Right - Home
advertisement

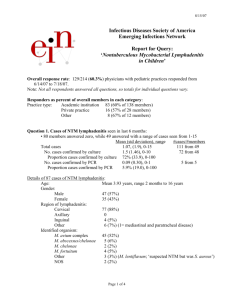
Lymphadenitis Amina Ahmed, MD Levine Children’s Hospital November 17, 2011 Definitions Lymphadenopathy Lymph node enlargement Infectious, inflammatory or neoplastic Lymphadenitis Localized inflammatory process Unilateral, bilateral Acute or chronic Pyogenic or granulomatous Lymphadenopathy Most healthy children have palpable lymph nodes Considered enlarged if > 10 mm > 5 mm epitrochlear is abnormal > 15 mm inguinal is abnormal Palpable supraclavicular nodes in the absence of cervical adenopathy are abnormal Palpable popliteal nodes are abnormal Lymphatic Drainage of Nodes Lymph Node Group Area of Drainage Potential Etiologies Occipital Back of scalp/neck Tinea capitis Seborrheic dermatitis Rubella Preauricular Lateral eyelids Lateral conjuctivae Skin above cheek Adenovirus Parinaud’s syndrome due to CSD, tularemia, HSV Axillary Hand, arm Chest wall, breast CSD Epitrochlear Ulnar aspect hand and forearm Local pyogenic infection CSD, tularemia Popliteal Lateral foot, lower leg, knee joint Local pyogenic infection Lymphatic Drainage of Head and Neck Lymph Node Group Area of Drainage Occipital Back of scalp/neck Submental Central lower lip, floor of mouth, skin of chin Submandibular Buccal mucosa, side of nose, medial palpebral commisure, upper lip, anterior tongue Superior deep cervical Occipital scalp, auriculae, back of tongue, trachea, thyroid, esophagus Inferior deep cervical Dorsal scalp and neck, superfical pectoral region, superior deep cervical nodes Supraclavicular Right: left lower lobe, lingula, right lung Left: left upper lobe, abdomen Infectious Causes of Lymphadenopathy in Children Location of Affected Nodes Cause Bacterial Cervical Mediastinal Abdominal S aureus S. pyogenes M. tuberculosis NTM B. henselae Anaerobic bacteria Yersinia F. tularensis Syphilis Epstein-Barr virus Cytomegalovirus Herpes simplex Adenovirus Human immunodeficiency virus Human herpes virus 6 Rubella Parasitic Histoplasmosis Sporotrichosis Coccidioidomycosis Blastomycosis Toxoplasmosis Coxsackie Fungal Brucellosis Viral Generalized Noninfectious Causes of Lymphadenopathy in Children Location of Affected Nodes Cause Malignancy Cervical Mediastinal Abdominal Generalized Hodgkin's Disease Non-Hodgkin’s Lymphoma Leukemia Thyroid tumors Neuroblastoma Metastatic disease Lymphoproliferative disorders Other Parotid tumors Immunodeficiency diseases Collagen vascular disease Sarcoidosis Congenital Rhabdomyosarcoma Kawasaki syndrome Histiocytosis X Storage disorders Serum sickness Branchial cleft cyst Cystic hygroma Bronchogenic cyst Thyroglossal duct cyst Epidermoid cyst Etiology of Lymphadenitis History Duration of illness Skin lesions or trauma Epidemiology Age, ethnicity Travel, pets Physical examination Dental disease Ocular or oropharyngeal lesions Noncervical adenopathy Hepatomegaly or splenomegaly Infectious Causes of Lymphadenitis Acute bilateral cervical lymphadenitis Response to pharyngitis Part of generalized lymphoreticular response Acute unilateral lymphadenitis Pyogenic bacterial infection Subacute or chronic lymphadenitis Acute Bilateral Cervical Lymphadenitis Pharyngitis S. pyogenes Viral upper respiratory tract infections Epstein-Barr virus Cytomegalovirus Herpes simplex Adenoviral syndrome HIV Enterovirus HHV-6 Rubella Pyogenic Lymphadenitis Acute (< 2 weeks duration) S. aureus Streptococcus pyogenes, S. agalactiae Francisella tularensis Pasteurella multocida Yersinia pestis Subacute (≥ 2 weeks duration) Bartonella henselae Non-tuberculous mycobacteria (NTM) M. tuberculosis Toxoplasmosa gondii Pyogenic Causes of Adenitis Organism S. pyogenes S. agalactiae S. aureus NTM B. henselae T. gondii Anaerobes Neonate 2 mo – 