INPATIENT MANAGEMENT OF DIABETIC KETOACIDOSIS
advertisement

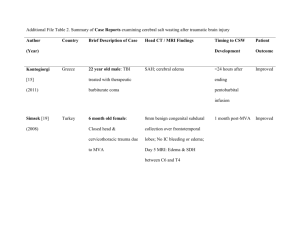
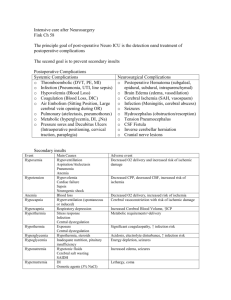
Guidelines for the Early Management of Diabetic Ketoacidosis in Children Michael Bressack, MD DEFINITION Hyperglycemia (serum glucose >300 mg/dl) with glycosuria Metabolic acidosis (serum bicarbonate <15, elevated anion gap, pH <7.30) Ketonemia with ketonuria CLINICAL PRESENTATION HYPERGLYCEMIA Polyuria Polydipsia Weight loss Dehydration/shock Decreased level of consciousness CLINICAL PRESENTATION METABOLIC ACIDOSIS Kussmaul breathing Fruity breath (acetone) ? decreased level of consciousness ? depressed cardiac function ? intestinal ileus (vomiting, pain) LABORATORY DATA Hyperglycemia Metabolic acidosis (anion gap) [Na+]-([Cl-]+[HCO3-]) OH butyrate Low [Na+] [Nac+] = [Nam+] + 1.6(blood glucose-100) 100 LABORATORY DATA Hyperglycemia Metabolic acidosis (anion gap) [Na+]-([Cl-]+[HCO3-]) OH butyrate Low [Na+] Abnormal [K+] Pre-renal azotemia MONITORING Blood glucose q 1 h - q 4 h Electrolytes q 1 h - q 4 h Anion gap q 1 h - q 4 h Renal function q 4 h – q 6 h Cardiac monitor/EKG CLINICAL MONITORING Cardiovascular Intake/urinary output Neurologic status (Glasgow Coma Scale) CARDIOVASCULAR TREATMENT Treat shock immediately 10-20 ml/kg doses of NS or LR Slow rehydration for 5-15% deficit over 48 hours SLOW REHYDRATION Maintenance, deficit, excessive urine (because of the risks of cerebral edema, infuse fluid at a maximal rate of 1.5 to 2 times maintenance) Normal saline is usually the best initial fluid (avoid hypotonic fluid) Follow [Na+] closely (keep [Na+corrected] 135meq/l) TREATMENT FOR HYPERGLYCEMIA / KETOACIDOSIS Rehydration lowers blood glucose Low-dose continuous insulin (.05 - 0.1 u/kg/hr) IV bolus of insulin is not necessary CONTINUOUS INSULIN DRIP Decrease blood glucose 50-100 mg/dl/hr (after the initial drop due to rehydration) Add glucose to intravenous fluid when blood glucose <250-300 mg/dl add glucose to maintenance fluids only Increases bicarbonate and decreases anion gap (takes longer to correct ketoacidosis than hyperglycemia) use enough insulin to correct the anion gap acidosis, and add enough glucose to the intravenous fluid to tolerate the insulin TREATMENT FOR K+ Usually hyperkalemia on presentation Total body K+ deficit Monitor EKG Initiate K+ replacement when serum level <5.5meq/l and adequate urine output In the rare situation of hypokalemia at presentation, immediately treat with K+ replacement and fluid therapy, but delay insulin treatment until K+ >3.3meq/l INDICATION FOR BICARBONATE Life-threatening hyperkalemia Bicarbonate has no place in the management of DKA Cerebral edema is a medical emergency (major cause of death in pediatric DKA) Causes of Morbidity/Mortality in DKA Cerebral edema/dysfunction (80-90% of deaths) Shock/ischemia Hyper/hypokalemia Hypoglycemia Sepsis ARDS Thrombosis Central venous catheters are particularly prone to thrombosis. If used, prophylaxis with low-dose heparin should be considered. Cerebral Edema/CNS Dysfunction Clinical cerebral edema occurs in 0.5-0.9% of all episodes of DKA and accounts for 57-87% of all DKA deaths A clinical, not a radiological, diagnosis (e.g. CNS dysfunction does not correlate with CT changes) Mortality ~25% (respiratory arrest on presentation has the worst prognosis) Significant morbidity in survivors (~25%) Morbidity/mortality from herniation Major cause of death in DKA Occurs nearly exclusively in patients <20 years old More common in: younger children children who have a longer duration of DKA before treatment children with newly diagnosed diabetes elevated initial BUN low initial pCO2 rapid administration of hypotonic fluids failure of corrected serum sodium to rise during treatment treatment with bicarbonate Occurs within first 24 hours after starting Rx (usually 4-12hrs) Signs and Symptoms of Cerebral Edema Headache, emesis Lethargy, incoherence, agitation, incontinence, coma Seizures Sudden, persistent bradycardia (decline >20bpm) not attributable to improved intravascular volume or sleep state Abnormal neurogenic respiratory pattern (e.g. tachypnea, Cheyne-Stokes respiration, apneusis) Decreasing Glasgow Coma Scale Cranial nerve palsy (e.g. III, IV, VI) Cushing’s reflex (e.g. hypertension) Decorticate / decerebrate posturing Cardiopulmonary arrest Etiology of Cerebral Edema Cerebral edema due to osmotic shift of fluid Primary ischemia/hypoxia with secondary cerebral edema Prevention and Treatment of Cerebral Edema Cardioplumonary stabilization on presentation fluid boluses of isotonic crystalloids for shock intubation/ventilation for respiratory failure After acute therapy for shock, avoid excessive fluid or hypotonic fluid (use only 0.45%saline or normal saline) Avoid medications that can mask intracranial hypertension e.g. phenergan, benzodiazepines Promptly give intravenous mannitol (0.51.0gm/kg) or 3% saline (5-10ml/kg) for clinical signs of elevated ICP Consider intubation for neurologic deteriorationrisks include pCO2, which can elevate ICP, and pCO2, which causes cerebral ischemia