Puerto Ricans – Oculocutaneous albinism Thrombocytosis H- Hemorrhage, Hereditary Asplenia, Down myeloprol. IPLATELETS- Infections, Kawasaki, Immune:GVH, Nephrotic syndrome Polycythemia vera, Myeloproliferative, Essential Leukemia (CML) Anemia,- Iron, Vit E deficiency, Sideroblastic Tumors Epinephrine, Steroids Lymphoma, Hodgkins Exercise Trauma, Fractures Splenectomy Anemia An 18 month old girl brought in for pallor. Normal diet and PMH. She is alert, interactive, only pallor, normal vital signs, No hepatosplenomegaly, lymph nodes or bruises. CBC- Normal WBC, Plt, Hb 4.5g/dl, MCV 74, Anemia – Reduced production – Increased destruction – Loss What else do you want?? Reticulocyte count Normal/Low- reduced production – Iron deficiency anemia- MCV will be low – ALL (leukemia)- other findings, LN, HSM – Diamond Blackfan anemia– TEC: Over 1 year of age, Pallor, transient rbc production failure, recovers, MCV and Hb F high during recovery, rbc transfusion, rbc ADA normal . Normal smear A 2 month old girl with a history of ventricular septal defect and horseshoe kidney presents for a health maintenance visit. Her parents are concerned that she is not feeding well, appearing to become “tired” soon after beginning to breastfeed. She is tachycardic and appears pale. Her hemoglobin level is 3.8 g/dL. Peripheral smear reveals macrocytic red blood cells. The bone marrow aspirate shows normal cellularity of the marrow with markedly decreased erythroid precursors. Which of the following findings is most likely to be identified during additional physical examination of this patient? 1. Multiple superficial hemangiomas 2. Cutis aplasia 3. Bifid thumbs 4. Speckled white rings in the periphery of the iris 5. Posterior parietal hair whorl Microcytic anemia is a characteristic laboratory abnormality of all listed diseases except ala Th Si ck l e ce l ss em ia t ld is e ra in g so n po i ad Le 0% it 0% as e 0% cy 0% en 4. de fic i 3. n 2. Iron deficiency Lead poisoning Sickle cell disease Thalassemia trait Iro 1. 6 Microcytic anemia Question A blood smear taken from a toddler shows microcytic hypochromic anemia. Iron supplementation therapy is started. When will the reticulocyte response be at maximum? a. 1-2 days b. 5-7 days c. 14-21 days d. 3-4 weeks e. about 6 weeks Iron deficiency questions Low MCV, low MCHC, low retic, RDW can be normal, Low Iron, Incr TIBC, Transferrin low, Ferritin low Causes: Inadequate dietary intake – Toddlers, too much milk, less solids, Breast fed need iron supplements – Blood loss: Menstrual, GI tract, Meckels, Epistaxis D/D: Thalassemia trait- MCV much lower in prop to anemia Anemia of chronic disease- low Fe, low TIBC, normal /high Ferritin. Question- Beta Thalassemia 3 year old comes for a routine check and found to be anemic. P/E Normal. CBC Hb 8.9, MCV 58, Iron levels are normal. Hemoglobin electrophoresis is done and shows Beta Thalassemia trait. All are true except: 1. The MCV is always low 2. Fetal hemoglobin is < 2% 3. Hemoglobin A 2 is > 3.5% 4. Does not respond to Iron 5. RDW is usually normal Beta Thalassemia Minor Quantitative defect in globin chains – Reduced production of Beta chains Hb electrophoresis – Hb A- 2 Alpha, 2 Beta – Hb F- 2 Alpha, 2 Gamma – Hb A2- 2 Alpha, 2 Delta Excess Alpha combines with Gamma or DeltaIncreased Hb F and A2. Smear abnormalities significant even with MILD anemia. Anemia Low MCV, normal RDW, normal retic Smear shows aniso and poikulocytosis, target cells, microcytes, misshapen cells, basophilic stippling Hb Electrophoresis: Increased Hb A2 and/or F. Normal iron studies, no response to iron Beta Thalassemia Major No production of Beta chains- Chromosome 11 Autosomal recessive 25 % chance with each pregnancy Pre-natal testing for carriers Chorionic villous sampling for diagnosis Transfusion dependent-allows for normal development Pen Prophylaxis, Anti oxidants Splenectomy after age 5 Iron overload- inherent and transfusion Need chelators Question 4 year old male with no complaints. Routine CBC showed a Hb9.8, MCV 62, RDW 12.5 , Retic 0.2%, Normal Iron studies, Hemoglobin electrophoresis was normal with normal Hb A2 and Hb F. You suspect Alpha Thalassemia. All of the statements are true except: 1. 