1y 1-4 y 5-18 y - - + ++ ++ + - - + ++ ++ + - - ++ + - + ++ ++ - - + + - - + ++ Principles and Practice of Infectious Disease; Long S, ed. Acute Unilateral Cervical Lymphadenitis S. pyogenes Associated with impetigo or streptococcosis Lymphangitis more common with GAS S. aureus Longer duration of disease before diagnosis More likely to suppurate, longer time to resolution Subacute Lymphadenitis Approximately 2-3 week duration Painless or minimally tender Discoloration of overlying skin may occur Suppuration and drainage may occur Subacute Lymphadenitis Cat-scratch disease (B. henselae) Toxoplasmosis Mycobacteria Nontuberculous mycobacteria (NTM) Tuberculosis BCG adenitis Tularemia (F. tularensis) Typically increasing adenopathy, suppuration Case 1 : Red Neck 3 week old with fever and submandibular swelling with erythema Evaluation? Empiric treatment? Case 1 : Red Neck Differential GBS S. aureus Evaluation Blood culture LP Empiric treatment Ampicillin Nafcillin Vancomycin GBS Cellulitis-Adenitis Syndrome Late-onset GBS disease Typically 2-11 weeks of age Abrupt onset of fever and facial or submandibular swelling Ipsilateral OM Bacteremia in 90% of cases Meningitis in 25% Case 2 : When Antibiotics Fail 23 month old admitted with submandibular adenitis Treated with amoxicillinclavulanate for 7 days without improvement Temperature 101.9 Case 2 Differential diagnosis Acute adenitis S. aureus MSSA, MRSA S. pyogenes Empiric treatment Further management Cervical Adenitis: S. aureus, S. pyogenes Account for 40-80% of cases of acute cervical adenitis Most common in 1-4 y of age Recent URI- pharyngitis, tonsillitis, AOM Primary sites Submandibular (50-60%) Upper cervical (25-30%) Submental (5-8%) ~ 25% suppurate (mainly S. aureus) Management of Acute Cervical Adenitits Empiric therapy for S. aureus, S. pyogenes (7-10 d) No improvement ? MRSA, ? anaerobes consider aspiration Broaden antimicrobial coverage ? Suppuration (abscess) US or CT Drainage, excision No improvement subacute ? CSD B. henselae titers ? NTM MSSA versus MRSA MSSA -lactamase production Only 5% susceptible to penicillin Susceptible to semisynthetic penicillins and cephalosporins MRSA Altered PBP2a Resistant to all -lactam antibiotics Susceptible to vancomycin, clindamycin (variable) Antimicrobial Treatment of MRSA Macrolides Increasing resistance- not reliable Clindamycin Used widely Inducible resistance; increasing resistance TMP-SMX Not FDA approved; limited experience Not active against GAS Susceptibility rates high Add rifampin for large lesions, -lactam for GAS Rifampin Susceptibility high Use only in combination with other agents Tetracyclines Not approved in pediatric patients Linezolid Expensive Save it! Fluoroquinolones Resistance increasing Not approved in prepubertal children Case 3 : All in the Family 8 y old girl referred to hematology-oncology for evaluation of inguinal adenopathy Node present for 3 weeks Tender only when walking Family went camping 2 weeks before onset Father and sister also had adenopathy Case 3 Subacute adenitis B. henselae Toxoplasmosis NTM, MTB F. tularensis Evaluation Management Cat-Scratch Disease Etiologic agent is Bartonella henselae Approximately 25,000 cases annually in US Cats are the reservoirs and the vectors 10-30% cats are bacteremic (kittens > cats) Flea transmission from cat to cat > 90% of patients have had contact with a cat 50-80% have been scratched Cat-Scratch Disease Overview of 1,200 patients with CSD 87% < 18 y 85% with single node Noncontiguous adenopathy in 2% Suppuration in 12% Other family members affected in 3.5% 60 had atypical disease Am J Dis Child 1985; 139: 1124-33 Clinical Presentation of 2,083 Patients with CSD Clinical features Numbers Percentage 1784 