Gastroenterology
advertisement

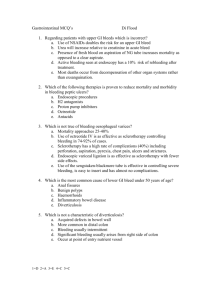
Gastroenterology Ambulatory Medicine Clerkship Scott Grisolano, MD Division of Gastroenterolgy and Hepatology KUMC Outline • Physical exam • History taking • Evaluation of abdominal pain – Common Clinical Scenarios – Differential diagnosis Physical Exam - Abdomen • Inspection – – – – Skin Hernia Contour Pulsations, peristalsis • Auscultation – Bowel sounds – Bruits • Percussion, Palpation – Liver, spleen, masses, aneurysm – Peritoneal irritation • Rigid abdomen, guarding, rebound tenderness • How was the ride to the ER? • blunted: elderly, severely ill • HEENT – Scleral icterus – Conjunctival pallor • Skin – – – – – Jaundice Spider angiomata Gynecomastia Petechiae, bruising Caput medusae • Extremities – Palmer erythema • Abdomen – HSM – Ascites • Neurological – mentation – Asterixis • Anorectal – Perianal exam – DRE – Stool Painful History • • • • • Location Onset, frequency, duration, severity Quality Radiation Factors that exacerbate or improve symptoms such as food, antacids, exertion, defecation • Associated symptoms: fevers, chills, weight, N, V, diarrhea, constipation, hematochezia, melena, jaundice, change in the color of urine or stool, change in the diameter of stool • Family history of bowel disorders • Medications: OTC (acetaminophen, aspirin, and NSAIDs) • Menstrual history in women Embryology - Pain - Artery - Organ • Foregut – Epigastrium – Celiac – S, D • Midgut – Periumbilical – SMA – J, I, TC • Hindgut – Hypogastrium – IMA – TC, R Pain • Visceral pain (viscus) – diffuse, poorly localized – gnawing, burning, cramping • Somatic pain (abdominal wall, parietal peritoneum) – more intense, better localized • Referred pain – same dermatome – sharp, well localized; resembles somatic Abdominal Pain - Triage • Acute – Sick patient? – High level of suspicion in immunosuppressed, elderly – Abdominal examination • Chronic Abdominal Pain - Triage • History – differential diagnosis • Examination – vital signs • Labs – – – – – – CBC CMP Liver biochemistries Amylase, lipase UA Pregnancy test • Abdominal x-ray Ruptured or Perforated Viscus - PUD, ectopic pregnancy, dissecting aneurysm Obstruction of Viscus - adhesions, hernia, volvulus, intussusception Ischemia - mesenteric, PE, MI Inflammation - pancreatitis, cholecystitis, appendicitis, diverticulitis Peritonitis Abdominal Pain - Triage • History – differential diagnosis • Examination – vital signs • Labs – – – – – – CBC CMP Liver biochemistries Amylase, lipase UA Pregnancy test • Abdominal x-ray RUQ Pain • Liver, biliary tree – May radiate to back, epigastrium • Pancreatitis • Cardiac • Pleural/pulmonary • Nephrolithiasis Epigastric Pain • Acute pancreatitis • PUD • GER • Cardiac • Pleural/pulmonary Lower Abdominal Pain • Distal intestinal tract • Urinary tract • Pelvic structures – Colonic, SB source = diarrhea, hematochezia – Rectal source = urgency, tenesmus Lower Abdominal Pain • LLQ – Diverticulitis – Colitis • Infectious, ischemic, IBD • RLQ – Appendicitis – ileocolitis Lower Abdominal Pain • Females – Menses, dysmenorrhea, dyspareunia – Possibility of pregnancy – Vaginal discharge, bleeding – Adnexal cysts – Ovarian torsion – Ectopic pregnancy – PID Specific Conditions • • • • • PUD Gallbladder disease Acute pancreatitis Small bowel obstruction GI bleeding Specific Conditions • • • • • PUD Gallbladder disease Acute pancreatitis Small bowel obstruction GI bleeding PUD • Duodenal ulcer – symptoms of occur when acid is secreted in the absence of a food buffer – symptoms occur 2-5 hours after meals or on empty stomach • Gastric ulcer – more severe pain occurring soon after meals, with less frequent relief by antacids or food PUD • Epigastric pain in 2/3 symptomatic patients – may localize to the RUQ, LUQ – burning, gnawing, or hunger-like in quality, may be vague • Sudden development severe, diffuse abdominal pain may indicate perforation • Vomiting is the cardinal feature in pyloric outlet obstruction • Hemorrhage may be heralded by nausea, hematemesis, melena, or dizziness PUD - Etiology • Helicobacter pylori • NSAIDs < 5% 30-50% Alarm Symptoms / Red Flags • • • • • • • • • Age > 50 Weight loss Dysphagia Persistent vomiting Palpable abdominal mass Occult gastrointestinal bleeding Otherwise unexplained anemia Family history UGI malignancy Previous gastric surgery Specific Conditions • • • • • PUD Gallbladder disease Acute pancreatitis Small bowel obstruction GI bleeding Gallbladder • Biliary colic – Pain reaches crescendo then resolves completely – Pain is visceral in origin (no true gallbladder wall inflammation) – Pain resolves when the gallbladder relaxes, permitting stones to fall back from the cystic duct • Acute cholecystitis – RUQ pain lasting > 4-6 hours should raise suspicion for acute cholecystitis – Symptoms of malaise, fever more likely Cholecystitis – Clinical Presentation • Abdominal pain – RUQ, epigastrium – may radiate to the right shoulder or back • Pain is steady and severe – nausea, vomiting, and anorexia • Prolonged RUQ pain (> 4-6 hours), especially if associated with fever, should arouse suspicion for acute cholecystitis as opposed to an attack of simple biliary colic Differential Diagnosis • • • • • • • Acute pancreatitis Appendicitis Acute hepatitis Peptic ulcer disease Diseases of the right kidney Right-sided pneumonia Fitz-Hugh-Curtis syndrome – perihepatitis caused by gonococcal infection • Sub-hepatic, intra-abdominal abscess • Perforated viscus • Cardiac ischemia Cholecystitis – Labs • Bilirubin, AP generally normal in uncomplicated cholecystitis – biliary obstruction is limited to the gallbladder • If bilirubin, AP elevated this should raise concerns about complicating conditions such as cholangitis, choledocholithiasis – mild elevation in serum aminotransferases and amylase, and hyperbilirubinemia with jaundice have been reported even in the absence of these complications • These abnormalities may be due to the passage of small stones, sludge, or pus Cholecystitis – Physical Exam • Ill appearing, febrile, and tachycardic • Lie still on exam table because cholecystitis is associated with local parietal peritoneal inflammation that is aggravated by movement • Abdominal examination usually demonstrates voluntary and involuntary guarding • "Murphy's sign" may be a useful diagnostic maneuver Acute Calculous Cholecystitis Specific Conditions • • • • • PUD Gallbladder disease Acute pancreatitis Small bowel obstruction GI bleeding Acute Pancreatitis - Etiology • Gallstones (45%) 80% • Alcohol abuse (35%) • Post-ERCP, medications, metabolic, hereditary, infectious, connective tissue disease, trauma, congenital anatomic abnormalities, tumors (10%) • Idiopathic (10%) • Overall mortality 10 -15% – severe disease as high as 30% • Males (alcohol) > Females (choledocholithiasis) Acute Pancreatitis – Clinical Presentation • Mid-epigastric abdominal pain – Steady, boring pain – Radiation to the left upper back • Anorexia, nausea vomiting diarrhea • Low grade fever • Presentations associated with complications – Shock – Multi-system failure Acute Pancreatitis – Physical Exam • • • • • • Abdominal tenderness Fever (76%) Abdominal guarding (68%) Abdominal distension (65%) Tachycardia (65%) Hypoactive bowel sounds • • • • • • • Jaundice (28%) Dyspnea (10%) Hemodynamic changes (10%) Melena or hematemesis (5%) Cullen’s sign The Grey-Turner sign Left pleural effusion Acute Pancreatitis - Diagnosis • Serum amylase – Not specific for pancreatitis • intestinal ischemia, renal insufficiency, small bowel obstruction, macroamylasemia, parotitis – Short half-life: elevates early, returns to normal early (within 2-3 days) • Serum lipase – More specific to pancreas – Long half-life: levels rise later, stay elevated for longer (7-14 days) • Liver enzymes – ALT, AST, alkaline phosphatase, total bilirubin – ALT > 150 in patient with cholelithiasis suggests gallstone pancreatitis Acute Pancreatitis - Diagnosis • Ultrasound – Most useful initial test for common bile duct dilation and gallstones • Contrast CT Scan – Not necessary for diagnosis of acute pancreatitis – May help identify etiology in rare instances (tumor) – Useful to assess complications - fluid collections or pancreatic necrosis Pseudocyst - takes > 4 weeks to develop pseudocyst Acute Pancreatitis - Severity