2. 3. 4. 5. It is carried on 4 alleles The severe form is Hydrops fetalis Hemoglobin H disease occurs when 3 alleles are affected Diagnosed by newborn screening when a “fast moving” hemoglobin is noted. Fast moving hemoglobin is made up of a hemoglobin with 4 beta chains Thalassemia- Alpha Reduced Alpha chains 4 types- carried on 4 allelles. (xx/xx) One absent- Silent carrier (x-/xx) 2 absent- Alpha Thal trait (xx/- - or x-/x-) 3 absent- Hb H disease (x-/- -) Has 4 excess Beta chains) 4 absent- Hydrops fetalis (- -/- -) NB period: Excess Gamma chains form Hb Barts- FAST moving Hb on Newborn screening Case 3 year old patient is brought to the ER with complaints of feeling very tired over the past 3 days. Patient is pale, jaundiced with the spleen tip palpable. CBC Hb 5, Retic 5 %, LDH Increased, What does this sound like?? Question A previously well African-American child visited Africa and was given malarial prophylaxis. He experienced pallor, fatigue, and dark urine. His hemoglobin level decreased from 14.8 to 9 g/dL. SMEAR An African-Am child visited Africa & received malaria prophylaxis. He has en cy 0% de fic i at it i s 0% G6 PD Si ck l e ce ll oc yt os is sp he r ry ed it a He r 0% di se as e 0% He p 1. Hereditary spherocytosis 2. Sickle cell disease 3. Hepatitis 4. G6PD deficiency 6 Reticulocyte count- Increased Hemolysis – IntrinsicMembrane defects-Hereditary spherocytosis (HS) Enzyme-G 6 PD deficiency Hemoglobinopathies – Extrinsic- AIHA (Auto-immune hemolytic anemia), DIC, Intravascular hemolysis Loss – Blood loss Children with hereditary spherocytosis have all of the listed conditions except: 1. positive Direct gil i fra d rm al os m ot ic ea se 0% .. CH C 0% M in .. . in cr in es it i al rm ab no sp e la lb ga l ly, ab no 0% ct r dd e m Co o ct eg a om eD ir e 0% ... bs 0% en 4. 5. sp l 3. po s it iv 2. Coombs splenomegaly, gallbladder stones abnormalities in spectrin and /or ankyrin increased MCHC abnormal osmotic fragility test. 6 Spherocytes Spherocytes Nucleated rbc Coombs-AIHA Osmotic fragility-HS HS- with severe anemia A 6 year old girl who has hereditary spherocytosis presents with a 1 week history of fever. Physical examination reveals abdominal pain, vomiting, fatigue and pallor. Her hemoglobin is typically about 10 g/dL with a reticulocyte count of 9%, but now, her hemoglobin is 4 g/dL and the reticulocyte count is 1%. Her bilirubin is 1 mg/dL. Of the following, the MOST likely cause for this girl’s present illness is infection with – – – – – Coxsackie virus Parvovirus B19 Epstein-Barr virus Hepatitis A virus Influenza A virus HS- with severe anemia 0% ru s za A vi vir u In flu en sA at it i He p 0% s 0% rr vir us Ep st ei n- ru s Pa rv ov i e ck i Co xs a 0% B1 9 vir us 0% Ba 1. Coxsackie virus 2. Parvovirus B19 3. Epstein-Barr virus 4. Hepatitis A virus 5. Influenza A virus 6 Newborn Screening Questions You get a call from a frantic parent because she received a letter from the State regarding her baby’s test results on NBS. FS- SS disease, S-B0 Thal, Sickle cell w/ HPFH. FSA- Sickle B+ thal, Sickle cell trait FSC- SC disease FAS- Sickle cell trait FAC- Hb C trait FAE- Hb E trait FE - Hb EE disease, E-Thal Sickle cell Questions Hemolysis- life span 20-50 days. Abnormal cell shape, abnormal adherence to endothelium, decreased oxygenation, Increased polymerization. Symptoms start by 2-4 