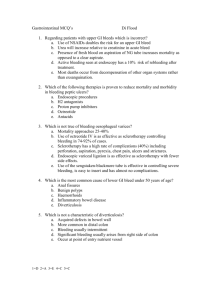
acuteabdomen3
advertisement

The Acute Abdomen Raymond Yiu Surgery Team 3 • Acute Life-threatening intra-abdominal conditions • Requires Emergency admissions • Often requires Emergency surgery Aetiology: Abdominal Pain • EXTRAABDOMINAL – Cardiovascular – Metabolic – Abdominal wall – Neurogenic • INTRABDOMINAL – – – – Imflammatory Traumatic Obstructive Vascular MI DKA rectus sheath haematoma referred pain INTRABDOMINAL – Imflammatory Conditions (Peritonitis) Localised / Generalised Primary / Secondary / Tertiary – Traumatic Blunt / Penetrating Injury Bleeding / Peritonitis – Obstructive Gastric/ Small / Large Bowel – Vascular Mesenteric infarction Strangulated hernias Volvulus (small or large bowel) Rupture AAA Aortic dissection Imflammatory Conditions Peritonitis Peritonitis • Bacteria primary/ secondary/ tertiary spontaneous • Chemical Peritonitis: Bacterial secondary: majority of cases perforated viscus / GIT primary: very rare healthy people in absence of surgery and trauma (children and young adult females) streptococcal pneumoniae/ gonococcus laparotomy + washout + antibiotics tertiary: ICU patients persistent/ recurrent sepsis following adequate therapy of secondary peritonitis poor prognosis Spontaneous bacterial peritonitis • Immunocompromised patients with ascites, cirrhosis, renal failure on CAPD, nephrotic syndrome • Gram negative organisms E. Coli in ascites (bacterial translocation) • Present with abdominal pain, fever, generalised perionitis • Ascitic fluid tapwhite cells, gm stain, culture • Treatment by iv cephalosporins, intraperitoneal antibiotics (vancomycin/netelmicin for gm +ve organisms) Peritonitis: Chemical • Leakage of irritant fluids ie urine, bile, acid leading to initial chemical peritonitis • Later secondary infection occurs after a few hours • Clinical Examples: PPU, Bile leak from cystic duct stump post cholecystectomy Peritonitis Clinical Features • Abdominal pain (recent onset) • Irritation of somatic nerves supplying parietal peritoneum • Constant, sharp, aggravated by movement • May be referred to other parts of body (eg shoulder-tip pain in acute cholecystitis) Peritonitis Clinical Features • Systemic: • Abdominal: Generalised Fever Tachycardia Leucocytosis Chills/rigors Dehydration tenderness, guarding, rigidity,absent BS, distention (ileus) localised Peritonitis Localisation of signs and pathology Peritonitis Clinical Features Pancreatitis Liver abscess PPU Cholecystitis Cholangitis Appendicitis Diverticultis Meckels diverticultis Small bowel perf Acute abdomen Common conditions Appendicitis Cholecystitis Acute appendicitis: aetiology Obstruction of lumen by: Lymphoid hyperplasia Faecolith Parasites Cancer/ carcinoid Acute appendicitis: Clinical Features 7% population 10-30 years Mortality rate <1% 5% Elderly and young (delay in diagnosis) Acute appendicitis • RLQ pain • Pain migration • Anorexia, nausea • • • • • RLQ tenderness RLQ guarding RLQ rebound Fever Leucocytosis (80%) Mcburneys point Acute appendicitis: Signs Rovsings sign: Pain in RLQ on pressing LLQ Dumphys sign: Pain on coughing Psoas sign: Obturator sign: Acute appendicitis: Signs Depends on where inflamed appendix is: Retrocecal: Lumbar sign: Pain in right flank Pelvic: irritate bladder: dysuria irritate rectum: diarhoea Acute appendicitis: Ix Acute appendicitis Laparoscopic Young women of child bearing age Open Acute appendicitis: appendiceal mass • Usually reflects delayed presentation • Patient presents with mass in RLQ • +/- peritoneal signs • Mass represents walling off of appendix by surrounding structures • Rx: Osler-schering regime in absence of clinical signs • Conservative rx with IVF and iv antibiotics until sx subside (follow by colonoscopy and interval appendicectomy 4-6 weeks later) Acute Cholecystitis Remember 4 ‘F’s Cholesterol Pigment Calcium Acute Cholecystitis Chemical peritonitis initally Acute Cholecystitis clinical features Short onset RUQ pain Fever RUQ peritoneal signs Murphys signs Acute Cholecystitis Imaging Acute Cholecystitis Treatment • Short duration of sx (<5days pain) – Consider surgery (lap) – Higher incidence of conversion • Longer duration of sx (>5days) – – – – conservative treatment by npo, iv antibiotics Followed by lap cholecystectomy 6-8 weeks later Any signs of perforation requires urgent surgery Interval cholecystitis • Unfit patients – cholecystostomy Intestinal Obstruction Aetiology • Extramural: adhesions hernias (int/ext) tumor • Intramural tumor stricture (radiation/crohns/tb) • Intraluminal Food bolus GS FB Faecal impaction Aetiology by incidence (SBO) • Previous OT: adhesions • “Virgin” abdomen: carcinoma, hernias Questions to ask? • Site: Stomach vs SB vs LB • Presentation: Acute vs Subacute • Urgency: simple mechanical vs