Cytology and Cytological Techniques - Yola
advertisement

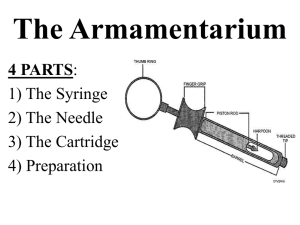
Cytology and Cytological Techniques Clinical Pathology Cytology The microscopic examination of cells. Generally refers primarily to cells exfoliated from tissues, lesions, and internal organ/tumor cells. A very valuable diagnostic tool. Is inexpensive Is quick and easy Involves little or no risk to the patient Cytology Continued Must be able to identify normal cells from abnormal cells, and inflammatory from non-inflammatory cells Disadvantage may be that some tumors do not exfoliate cells well and therefore may not provide and adequate sample to examine. Cytologic Interpretation May be able to diagnose Identify the disease process Help form a prognosis May determine what diagnostic procedures should be performed next May help with therapy options Cytologic Techniques Fine Needle Aspirate (FNA) Fluid AspirationThoracocentesis/Abdominocentesis Solid mass imprinting Vaginal wall technique Cerebrospinal (CSF) Fluid Analysis Synovial Fluid Analysis Nasal Flush General Collection Techniques When possible prepare several smears Use stained and unstained techniques May use a variety of stains Use clean, dry slides Scrapings Done on freshly cut surfaces Scrap lesion/tissue with clean scalpel blade Place material collected on a slide and spread Advantage: May collect more cells Disadvantage: More difficult to collect and only able to collect superficial lesions Imprints May be prepared from external lesions (ulcers) May be prepared from tissues excised during surgery or necropsy. Easy to collect Disadvantage: May only collect few cells and may contain contamination Solid Mass imprints Cut mass in half Blot dry Need to remove blood/tissue fluid from surface Use sterile gauze or other absorbent material Excess blood/fluid inhibits cells from spreading and assuming normal size and shape Touch the slide to the blotted surface Stain Fine Needle Aspirates Preferred method of obtaining samples from masses. Avoids superficial contamination Very little risk to patient Less complications to internal organs than core biopsy techniques Implantation of malignant cells along the aspiration tract is extremely rare Disadvantage: May not get a good sample because using just a small needle. Fine Needle Aspirate 2 techniques Aspiration Collect with 22-25 gauge needle Use 3-12 ml syringe Need slides Non-aspiration FNA Aspiration Technique Hold mass/lymph node firmly Introduce the needle with syringe attached into the mass Apply strong negative pressure by withdrawing the plunger to about 2/3 -3/4 of the volume. Do several times in same area or redirect needle. Stop negative pressure and remove needle from mass Remove needle from syringe and air is drawn up into syringe Sample that is in hub of needle is expelled onto slide by rapidly depressing the plunger Hold needle close to slide, if too far away will result in small droplets that dry rapidly before smear technique may be done. FNA Non-Aspiration Technique Works best for small masses that are difficult to aspirate. Works well for highly vascular tissues Using a needle only, move rapidly back and forth (stabbing motion). Withdraw needle and place syringe with air to force onto slide. Preparation of smears from aspirates Squash prep method Needle spread method Blood smear method Squash Preparation With experience, can yield excellent cytologic smears Aspirated material is placed on the center of the slide A second slide is placed over the sample to form a cross. Carefully slide apart from first slide (Put down on and pick up to move). Do not place excessive downward pressure to the first slide because will cause distorted ruptured cells The weight of the spreader slide is sufficient to adequately spread the cells. Needle Spread Method Spread aspirate on the slide with tip of needle. Pull sample out into several projections (starfish appearance). Blood Smear Technique Use if material is thick or fluid After material is expelled on slide, second slide is held at 30-40˚angle. Second slide is pulled backward until it contacts the fluid Rapidly move forward like a blood smear. Common Problems with FNA Few or no cells obtained Some lesions do not exfoliate cells well. The needle may miss the site of the lesion Timid collection Inadequate negative pressure Blood contamination Using too large needle gauge Prolonged aspiration Failure to blot if doing imprint Common Problems with Preparation Poorly prepared slides due to thick or high cell numbers Allowing material to dry on slide before squash prep or other smear technique. If a large amount of material is present, spread between two slides May have to do 4-5 slides form the same site in order to get valuable diagnostic sample. Staining Slides Diff-quik, Wright’s, Geimsa Papanicolau stains used in human Ob/gyn exams. Stains nucleus and nuclear material better. New Methylene Blue stain Air dry these slides, do not heat fix. Use clean slides (make sure no lint on slide) Stain immediately after air drying Take care not to touch the surface of the slide or smear at any time. Medical Terminology Hypertrophy-an increase in cell size and/or functional activity in response to a stimulus. Hyperplasia- increase in cell numbers, via increased mitotic activity, in response to a stimulus. Neoplasia- increase in cell growth and multiplication that is not dependent on an external stimulus. Metaplasia- a reversible process in which one mature cell type is replaced by another mature cell type (adaptive response to a stimulus) Medical Terminology Continued Dysplasia- reversible, irregular, atypical, proliferative cellular changes in response to irritation or inflammation. Anaplasia- A lack of differentiation of tissue cells Less differentiated cells in a tumor is more malignant Chromatin pattern- the microscopic pattern of nuclear chromatin (the chromatin pattern coarsens as malignant potential increases)