months of age. Hb electrophoresis, S >75 %. Penicillin daily until age 5. Prevention of pneumococcal infections-asplenic. PPV (Pnu-23) age 2, 5 Meningococcal vaccine early two doses and every 5 years. Folic acid daily Sickle cell questions Vaso-occlusive crisis New infant born in another country presenting with swollen hands---Dactylitis Aplastic crisis: – low Hb, low retic, Secondary to Parvovirus B 19 infection. Splenic sequestration crisis: – – – – Sudden enlargement of the spleen in SS or older SC patient Rx- Transfuse Teach spleen palpation Splenectomy The mother of a 10 month old baby with SS disease asks you about prognostic indicators. All of the following indicate likelihood of more severe disease except: 1. High WBC 2. Associated alpha 0% .. . m ep iso de he Lo w th a ph a Re pe ia at ed te d al 0% so fd ac ob i og l ss . .. la h Hi g 0% n W BC 0% As so c thalassemia trait 3. Low hemoglobin 4. Repeated episodes of dactylitis 6 Sickle cell Acute Chest Syndrome True statements include all except: 1. Presents with a new infiltrate on X-ray 2. Due to infarction, infection, BM fat embolism 3. Treat with antibiotics to cover pneumococcus, Mycoplasma, Chlamydia 4. Treat with bronchodilator, Incentive spirometry, transfusion, Steroids (controversial). 5. Intensive hydration is important TCD- Transcranial Doppler A routine TCD on a 4 year old patient with SS disease shows a Cerebral blood flow (CBF) of 210 cm/second. What is the next step? STOP studies- STOP I and II According to the STOP protocol all children with abnormal TCD require enrollment in hypertransfusion protocol till (choose one) Repeat TCD is normal 2. Continue indefinitely 3. the child reaches 18 years 4. MRA/MRI are reported normal 1. ... ed or t 18 ar er ep es M RA /M RI re ac h ild ch th e 0% rs 0% ye a fin it e in de no Co nt in ue is D TC pe at Re 0% ly rm al 0% 6 Sickle cell and Stroke Questions Affects 10 % of patients Infarctive stroke (younger patients) Hemorrhagic stroke (older) STOP I study established the role of yearly TCD (transcranial doppler) to measure cerebral blood flow velocity as a tool for determining stroke risk. Transfusion therapy as current therapy for high risk patients (CBF> 200cm/sec) Reversal of CBF velocity is not sufficient to stop transfusion therapy. (STOP II) Sickle cell and Hydroxyurea FDA approved for adults Studies in children demonstrated efficacy and safety Increases hemoglobin F level Increases hemoglobin Decreases WBC – ancillary effect Reduces number of ACS, VOC Hydroxyurea is recommended by the hematologist for patients who have recurrent vaso-occlusive crises, acute chest syndrome. A healthy 5 year old boy- 2 day hx of fever, P/E normal No hepatosplenomegaly, LN, no focus of infection. CBC WBC 3, Neutrophils 25 %, Hb 12, Platelet 200X109/L, ANC 750. Most appropriate step is ist 12 w ol og a CB C in he m at as pi ra Re pe at to fe r Re 0% ee ks 0% te s. 0% BM fo r1 0 da y ys da 10 0% GCS F fo r in cil l 5. 0% ox i 2. 3. 4. Amoxicillin for 10 days G- CSF for 10 days. BM aspirate Refer to a hematologist Repeat CBC in 1-2 weeks Am 1. 6 Case A 2-year-old boy has had several 10-day-long episodes of fever, mouth ulcerations, stomatitis, and pharyngitis. These episodes have occurred at about monthly intervals. Absolute neutrophil counts have been 50/mm³on day 1 of each illness, 500/mm³ on day 10, and 1,500/mm³ on day 14. Among the following, the MOST likely cause for the findings in this patient is A. chronic benign neutropenia B. cyclic neutropenia C. Schwachman-Diamond syndrome D. severe congenital neutropenia E.. transient viral bone marrow suppression Abnormal Bleeding Epistaxis unrelieved by 15 minutes of pressure, both nostrils, requiring an ER visit, documented drop of hemoglobin. Menstrual periods( amount, pads, duration) Bleeding