86 1271 61 299 14 Parinaud’s oculoglandular syndrome 125 6.1 Encephalopathy 51 2.4 Systemic disease, severe, chronic 48 2.3 Neuroretinitis 30 1.4 Erythema nodosum 15 0.7 Thrombocytopenic purpura 7 0.3 Hepatosplenomegaly 7 0.3 Osteomyelitis 8 0.3 Typical presentation Inoculation lesion (skin, eye mucous membrane) Atypical manifestations Curr Infect Dis Rep 2000; 2: 141-46 Lymphadenitis : Typical CSD Primary lesion at site of inoculation Papule vesicle crusting in 1-4 weeks May be resolved at presentation of adenitis Lymphadenitis 5 d to 2 mo after inoculation Solitary (50%) or regional (50%) Axillary > cervical > submandibular Minimal tenderness Overlying skin not warm or erythematous Constitutional symptoms in 25-50% Regresses in 4-8 weeks Location of Lymphadenopathy in Patients with CSD Location No. (%) of Patients Total upper extremity Axillary Epitrochlear 610 (46.1) 586 24 Total neck and jaw Cervical Submandibular 340 (26.1) 191 149 Total groin Inguinal Femoral Preauricular Postauricular Clavicular Chest 228 (17.5) 143 85 87 (6.6) 2 31 4 Diagnosis of Cat-Scratch Disease Clinical Serology IgG ≥ 1:64 is seroreactive IgG ≥ 1:512 or 4 fold increase is diagnostic Absence of IgM does not exclude diagnosis Diagnosis of Cat-Scratch Disease Histology Necrotizing granulomas Warthin Starry silver stain may detect organisms Isolation of B. henselae is difficult PCR for tissue in research settings Management of Typical CSD Antibiotics not recommended for mild to moderately ill immunocompetent patient Self-limited; resolves in 2-3 mo Consider treatment for large, bulky nodes Azithromycin? Doxycycline? Surgical excision is not necessary for diagnosis or management Treatment of Cat-Scratch Disease In vitro susceptibility to multiple antibiotics Clinically response to antibiotics is minimal Anectodal reports suggest response to: TMP-SMX Rifampin Ciprofloxacin Gentamicin Pediatr Infect Dis J 1992: 11: 474-8 Azithromycin for CSD Randomized, double-blind, placebo-controlled trial 14 treated with azithromycin 15 treated with placebo In 7/14 azithromycin and 1/15 placebo-treated patients, 80% reduction in node volume at 30 d -Difference not significant after 30 d Clinical outcome not otherwise different Pediatr Infect Dis J 1998; 17: 447-52 Here…Kitty, Kitty! 8 year old boy being evaluated in GI Clinic for constipation 2 week history of rash and lymphadenopathy in neck and axilla Grandmother had brought home a kitten… Case 4 : Lump in my throat A 2 year old presents with cervical lymphadenitis. She is afebrile and otherwise asymptomatic After a 10 days of amoxicillin and 10 days of amoxicillin-clavulanate, the lymphadenitis is unchanged A TST is reactive at 8 mm. The patient’s CXR is normal. How do you proceed with further management? Case 4 Subacute (≥ 2 weeks duration) Bartonella henselae Non-tuberculous mycobacteria (NTM) Mycobacterium tuberculosis Toxoplasmosa gondii (MTB) Further evaluation Mycobacterial Lymphadenitis M. tuberculosis complex M. tuberculosis M. bovis Nontuberculous mycobacteria (NTM) Most common M. avium complex NTM versus MTB Lymphadenitis NTM lymphadenitis much more common than MTB Similar clinical presentation TST may be reactive in either CXR may be normal in TB Histologically identical Differentiation requires isolation of pathogen MTB Lymphadenitis All ages Localized adenopathy (scrofula) Supraclavicular, cervical, submandibular Systemic symptoms minimal Generalized adenopathy Cervical, supraclavicular Systemic symptoms present Primary pulmonary focus on CXR in 30-70% Treatment is chemotherapy NTM Lymphadenitis Immunocompetent children 1-4 y of age Portal of entry is usually oropharynx or skin Cervical adenitis - most common manifestation of NTM infection Unilateral