strangulating Site: Sx Gastric outlet Small bowel Large bowel Pain Epigastric Central colic Lower colic Vomiting Early Early/late Late/none BO/flatus Normal Normal/ none none Distension upper General General/ localised (just LB) Hyperactive BS Ausculatation Sucussion splash Hyperactive BS Site: X-ray Large gastric bubble Mainly LB dilatation (+SB if competent ICV) AXR Mainly SB dilatation (no LB or rectal gas) Gastric outlet obstruction SB obstruction RT decompression OGD Oral contrast study Virgin abdo Ca caecum hernias Previous OT adhesions LB obstruction Contrast enema (Watersoluble) Presentation: Acute vs Subacute SBO • Acute short onset May require laparotomy if does not resolve • Subacute: on/off symptoms that subside but does not completely resolve Investigate (eg colonoscopy) if subside Repeated attacks may require laparotomy Simple Mechanical Obstruction Can wait vs Strangulating Cannot wait Simple Mechanical Obstruction Simple Mechanical Obstruction Femoral hernias Strangulating obstruction Vascular supply compromised Can occur in any type of obstruction • Closed loop obstruction (eg volvulus, LBO with competent ICV) • Intussusception • Stangulation of mesenteric blood supply (adhesive band, hernias) Sigmoid Volvulus Example of close loop obstruction: both ends of the bowel are blocked and air enters in a one-way valve Sigmoid Volvulus Decompression : bedside sigmoidoscopy or colonoscopy failure intussusception Usually associated with polyps acting as lead point Small bowel ischemia Prolonged strangulation from adhesion band, hernia Small bowel volvulus Recognising bowel ischemia • Awareness is the most important • Pain out of proportion to abdominal signs • Peritoneal signs (may be late) • Sepsis (fever, high WCC, shock , acidosis) Management Hx and exam Initial Mx Baseline Ix Special Ix Preparation for OT History and Examination Discharge Diagnosis Undifferentiated GI causes Gastroenteritis Surgical GI UTI Pelvic Disorder 1972 41% 13% 7% 10% 11% 12% 1977 39% 19% 12% 18% --- Brewer, Am J Surg, 1976; Jazon, AC Scand, 1982; Powers, AJEM, History & examination and simple lab tests have about a 50-60 % accuracy in giving a diagnosis 1993 25% 18% 5% 8% 11% 12% Pattern Recognition is very important ! Pattern Recognition Central colicky Young + abdo pain + male shifts to RLQ region Elderly + Obese female RLQ peritoneal = appendicitis signs + Temp 38 C RUQ RUQ pain + peritoneal = Acute cholecystitis signs (Murphys)+ Temp 38 C Initial Mx NGT analgesia NPO Resuscitation: IVF Iv antibiotics Monitoring devices Foley (CVP) Baseline Laboratory testing Blood tests Plain X-rays ECG WBC Limited utility WBC > 11,000 LR+ = ~ 2 < 11,000 LR- = ~ 0.5 WBC alone doesn’t distinguish patients with surgical disease from non-specific abdominal pain Liver function tests • ↟ Bilirubin/ALP suggestive of biliary obstruction • ↟ Bilirubin/ ALT suggestive of hepatitis • Normal LFT in up to 40% with acute cholecystitis • May be deranged in all types of sepsis. Not specific for any disease entity Amylase – ↟ in acute pancreatitis – May be normal in 40% cases of pancreatitis – Raised in other intra-abdominal conditions eg PPU, hyperamylassaemia, renal failure Urinalysis • Pregnancy test ------> Mandatory for all young females (ectopic) • WBC UTI • Haemuturia (RBC) Renal colic (LR+ ~ 2 , LR- = 0.3) Hematuria occurs in up to 30% with AAA Most common misdiagnosis in AAA- kidney stone Plain X-rays Bowel obstruction70% sensitive Sensitive for free air 90-95% Aerobilia (RPC, GS ileus) Renal stones 90% radio-opaque GS 10% Normal X-rays does not exclude acute abdomen! Special investigations • History & examination and simple lab tests have about a 50-60 % accuracy • Technological advances in imaging are responsible for our increased accuracy in diagnosing patients with acute abdominal pain – CT – Ultrasound Imaging-Ultrasound Good first line investigation for most intra-abdominal conditons Non-invasive, no radiation Imaging-Ultrasound Biliary tract Cholecystitis Cholangitis Appendicitis Gynaecological conditions Ovarian cysts (rupture, torsion) Ectopic(TVS) Urological conditions (renal, ureteric stones, hydronephrosis) CT scan High accuracy in most acute abdominal conditions • GI Small/ large bowel obstruction Diverticulitis (hinchey grading) • Vascular AAA (esp leaking) Aortic dissection Mesenteric ischemia • Hepatobiliary Biliary tract (stones) Rupture HCC Pancreatitis Contrast Enema LB obstruction Hx and exam Baseline Ix CBC, RFT, LFT, Amylase, AXR, CXR Initial MX peritonitis Equivocal signs Operation peritonitis Serial Examination Peritonitis or condition requiring surgery No peritoneal signs or equivocal Further Ix CT/USS Def Diagnosis RX Preoperative preparation Informed consent IV antibiotics X-match Optimize comorbidities Booking of emergency OT