after procedures (circumcision, dental extractions, T and A-delayed bleed) Ecchymoses/bruising inconsistent with the degree of trauma Bleeding patient Physical Examination: Type of bleeding: Superficial or deep – Bruises, Petechiae – Epistaxis, Gum bleeding, Excessive menstrual bleeding – Site of bleeding – Bleeding into the joints and soft tissues – Look for evidence of shock – Medication history (Aspirin, NSAIDS) Lab studies (What do they measure?) CBC and Peripheral smear PT, INR and PTT – PT - Factor VII, common pathway – PTT- Factor VIII, IX, XI, XII, common pathway Mixing studies (Inhibitors and deficiency) Specific coagulation factor assays Coagulation cascade Questions on Circulating anticoagulant Mixing study If PT or PTT is prolonged, ask for a mixing study. Mix patient plasma with equal amount of normal plasma, the test will normalize if the abnormal result is because of a deficiency in factor. If there is an anticoagulant, it will not normalize or even if it does, it will become abnormal again after incubation. A healthy 2-day-old boy born at term undergoes circumcision. Bleeding noted at the site 10 hours after the procedure and increased steadily over the past 4 hours. Findings on exam are unremarkable except for bleeding along 2 to 3 mm of the surgical site; no petechiae or purpura. 0% 0% 0% e 0% Ne as nd di se t. . . Vo n W ill eb ra m un e m lo i on a ta l al th ro m bo cy t op e h. .. ... . la un e to r Im m VI II d ef ic i en cy va sc u tra in ed 5. Fa c 4. 0% in at 3. em 2. Disseminated intravascular coagulation Factor VIII deficiency hemophilia Immune thrombocytopenic purpura Neonatal alloimmune thrombocytopenia Von Willebrand disease Di ss 1. 6 Hemophilia Questions Factor VIII deficiency (Hemophilia A)-85% – X-linked recessive, Carriers asymptomatic – Severe<1%, Moderate 1-5, Mild 6-30 % – Treat Recombinant Factor VIII 1unit/kg raises factor level by 2 %. Half life 12 hrs. Joint bleeds need100%, muscle bleeds 50 %. – DDAVP for mild cases. – 30 % develop inhibitors after infusions with concentrate (Approx 50 infusions) Factor IX deficiency (Hemophilia B) – X-linked recessive, less common A patient with Hemophilia A has asked you about the possibility of his children being affected by the disease. The partner is normal. th .. ch a 00 % Th er e is a1 00 % a1 is er e Th 0% nc e th .. nc e ch a ch a 0% a5 is er e Th 0% th .. 0% nc e th .. nc e ch a 0% a5 4. 0% is 3. er e 2. There is a 50 % chance that his sons will have the disease. There is a 50 % chance that his daughters will be carriers There is a 100 % chance that his sons will have the disease There is a 100 % chance that his daughters will be carriers Th 1. Case 13 year old girl just started her periods and has been bleeding for the past 16 days. She has used 14 pads a day and is tired. Her vital signs are stable, Hb 9.5, PT, PTT normal. The mother had heavy periods and her 6 year old brother has nose bleeds for the past 2 years. Likely to have: Questions on Von Willebrand’s Disease 1-2 % of population Type I - 80 % of cases; Quantitative defect, Autosomal dominant (AD) Type 2 - 15-20 %, Qualitative defect – 2A, 2b (thrombocytopenia), 2M, 2N (AR) Type 3 - Severe (similar to hemophilia A) Autosomal recessive (AR) DDAVP- Releases VWF from endothelial cells and stabilizes Factor VIII – SE: Water retention, Tachyphylaxis, hyponatremia. – For mild Hemophilia, Type I VWD, 2 – Contra-indicated in Type 2B Rx-Plasma derived VWF containing concentrates Thrombophilia A 14 year old male presents with chest pain and difficulty breathing. He notes that his right calf has been swollen for the last 3 days and he has difficulty placing his foot on the ground. P/E Pain on dorsiflexion, Air entry reduced. CXR and EKG are normal. VQ scan shows a filling defect and