anterior cervical or submandibular Skin characteristically becomes violaceous Pain and constitutional symptoms minimal 50% suppurate, 10% drain Excision is the treatment of choice Do not incise and drain If not amenable to surgery- dual or triple drug treatment NTM versus MTB Lymphadenitis TST < 15 mm, CXR normal, no reactive TSTs in household- more likely NTM Excision for diagnosis and treatment If reactive TSTs in household Aspiration or excision for diagnosis Evaluation for TB in patient and sources Diagnosis of NTM Lymphadenitis Excision of node is the treatment of choice and provides clues to diagnosis Necrotizing granulomas AFB stains may be positive Definitive diagnosis and differentiation from TB requires isolation by culture NTM Lymphadenitis RCT of surgical excision versus antibiotic therapy Diagnosis by culture or PCR 50 children- surgery 50 children- clarithromycin/rifabutin for 12 wks Cure rate of 96% for surgery versus 66% for antibiotics Surgical excision is more effective than antibiotic treatment for children with NTM cervical adenitis Clin Infect Dis 2007; 4: 1057-64 Management of NTM Lymphadenitis Excision is the treatment of choice DO NOT INCISE AND DRAIN! DO NOT FORGET TO CULTURE! Lymphadenopathy not amenable to excision Experience with clarithromycin or azithromycin in combination with ethambutol and rifabutin DO NOT USE SINGLE AGENT THERAPY! Case 5 : Who Dunnit? 9 year old with ulcerative lesion of ring finger and painful elbow Patient reports cutting finger while picking up glass MRI shows multiple epitrochlear nodes No response to cefazolin Case 5 Epitrochlear adenitis S. aureus, S. pyogenes B. henselae F. tularensis Patient later reported being licked by a cat…or maybe bitten by a cat Tissue culture growing gramnegative rods Tularemia Etiologic agent is Francisella tularensis 100-200 cases per year in the United States Transmission Ticks Contact with rabbits Contact with rodents/domestic animals Poorly cooked road kill or game meats Tularemia Cutaneous inoculation (papule) ulcer regional nodes bacteremia Most common sign is regional adenopathy Inguinal most common in adults; cervical in children Untreated, nodes suppurate and drain Constitutional symptoms common in children Fever in 80-90% Malaise, chills, fatigue Clinical Forms of Tularemia Clinical Manifestation Features Glandular Most common manifestation (50-80%) May have papule or ulcer distal to node Multiple or groups of nodes Oculoglandular Nodular conjunctivitis Preauricular adenopathy Oropharyngeal Diphtheria-like illness; fever Typhoidal Ingestion of contaminated food Sepsis-like manifestation Pneumonia Aerosol exposure Rare in children Diagnosis of Tularemia Serology IgG > 1:160 is presumptive 4 fold increase is diagnostic Histology Follicular hyperplasia, caseating granulomas Isolation from tissue, blood, sputum Biosafety level 2 required for isolation Case 6 : Like mother, like daughter 16 year old Vietnamese girl with cervical adenitis Referred to pulmonologist TST placed referred to surgeon CXR normal MRI of chest shows mediastinal adenopathy NTM versus MTB Lymphadenitis Approach to child with suspected TB adenitis: Risk factors for TB (contact, country of origin, etc.) TST CXR Needle biopsy or excision for culture Specimens from other sites for culture Approach to child with adenitis, reactive TST: Investigation of household with TSTs CXR Needle biopsy or excision for culture M. tuberculosis Adenitis Most frequent form of extrapulmonary disease (30-60%) More common in Asians, females Localized or part of more generalized process Typically unilateral, supracalvicular or cervical node Painless, red, firm CXR frequently normal Diagnosis FNA versus excisional biopsy (with cultures!) PCR (tissue, PBMC)- variable yield Treatment- as for MTB Management of Acute Lymphadenitis Empiric therapy for S. aureus, S. pyogenes Consider local susceptibilities If no response to treatment Symptomatic consider parenteral therapy ? Abscess drainage needed Subacute node consider NTM, CSD B. henselae serology TST, CXR CBC with differential Management of Acute Lymphadenitis Further evaluation US Needle aspiration Biopsy Excisional preferred to incisional if unsure of diagnosis Early if malignancy suspected Management of Subacute Adenitis Evaluation for alternate infectious etiologies CSD- Bartonella titers NTM or MTB- TST, CXR Toxoplasmosis serology Diagnosis usually made by biopsy FNA or biopsy for diagnosis Treatment of Lymphadenitis Possible Pathogens Empiric treatment S. aureus/ S. pyogenes Cellulitis, symptoms With suppuration Clindamycin, vancomycin Incision and drainage S. agalactiae/S.aureus Nafcillin, clindamycin, vancomycin S. agalactiae- penicillin, ampicillin Anaerobes Add clindamycin or metronidazole B. henselae Symptomatic; consider azithromycin NTM Excision of node M. tuberculosis Four-drug antituberculosis regimen F. tularensis Gentamicin, streptomycin Content Specifications Covered Recognize the clinical manifestations of cat-scratch disease, including FUO Formulate a differential diagnosis in a patient with suspected CSD, (eg, nontuberculous myocobacterial infection, tuberculosis, sarcoidosis) Know how to diagnose CSD Know the epidemiology of CSD (ie, recent contact with cats, often kittens) Know how to identify and interpret a positive TST Understand the diagnosis and treatment of cervical adenitis secondary to NTM Know the major clinical manifestations of NTM in immunocompetent children Identify the clinical manifestations of Toxoplasma gondii infections acquired after birth Case : TB or not TB? 2 year old Hispanic female with neck swelling Treated 2 weeks with antibiotics with no improvement New node noted in region Referred to a surgeon Surgeon recommended medical management TST reactive at 12 mm Case : TB or not TB? Subacute adenitis Pyogenic abscess? CSD NTM MTB Tularemia Anaerobes Acid fast bacilli Denoument Differentiation between NTM and MTB adenitis requires isolation of the pathogen Caseating granulomas identified AFB noted on histology Treatment initiated Isoniazid, rifampin, pyrazinamide, ethambutol MTB isolated Resistance to PZA pasteurized got milk? Mycobacterium bovis Causative agent of TB in cattle Transmission Ingestion of unpasteurized milk products Aerosolization, inoculation Cow cow, cow human, human cow Rare cause of TB in industrialized countries < 0.1% of TB in the United States Case • 14 year old with 1-2 week history of fever, sore throat • Swelling of neck in last 3 days • Admitted for difficulty swallowing and dehydration Case Acute bilateral cervical adenopathy S. pyogenes Viral EBV CMV Adenovirus Evaluation Treatment Infectious Mononucleosis : EBV Seroprevalence 50% to 90% among 5 year olds Primary infection in children subclinical In adolescence, 30-50% symptomatic Pharyngitis, cervical adenopathy are hallmarks Posterior cervical, anterior cervical Diagnosis Heterophile antibody Not useful in children < 4 y or EBV titers Case 13 year old with submental adenitis Fever, toxic appearing Vancomycin and ceftriaxone initiated Blood culture: GNR Acute Lymphadenitis: Anaerobes Most frequent in older children /adolescents Poor dentition or periodontal disease Anaerobes isolated in up to 38% of aspirates from children with optimal culture techniques Acute Lymphadenitis: Anaerobes Can lead to septic thrombophlebitis of jugular veins, septic pulmonary emboli Lemierre syndrome Bull neck Systemic toxicity Positive blood cultures (Fusobacterium)