File
advertisement

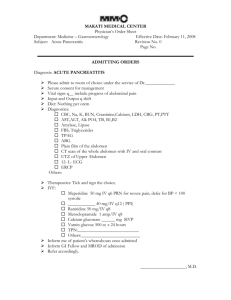
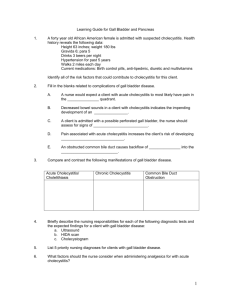
Care of Patients with Problems of the Biliary System and Pancreas Chapter 62 Mrs. Kreisel MSN, RN NU130 Adult Health Summer 2011 Hepatobiliary Anatomy Acute Cholecystitis • Acute cholecystitis is the inflammation of the gallbladder. • Calculous cholecystitis. • Cholelithiasis (gallstones) usually accompanies cholecystitis. • Acalculous cholecystitis inflammation can occur in the absence of gallstones. Gallstones Chronic Cholecystitis • Repeated episodes of cystic duct obstruction result in chronic inflammation • Pancreatitis, cholangitis • Jaundice • Icterus • Obstructive jaundice • Pruritus Clinical Manifestations • Flatulence, dyspepsia, eructation, anorexia, nausea and vomiting, abdominal pain • Biliary colic • Murphy’s sign • Blumberg’s sign • Rebound tenderness • Steatorrhea Nonsurgical Management • Nutrition therapy—low-fat diet, fat-soluble vitamins, bile salts • Drug therapy—opioid analgesic such as morphine or hydromorphone, anticholinergic drugs, antiemetic • Extracorporeal shock wave lithotripsy • Percutaneous transhepatic biliary catheter insertion Surgical Management • • • • Laparoscopic cholecystectomy Standard preoperative care Operative procedure Postoperative care: • Free air pain result of carbon dioxide retention in the abdomen • Ambulation • Return to activities in 1 to 3 weeks Traditional Cholecystectomy • Standard preoperative care • Operative procedure • Postoperative care: • Opioids via patient-controlled analgesia pump • T-tube • Antiemetics • Wound care Traditional Cholecystectomy (Cont’d) • Care of the T-tube • NPO • Nutrition therapy Cancer of the Gallbladder • Anorexia, weight loss, nausea, vomiting, general malaise, jaundice, hepatosplenomegaly; chronic, progressively severe epigastric or right upper quadrant pain • Poor prognosis • Surgery, radiation, chemotherapy Acute Pancreatitis • Serious and possibly life-threatening inflammatory process of the pancreas • Necrotizing hemorrhagic pancreatitis • Lipolysis • Proteolysis • Necrosis of blood vessels • Inflammation • Theories of enzyme activation Autodigestion Complications of Acute Pancreatitis • • • • • • Hypovolemia Hemorrhage Acute renal failure Paralytic ileus Hypovolemic or septic shock Pleural effusion, respiratory distress syndrome, pneumonia • Multisystem organ failure • Disseminated intravascular coagulation • Diabetes mellitus Clinical Manifestations • • • • • • • Generalized jaundice Cullen’s sign Turner’s sign Bowel sounds Abdominal tenderness, rigidity, guarding Pancreatic ascites Significant changes in vital signs Laboratory Assessment • • • • • • • Lipase Trypsin Alkaline phosphatase Alanine aminotransferase WBC Glucose Calcium Acute Pain • Interventions include: • The priority for patient care to provide supportive care by relieving symptoms, decrease inflammation, and anticipate and treat complications • Comfort measures to reduce pain including fasting and drug therapy • Endoscopic retrograde cholangiopancreatography Nonsurgical Management • • • • Fasting and rest Drug therapy Comfort measures Endoscopic retrograde cholangiopancreatography (ERCP) Surgical Management • Preoperative care—NG tube may be inserted • Operative procedures • Postoperative care: • Monitor drainage tubes and record output from drain. • Provide meticulous skin care and dressing changes. • Maintain skin integrity. Imbalanced Nutrition: Less Than Body Requirements • Interventions include: • NPO in early stages • Antiemetics for nausea and vomiting • Total parenteral nutrition • Small, frequent, moderate- to highcarbohydrate, high-protein, low-fat meals • Avoidance of foods that cause GI stimulation Chronic Pancreatitis • Progressive destructive disease of the pancreas, characterized by remissions and exacerbations • Nonsurgical management includes: • Drug therapy • Analgesic administration • Enzyme replacement • Insulin therapy • Nutrition therapy Pancreatic Abscess • Most serious complication of pancreatitis; always fatal if untreated • High fever • Blood cultures • Drainage via the percutaneous method or laparoscopy • Antibiotic treatment alone does not resolve abscess Pancreatic Pseudocyst • Complications: hemorrhage, infection, bowel obstruction, abscess, fistula formation, pancreatic ascites • May spontaneously resolve • Surgical intervention after 6 weeks Insulinoma • Most common type of neuroendocrine pancreatic tumor • Benign tumors of the islets of Langerhans that cause excessive insulin secretion and subsequent hypoglycemia • Management—removal of tumor Pancreatic Carcinoma • Nonsurgical management: • Drug therapy • Radiation therapy • Biliary stent insertion Surgical Management • Preoperative care: • NG tube may be inserted • TPN typically begun • Operative procedure may include Whipple procedure Surgical Management (Cont’d) • Postoperative care: • Observe for complications • GI drainage monitoring • Positioning • Fluid and electrolyte assessment • Glucose monitoring Whipple Procedure Three anastomoses that constitute the Whipple procedure: Choledochojejunostomy, pancreaticojejunostomy, & gastrojejunostomy •NCLEX TIME Question 1 A patient with chronic cholecystitis is complaining of pruritus, clay-colored stools, and voiding dark, frothy urine. Which laboratory analysis is a priority in the nurse’s assessment of this patient? A. Liver function tests B. Total bilirubin C. Lipase level D. White blood cell count Question 2 Which patient is more likely to develop gallstones? A. 55-year-old African-American male with a history of diabetes mellitus B. 62-year-old American-Indian female C. 45-year-old Caucasian female with a family history of gallstones D. 60-year-old obese, Mexican-American female with a history of diabetes mellitus Question 3 The nurse notes jaundice and bluish discoloration of the abdomen and flank in the patient complaining of abdominal pain of sudden onset that radiates to the left shoulder. Based on these symptoms, what intervention should be the priority for this patient? A. Passage of a nasogastric tube B. Observation for delirium tremens C. Pain relief D. Relief from vomiting Question 4 About how any Americans are affected by acute pancreatitis? A. 10,000 B. 30,000 C. 50,000 D. 80,000 Question 5 In the care of a patient with acute pancreatitis, which assessment parameter requires immediate nursing intervention? A. Heart rate 105 beats/min B. Blood pressure 110/82 mm Hg C. Respiratory rate 28 breaths/min D. Serum glucose 136 mg/dL