a diagnosis of DVT and pulmonary embolism is made. What are the important questions on history? – History of DVT in family members – H/o recurrent late miscarriages in mother and her sisters. – H/o trauma and precipitating factors The most common cause of familial predisposition to thrombosis is io n ef ic i III d m en om bi n id Le An t it hr V to r 0% en cy 0% ut at en cy cy C 0% Sd ef ic i en Pr ot ei n tib an Pr ot ei n lia op hi He m 0% de fic i od i es 0% Fa c 1. Hemophilia antibodies 2. Protein C deficiency 3. Protein S deficiency 4. Factor V Leiden mutation 5. Antithrombin III deficiency Tests performed on donated units of blood ... fro in ed fo rH ... on ly ar e un it s 0% un it s te ste d fo r es te d et all 0% ob ta f. . on ly ar ni ts lu al 0% HI .. 0% d es te et lu ni ts ar et es te d on ly f. . 0% ar 5. al 4. ni ts 3. lu 2. all units are tested only for hepatitis B and C all units are tested only for human immuno-deficiency virus (HIV) all units are tested for HIV, hepatitis B, and hepatitis C all units are tested for HIV, hepatitis B, hepatitis C, sickle cell trait, cytomegalovirus, and Epstein-Barr virus only units obtained from donors who have one or more risk factors are screened for HIV, all units are tested only for hepatitis B and C al 1. 6 Questions on Transfusion CMV negative- give leukocyte reduced. Irradiated products- To prevent GVHD Washed cellsPhenotype matched – To prevent allo-immunization Sickle negative CANCER IN CHILDREN Childhood Cancer Distribution Distribution-All ages Leukemia Lymphoma Brain Tumor Soft tissue sarcoma Germ call Bone Neuroblastoma Renal Retino Hepato Carcinoma Other A 6-year-old girl has aching in her arms, legs, and back for > 2 weeks. Results of laboratory tests include hemoglobin, 9.4 g/dL; white blood cell count, 5,600/mm³ with no abnormal cells noted on smear; and platelet count, 106,000/mm³. Radiographs of long bones reveal osteolytic lesions and radiolucent metaphyseal growth arrest lines. m ye lit is ng 0% os te o as e 0% ad M ul tif o ca l le ch er d ise em Ga u an 0% po is o ni 0% ia AL L 0% st ic ALL Aplastic anemia Gaucher disease lead poisoning Multifocal osteomyelitis Ap la 1. 2. 3. 4. 5. 6 ALL (Acute Lymphoblastic leukemia) 75% of all Leukemias Can present with generalized bone pain, fatigue Bruising, nose bleeds Unusual fevers, infection Lymphadenopathy, hepatosplenomegaly ALL- Should know (Acute Lymphoblastic leukemia) Abnormal to see blasts in the peripheral smear Diagnosis: >25 % blasts in the BM. Normal marrow has < 5 % blasts Single most common childhood cancer (29% of all childhood cancers); 2500-3500 cases per year Peak age 2-5 years More likely in Trisomy 21, Ataxia-Telangiectasia, Bloom syndrome, Kostmann’s, Monosomy 7, DBA, Fanconi anemia, 20% risk in twin if age <5yrs ALL Treatment Induction: 4-6 weeks, Consolidation /delayed Intensification: 6-12 months; rotating drugs. Maintenance : Daily oral 6-MP, weekly MTX, Monthly pulses of Vincristine and Steroid. Imatinib mesylate-Tyrosine Kinase Inhibitor- Ph Chromosome positive patients CNS prophylaxis: Intrathecal chemo CNS Therapy: RT + Intensive systemic chemo Testicular disease: RT SANCTUARY- CNS, Testis ALL- Prognosis Prognosis: WBC, Age, Cytogenetics – good if hyperdiploidy (>50),trisomy 4,10,17, t(12,21) – Bad if hypodiploid, Ph. chrom t (9,22),t(4,11), t(8,14) Immunophenotype: Pre-B good, B and T-worse Early response, Minimal residual disease (MRD) Infants: 50 % survival Early relapse is a poor sign Down Syndrome and Leukemia 10-20 fold increase DS: 400 fold Increase in M7 AML Superior response to Rx of AML Transient Myeloproliferative disorder in newborn which resolves within 3 months. Acute Myeloid Leukemia (AML) 20 % of all leukemias Increased incidence in < 1 year of age Higher incidence: – Downs, Fanconi, Bloom, DBA, Kostmann, Neurofibromatosis I, Schwachman-Diamond Chloromas– solid collection in bone/soft tissues Types: M0-M7, commonest M2 DIC in M3- (Promyelocytic- APML) M7- Downs syndrome Question Hodgkins • • • • • 16 year old male presents with a painless swelling in the supraclavicular region. Biopsy shows Hodgkins disease Stage 2. All are true except: 1. Presence of “B” symptoms is worse for prognosis 2. B symptoms are fever, increasing size of mass 3. Staging depends on whether it is on one or both sides of the diaphragm 4. Sperm banking should be done 5. Second malignancy can occur in patients who receive combination chemo and RT Question 4 year old boy presents with a 6 day history of bilateral, rapidy progressive 1. 2. 3. 4. 5. facial swelling. There is no history of associated trauma or upper respiratory symptoms. On P/E, there is significant swelling below both eyes and of both cheeks. The angle of the jaw is maintained. On examination of the oral cavity, both the soft and hard palate are swollen as are the gingiva. The teeth are loose and inverted due to the degree of gingival swelling. A CT of the sinuses reveals extensive bilateral opacification of both maxillary sinuses. LDH was 1,850 U/L. Which of the following is the most likely to cause of this patient’s physical findings? Human herpesvirus 6 Cytomegalovirus Cryptosporidium hominis Parvovirus B19 Epstein-Barr virus Burkitt’s Lymphoma Endemic Burkitt’s – African type, head and neck, jaw – 95 % chance of EBV Sporadic Burkitt’s – Abdomen – 15-20 % chance of EBV t (8;14) Immunotherapy: Anti-CD 20 monoclonal antibody; (Rituximab) Question 5 yr old boy with progressive vomiting, headache, unsteady gait and diplopia for 4 weeks. MRI shows a contrast enhancing tumor in the 4th ventricle with obstructive hydrocephalus. Brain Tumors- Important to know 20% of all malignancies in children Age 3-7 years Most often infratentorial Sx: Persistent vomiting, headache, gait imbalance, diplopia, ataxia, vision loss, school deterioration, growth deceleration Associations with Inherited Genetic disorders: – Neurofibromatosis, Tuberous sclerosis, VonHippel-Lindau disease, Li-Fraumeni (glioma), Turcot syndrome Medulloblastoma - most common CNS tumor – Trt: Resection, Craniospinal RT, Chemo – Prognosis: Age, large size, degree of resection, dissemination, histology. Wilms Tumor An 18-month-old girl is being evaluated because her mother thinks her abdomen seems “full.” Physical examination reveals an abdominal mass. Ultrasonography identifies a solid renal mass. At surgery, a stage I Wilms tumor is found. Stage I Wilms- Chance of 4-year survival is CLOSEST to 0% 0% 95 % 0% E. 0% D. 75 % 0% C. 60 % 5. E. 45 % 4. D. B. 3. C. 30 % 2. B. 30% 45% 60% 75% 95% A. 1. A. 6 Wilms Tumor- Important Presentation: No Sx, HT, Hematuria, Malaise Histology: favorable(FH) vs unfavorable (UH) Staging: I-local, II-excised, III-residual, IVmetastases, V -bilateral Treatment: Nephrectomy, Chemo-all, St I-II-2 drugs-18 weeks, St III-IV- 3 drugs+ RT Prognosis: – FH: > 90% at 2 years – UH: < 60% at 2 years Congenital anomalies associated with Wilms’ tumor include all of the following except 1. Polydactyly 2. Aniridia 3. Hemihypertrophy 4. Cryptorchidism hi d Dr as h pt or c sy nd ro m y op h De n ys - Cr y ih 0% e 0% ism 0% rtr An ir i di a 0% He m Po ly da c ty l y 0% yp e 5. Denys-Drash syndrome 6 A 9 year old previously healthy girl manifests progressive painless proptosis and decreased visual acuity of the left eye during a 2 month period. The most likely diagnosis is: a. Pseudotumor of the orbit b. Trichinosis c. Retinoblastoma d. Rhabdomyosarcoma e. Orbital cellulitis Rhabdomyosarcoma Painless non tender mass 60% under age 6 Sites: head & neck, GU, Extremities, mets lungs. Majority