Staging Ranson Criteria - > 3 indicates severe AP • At Admission – Age > 55; WBC > 16K; Glucose > 200; LDH >350; AST > 250 • During first 48 hours – – – – – Hct decrease by > 10% with hydration BUN increase > 5 mg/dL Calcium < 8 mg/dL pO2 < 60 mm Hg Evidence of fluid sequestration (> 6L replacement needed) Specific Conditions • • • • • PUD Gallbladder disease Acute pancreatitis Small bowel obstruction GI bleeding Small Bowel Obstruction • Post-operative adhesions • Hernia • Tumors SBO - Symptoms • Abdominal distention, vomiting, crampy pain • Abdominal pain – Periumbilical, crampy – paroxysms of pain every 4-5 minutes – presence of constant abdominal pain or change of pain from colicky to constant suspect strangulation • Patients may or may not complain of obstipation and inability to pass flatus since colon requires 1224 hours to empty after the onset of bowel obstruction SBO – Physical Exam • Fever, tachycardia: associated with strangulation • Inspection – surgical scars, degree of distention • Auscultation – may reveal high-pitched or hypoactive bowel sounds • Percussion, Palpitation – Tenderness to percussion, rebound, guarding, and localized tenderness suggests peritonitis – Tympany usually present due to air-filled loops of bowel or stomach – abdominal mass may indicate an abscess, volvulus, or tumor – Search for inguinal, femoral, and incisional hernias • Rectal examination – gross or occult blood can be found with neoplasm, ischemia, and intussusception. SBO – Labs • Leukocytosis: may indicate presence of strangulation • Metabolic alkalosis: seen with frequent emesis • Metabolic (lactic) acidosis: ischemic bowel SBO – X-rays • Upright chest film to rule out the presence of free air • Supine and upright abdominal films – Multiple air-fluid levels with distended loops of small bowel are seen in small bowel obstruction, although occasionally can be seen in setting of paralytic ileus • Presence of air in the colon or rectum makes the diagnosis of complete obstruction less likely, particularly if symptoms have been present for more than 24 hours • Plain films: – equivocal in 20-30% of patients – normal, nonspecific in 10-20% SBO – CT scan • Presence, level (transition point), severity, and cause may be identified • Other abdominal pathology can be detected • Absence of air, fluid in distal small bowel or colon denotes complete obstruction • Intestinal pneumatosis and hemorrhagic mesenteric changes can be seen in advanced strangulation • In most cases of SBO, no obvious source of obstruction is seen, since adhesions cannot be detected by CT scan SBO - Management • "never let the sun rise or set on a small bowel obstruction" Specific Conditions • • • • • PUD Gallbladder disease Acute pancreatitis Small bowel obstruction GI bleeding All bleeding is not the same… • • • • • Where is it coming from? Pace of bleeding? Volume of bleeding? Associated symptoms? Color of blood? What color blood? • Melena • Hematochezia • Occult blood positive Acute GI Bleeding UPPER > 75-80% vs. LOWER 20-25% Acute GI Bleeding • Assessment, stabilization, resuscitation • Medication review – Anticoagulants (Coumadin) – Antiplatelet agents (Plavix) – Aspirin, NSAIDs Clinical Prognostic Factors Older age (>60) Severe comorbidity Altered hemodynamics - Tachycardia - Orthostasis Transfusion > 100 bpm > 20 mg Hg systolic > 10 mg Hg diastolic - 4 - 6 units/resuscitation event Severe coagulopathy Inpatient status at time of bleed UGI Bleeding • EGD – Diagnosis • identifies bleeding site (90-95%) • prognostic value – Endoscopic Therapy • Medical Therapy – IV Proton Pump Inhibitors (PPIs) – octreotide Active Bleeding - Dieulafoy Lesion 90% Esophageal Varices LGI Bleeding • LGIH accounts for 20-25% of all GI bleeds • Definition: distal to the ligament of Treitz • Colonic lesions account for vast majority • Majority cease without intervention • 15-20% require intervention LGIB - Etiology * post-polypectomy bleeds LGI Bleeding • Urgent Colonoscopy – After rapid oral purge – Diagnosis • identifies bleeding site 54-80% – Treatment • epinephrine, heater probe, bipolar, hemoclips Diverticular Bleed Post-polypectomy - NBVV Ischemic Colitis