Lumbar
Puncture
What you need to know
(and what I wish I had)
Mark Keezer, MDCM, FRCPC
MSc candidate, Epidemiology, McGill University
Epilepsy Fellow, National Hospital for Neurology &
Neurosurgery, London, UK (to begin in September, 2013)
NEJM video
http://www.nejm.org.proxy1.library.mcgill.ca/doi/full/10.1056/NEJMvcm054952
Outline
1.
2.
3.
4.
Preparation
The Procedure
Interpreting the Results
PLPHA
1. Preparation
a.
b.
c.
d.
e.
Consent
Antiplatelets
Labs
Neuro-imaging
Supplies needed
Patient consent
•
•
•
•
Back pain
Radicular pain
Hemorrhage
Infection
• PLPHA (~40%)
Should antiplatelets or
prophylactic heparin be
held?
• Prospective cohort
o 924 orthopedic patients undergoing spinal or epidural anesthesia
o 39% receiving antiplatelets
o 2% receiving prophylactic heparin
o 0 epidural hematomas
• No relationship with minor hemorrhage during procedure
Horlocker TT et al. Preoperative antiplatelet therapy does not increase the risk of spinal hematoma associated with regional
anesthesia. Anesth Analg 1995;80:303-9.
•
Risk of epidural hematoma with clopidogrel unknown
What are the minimum
platelet count and INR
values?
Coags & platelets
• Platelets > 50,000
• INR <1.5
• Guidelines at the Preston Robb day centre
o Currently it seems it is acceptable to not verify CBC and coags if patient
reasonably expected not to have any abnormalities (verbal
communication with Dr. Durcan).
• Prospective cohort 301 patients
• Risk factors for CT head abnormality
o
o
o
o
o
>60 yo
Immunocompromised
Hx of CNS disease
Hx of seizure within 1 wk
Abnormal neurologic exam
• Including poor comprehension
• Sensitivity 94%
• Specificity 51%
Hasbun R et al. Computed Tomography of the head before lumbar puncture in adults with suspected meningitis. NEJM
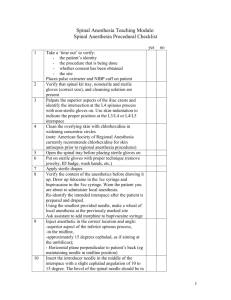
The LP kit
What else do you need?
• The obvious
o Xylocaine
• 1% or 2%
• With or without epi
o Topical disinfectant
• 5% chlorhexidine (avoid detergent and 0.5% solution)
• Proviodine solution
• The essential
o Sterile gloves
o Face mask
• The helpful
o Piquet
• Keep your RN happy
o 2 Pillows
CSF tubes
• How many tubes do you need?
• How much CSF in each tube?
o 1 cc
• For most standard tests
o 2 cc
• HSV PCR
• OCB (don’t forget to send serum!)
o 3 cc
• Cytology
o 8 cc
• AFB cultures
• Fungal cultures
Local anesthesia
• Max xylocaine dose (70 kg individual)
o 30cc if 1%
o 15cc if 2%
o s/c needle alone vs additional 20 gauge needle
• The “bleb”
2. The Procedure
a.
b.
Positioning
Vertebral level
Positioning
• Back as close to edge of bed
as possible
• Maximize anteroflexion
• Minimize lateroflexion
o Pillow under head & between legs
o Be careful of the shoulders
o Palpate along the vertebral bodies
Tuffier’s line
Vertebral level
• L3-L4 vs L4-L5
o Compromise between width of the space and spondylosis
o Conus medullaris extends to L2-L3 in 6% of pts
The Procedure
• Aim towards the umbilicus
• The expected resistance of
the interspinous ligament
• The satisfying “pop” of the
ligamentum flavum
The stylet
• Never move the needle without the stylet!
• With insertion of the needle
o Avoid introduction of a plug of epidermis into the subarachnoid space,
allowing for the growth of an epidermoid tumour
• With removal of the needle
o Prevent a strand of arachnoid being threaded into the dural defect,
increasing risk of PLPHA
• If not in the proper space
o Most often needle is deviated from the midline
• Hence the radicular pain
o Attempt with large gauge needle (18 or 20 gauge)
• If no CSF
o Rotate the needle 90°
o Advance further or withdraw
• If slow flow
o Valsalva manoeuvres
• Throw out any bloody needle
Negative pressure LP
• Has been studied and found to be safe
o Only while using 25 gauge needles or smaller!
Linker G et al. Fine-needle, negative-pressure lumbar puncture: a safe technique for collecting CSF. Neurology 2002;59:2008–2009.
3. Interpreting the Results
a.
b.
c.
Normal values
Tubes 1 & 4
Correcting for a traumatic tap
Normal CSF values
• ≤ 5 RBC / μL
• ≤ 5 WBC / μL
• Protein
o ≤ 0.5 gr/L
• Cytology
o 80% sensitive for leptomeningeal carcinomatosis from lymphoma or
leukemia.
• 123 patients with suspected SAH
o 8 patients with ruptured aneurysm on CA but negative CT head
o 2 patients had a > 25% in RBC count between tubes #1 and #4
Correcting WBC in a
traumatic tap
• RBC x (peripheral blood WBC count ÷ peripheral
blood RBC count)
o Usually ~ 1000
Correcting protein in a
traumatic tap
• Add 0.01 gr/L for every 1000 RBC / μL
4. PLPHA
a.
b.
c.
Proven methods to decrease risk
Unproven methods
Treatment
What can we do to prevent
PLPHA?
PLPHA prevention
• Proven methods
o Bevel parallel to spine
o Atraumatic needle
o Needle gauge
• Unproven
o Recumbency
o Volume of CSF removed
• Systematic review of the literature
o Atraumatic needle superior to Quincke
• 24% versus 12%
o Small gauge superior to large gauge
Needle types
}
“atraumatic” needles
• Prospective cohort 239 patients
• Sex
o Women = 46%; men = 21%
• Gauge
o 20 gauge = 50%; 22 gauge = 26%
Vilming ST et al. The importance of sex, age, needle size, height and body mass index in post-lumbar puncture headache.
Cephalalgia 2001;21:738–743.
Bevel orientation
• Prospective cohort of 380 patients
o Bevel parallel to spine (bevel up)
• 7.9% with PLPHA
o Bevel perpendicular to spine
• 19.3% with PLPHA
Kochanowicz J et al. Post lumbar puncture syndrome and the manner of needle insertion [in Polish]. Neurol Neurochir Pol
1999;32(suppl 6):179–182.
• Post LP recumbency has been studied by several
studies, none of which have shown any clear
benefit (up to 24 hrs)
• Most clinicians will generally enforce some period
o Dr. Bray’s 45 minutes
Treatment of PLPHA
Epidural blood patch
• 15-20 cc autologous blood
o At site of LP
o Supine 1-2 hrs post
o 95% reported success rate
Summary
1.
Preparation
1.
2.
3.
2.
The Procedure
1.
2.
3.
Positioning!
The stylet
Interpreting the Results
1.
2.
4.
Don’t hold the ASA
CBC, coags and neuro-imaging?
Plan your CSF tubes
Be concientious about Tubes 1 & 4
Correcting for a traumatic tap
PLPHA
o Prevention
• Bevel parallel to spine
• Atraumatic needle
• Needle gauge
o Treatment
Questions?