sporadic, associations: B-W, Li Fraumeni, NF 1 Types: – Embryonal 70%, better prognosis – Alveolar 30 %, trunk, worse prognosis Treatment: Surgery, Chemo, local control RT Mass The mother of a 22-monthold boy reports that he has been fussy and tired. Findings on physical examination confirm the presence of a nontender rt upper quadrant mass. Bilateral periorbital ecchymoses also are noted. Of the following, the MOST likely cause for these findings is A. multicystic kidney disease B. neuroblastoma C. non-Hodgkin lymphoma D. Hepatoblastoma E. Wilms tumor All statements are true about Neuroblastoma except: M gn os .. on l yd ia .. . os tc in qu en t Fr e 0% om m ye ar ca on m om 0% s, 97 t.. ri n nc e ith rw be tte M os tc sis 0% <4 an -cr tra ex 0% N. .. i.. 0% m on 5. Pr og no 4. om 3. os tc 2. Most common extracranial solid tumor Prognosis better with Nmyc oncogene amplification and tumor diploidy (DNA index 1) Most common cancer in the first year of life Frequent in <4 years, 97 % cases by 10 years Most commonly diagnosed as Stage III or IV M 1. 6 Case A 16 year old male comes in because he fell in the supermarket. P/E shows a small painless mass on the medial aspect of the knee. • X ray shows a fracture and a lytic sunburst pattern. (periosteal elevation)-OS • Xray shows an onion peel appearance- ES • Xray- radioluscent, sharp, rounded lesion < 2cm with reactive sclerosis- Osteoid Osteoma X ray and MRI Ewing’s Sarcoma Osteogenic Sarcoma MRI, Bone scan, Biopsy, CT Chest for mets. Peak incidence- 2nd decade Predisposition: Hereditary retinoblastomas, LiFraumeni, Pagets, RT, Alkylating agents 60 % near the knee (Metaphyses of long bones) History of fall, pain common symptom, mass, no systemic symptoms. Treatment: Sperm banking, Neo-adjuvant Chemotherapy, limb preserving surgery. A 16 year old Caucasian female comes with complaints of chest pain and difficulty breathing for the past one week. She has had fever, wt loss over the last 2 months. She has reduced air entry and CXR shows a moth eaten appearance of one of the ribs and a pleural effusion. Biopsy is done and is consistent with Ewing’s Sarcoma Retinoblastoma- need to know Presentation: Leukocoria (cats eye reflex), dilated pupil, esotropia, strabismus Unilateral 75 % (could be hereditary/non) – 60 % unilateral and non hereditary – 15 % unilateral and hereditary (RB1 mutation) Bilateral 25 % – 25 % are bilateral and hereditary, have RB1 mutation – Earlier age, 11mos, Can develop in each eye separately – Higher incidence of sarcoma, melanoma, brain tumors. A child with ALL was started on Chemotherapy. She had a WBC 82,000, Hb 9gm, plt ct 45,000. She develops tumor lysis syndrome: Which depicts Tumor lysis .. hi g h, hi g P gh , hi K 0% LD H , al ,P al rm no K 0% LD .. . h. .. no rm hi gh ,P rm al no K 0% LD H , LD H , al no rm P gh , hi 0% h. .. ... no r LD H h, hi g K 5. 0% P 4. gh , 3. hi 2. K high, P high, LDH normal, Na high K high, P normal, LDH high, Na nl K normal, P high, LDH high, Na high K normal, P normal, LDH high, Na normal K high, P high, LDH high, Na normal. K 1. Tumor lysis syndrome Rapid destruction of cancer cells. Release of intracellular ions, also Uric acid, can cause tubular obstruction and damage. Treatment: Allopurinol or Rasburicase early, hydration, alkalinization, diuretic therapy. Spinal cord compression Presentation: back pain worse with movement, neck flexion, straight leg raising, valsalva – Weakness; partial/complete paralysis, Incontinence Local tumor extension or metastasis Lymphomas, neuroblastoma, soft tissue sarcomas Therapy: Urgent treatment to relieve pressure and prevent permanent neurologic damage. – – – – Neurology/Neurosurgery consult High dose dexamethasone Emergency radiation therapy Laminectomy Questions on-Superior Vena Cava Syndrome Mass lesion obstructs flow through the SVC Symptoms Dyspnea, edema of face, neck, upper extremities – Periorbital edema, conjunctival edema (itchy eyes) – Dysphagia, resp distress, vocal cord paralysis Tracheal compression: resp distress, wheezing Due to- NHL, Tcell ALL, Lymphoma, Secondary cause: occluded central venous catheter Chemotherapy-Side effects that you need to know Anthracyclines: Cardiac toxicity Vincristine: foot drop, peripheral neuropathy Cisplatinum: kidney, deafness Methotrexate, 6MP: Liver toxicity Bleomycin: Pulmonary fibrosis Asparaginase: Pancreatitis, Coagulopathy Etoposide (VP-16): Secondary AML Cyclophosphamaide: Hemorrhagic cystitis (MESNA as Uroprotector) and Infertility Fever, Neutropenia Single most important risk factor: ANC Organisms: Gram negative infection, Staph epi in catheter patients Medication: Broad spectrum 3rd generation antibiotics Anti-fungal after 4 days Examine patient thoroughly 16-year-old girl, completed therapy at age 8 for Hodgkins disease with Involved field RT and chemo. She now develops petechiae, purpura, lymphadenopathy and hepatosplenomegaly.Lab include: plt 12,000,Hb 8.0 gm/dL; and WBC 13,000/mm³. She has…. 0% d nd uc e e. .. Vi ra l- i an st ic pl a ta on se te - 0% IT P IT d el va r ic Dr ug La ed in at in du ce .. ig. al m em se co nd Di ss 0% P 0% la 0% sa 5. La 2. 3. 4. AML as a second malignancy Disseminated varicella Drug-induced ITP Late-onset aplastic anemia due to chemotherapy Viral-induced ITP AM 1. 6 You are evaluating a 9 year old child for short stature. She was treated at 3 yrs of age for ALL, received cranial RT. Her height is < 5th percentile and she is Tanner stage I. Most likely to have an abnormal test of 1. Growth hormone 2. Estradiol 3. Follicle stimulating 0% 0% gh o. .. g.. . at in le ul re sti m n op i ot r yr oi d Th Go na d st im lic le as in ho r. . . di in g ul at wt h Fo l 0% ol 0% Es tra ho rm on e 0% Gr o hormone 4. Gonadotropin releasing hormone 5. Thyroid stimulating hormone 6 Need to know- Late effects of cancer therapy RT: Hypothalamic pituitary axis is impaired; central hypothyroid and Adrenal insuff. RT doses higher in brain tumor GH is dose sensitive to the effects of RT Age related: < 5 years susceptible Panhypopituitarism with higher doses ovarian failure with RT A 16 year old boy is receiving chemo for rhabdomyosarcoma He recd a year of cycles of Vincristine, Actinimycin-D and Cyclophosphamide. Most likely endocrinologic late effect of this therapy 1. Growth hormone deficiency 2. Hypothyroidism 3. Impotence 4. Infertility 5. Osteoporosis 0% 0% 0% 0% Gr o wt h ho rm on e de fic i en Hy cy po th yr oi di sm Im po te nc e In fe rti lit y Os te op or os is 0% 6 Chemotherapy effects Chemotherapy with alkylating agents Females: less effects than males normal puberty early menopause Males: irreversible gonadal toxicity sterility with azospermia Puberty usually not affected (leydig cells) The most common reason for the failure of hematopoietic stem cell transplantation is Ve no - oc c 0% 0% 0% ft v In fe c tio s. n ho st di se as Gr e af tr ej ec tio n 0% en ce ur r ec er as Di se lu siv e di se as e of .. . 0% Gr a 1. Veno-occlusive disease of the liver 2. Disease recurrence 3. Infection 4. Graft vs. host disease 5. Graft rejection 6 GVHD ( Graft vs Host disease): All are true except 0% 0% 0% 0% ac tio n eG of th VH e D ... Af st ar fe ts ct st w ith he in sk Irr .. . in ad , li ia ve tio ra n nd of Co bl .. m oo pl d et pr e od HL ... A m at ch in g. .. 0% re 5. Ac ut 4. he 3. st 2. It is the reaction of the donor lymphocytes against the host. Acute GVHD starts within the first 100 days and chronic is after 100 days. Affects the skin, liver and GI tract Irradiation of blood products does not help Complete HLA matching prevents GVHD It i 1. 6