C - Emerging Infections Network - Infectious Diseases Society of
advertisement

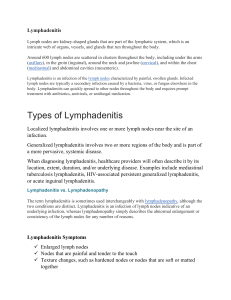
8/15/07 Infectious Diseases Society of America Emerging Infections Network Report for Query: ‘Nontuberculous Mycobacterial Lymphadenitis in Children’ Overall response rate: 129/214 (60.3%) physicians with pediatric practices responded from 6/14/07 to 7/18/07. Note: Not all respondents answered all questions, so totals for individual questions vary. Responders as percent of overall members in each category: Practice type: Academic institution 83 (60% of 138 members) Private practice 16 (57% of 28 members) Other 8 (67% of 12 members) Question 1. Cases of NTM lymphadenitis seen in last 6 months: • 80 members answered zero, while 49 answered with a range of cases seen from 1-15 Mean (std deviation), range #cases/#members Total cases 1.07, (1.9), 0-15 111 from 49 No. cases confirmed by culture 1.5 (1.46), 0-10 72 from 48 Proportion cases confirmed by culture 72% (33.9), 0-100 No. cases confirmed by PCR 0.09 (0.30), 0-1 5 from 5 Proportion cases confirmed by PCR 5.9% (19.0), 0-100 Details of 87 cases of NTM lymphadenitis: Age: Mean 3.93 years, range 2 months to 16 years Gender: Male 47 (57%) Female 35 (43%) Region of lymphadenitis: Cervical 77 (88%) Axillary 0 Inguinal 4 (5%) Other 6 (7%) (1= mediastinal and paratracheal disease) Identified organism: M. avium complex 45 (52%) M. abscessus/chelonae 5 (6%) M. chelonae 2 (2%) M. fortuitum 4 (5%) Other 3 (3%) (M. lentiflavum; ‘suspected NTM but was S. aureus’) NOS 2 (2%) Page 1 of 4 8/15/07 Treatment: Surgery Antibiotics Both PPD status: Negative Positive Not done Race/ethnicity: Non-hispanic white Hispanic white Black Asian 27 (32%) 14 (16%) 44 (52%) 57 (67%) 15 (18%) 13 (15%) 59 (69%) 15 (18%) 10 (12%) 1 (1%) Question 2: The incidence of NTM lymphadenitis is: Not changing 73 (71%) Increasing 16 (15%) Decreasing 14 (14%) Question 3: What percent of suspected NTM cases are confirmed by (answered by 91 members): Mean, median (std deviation), range Tissue culture 66.2%, 70% (27.2), 0-100 Tissue PCR 5.6%, 0% (14.5), 0-100 Not confirmed 29.5%, 25% (26.6), 0-100 Question 4. Treatment – What percent of your NTM cases are: Undergo surgical excision 79.0%, 90% (24.7), 0-100 Require adjunctive antibiotics 40.2%, 30% (36.1), 0-100 Treated with antibiotics alone 18.7%, 5% (25.9), 0-90 Require repeat surgery 8.9%, 5% (12.2), 0-66.7 Comments about mycobacterial lymphadenitis or this survey: Treatment, specific case information • Combination antibiotic therapy is more effective than single agent. Surgery is more effective than antibiotic therapy • Surgery only a last-resort • We usually get patients referred by ENT as their node is in the facial nerve distribution • Most of my ENT colleagues will not remove the involved nodes due to location (close to facial nerve). • Many of my patients who require repeat surgery are initially operated on by surgeons less familiar with the treatment so the initial surgery is incomplete. I have had patients with culture confirmed NTM fail antibiotic therapy and some with extensive disease respond completely to antibiotic therapy. • We do surgical excision but if the lymph node cannot be completely excised (often because of proximity to critical structures) Page 2 of 4 8/15/07 • My biggest problem is getting them referred to me BEFORE they have received multiple rounds of inappropriate antibiotics and inappropriate surgical procedures without the proper cultures. • It is impossible to know whether antibiotics are "required" and extremely difficult to tell whether they help. The nature history of the infection is spontaneous rupture and prolonged drainage. Most of my cases end up with prolonged drainage from the spontaneous rupture or following surgical excision. None of my cases have been life threatening in any way but all are life annoying and very cosmetically unappealing. •The surgeons see the patient usually before ID and refer pt after excision when histopathology shows caseating granuloma or culture is positive for MAC. At that point I've started azithromycin and continued until the scar is well healed and I don't feel any underlying lymph node. On occasion with a difficult to excise node we've treated with azithromycin until the node is smaller and then excised any remaining node. • Some patients with positive PPD (age, size dependent) need both M.tb and NTM therapy until results available. • 14 were <5y, 1 was 12y. 10 were girls. 13 were cervical, 1 was axillary, 1 was inguinal. 15 were MAC, 13 were both, 2 were antibiotics, 1PPD+ in 6. (This member reported 15 cases). • If extensive, it is often a difficult infection to treat. Pt on multiple abx for 1 year. • Depending on how close to facial nerve or parotid gland - surgical cases may be performed by general pediatric surgeon OR ENT. Incidence is decreasing - we used to see more cases. • How many use ABX monotherapy vs. two/three combination therapy? How many do not treat with either surgery or ABX? • Is PCR approved for this? How long do you treat? When you have a submandibular lesion do the surgeons wait a while prior to excision to avoid facial palsy? • Most of the surgeons here in Las Vegas resist surgery and despite available data prefer you "cure" the infection with antibiotics Geography • My experience in the NE compared with the SW suggests it is more common in the SW • Pretty common here in NC but I'm not in clinic that often so I haven't had any new cases recently. • We did have 1-2 others cases over the preceding 2-3 years. We don’t see it all that often here in Manitoba (that we know of). Pathogenesis, Diagnosis • Several M. bovis cases which I count with TB • Often confirmed by tissue pathology & stains without positive cultures. QuantiFERON useful when PDD+ in older children. • 16 year old female had a lesion over right gluteal area near posterior iliac crest 4cmx2cmx1cm. She developed after using tanning bed. She underwent I&D. She cleared after 8 weeks of clarithromycin and ciprofloxacin. • Some of the cases are culture negative • We have seen an (apparently) increased number of cases involving the face. • Definitely appears to be increasing prevalence. Although I have been directly involved with only one patient in the past 6 months • We do not have PCR testing available here • Most of the lymphadenitis [cases] we see have no identifiable organisms Page 3 of 4 8/15/07 • The first case [M. abscessus/chelonae] occurred from seeding the peritoneum and omental/mesenteric LN's from drainage from a VP shunt where the source was a CNS infection with temp lobe abscess. • We see lots of M. bovis cervical LAN in San Diego (see WM Dankner's paper from a few years back describing the epi nicely) • It seems to be decreasing in our region despite increasing attempts to look for it. • I am seeing more pulmonary disease than lymphadenitis over the last few years. • Need better diagnostic tools • More availability of PCR would be helpful; otherwise, need to wait for culture. Other • Your question about "PPD" is unanswerable--positive or negative at what cut-off of interpretation? • I'd have to pull charts to answer your specific questions about cases; I see about 1 case every 4-6 weeks. Usually it is a toddler (my impression is that male about same as female) and an anterior cervical node. • Commonly seen in young healthy children (<5 yo) as cervical LAN. General comments: • We are seeing infinitely more CA-MRSA • We all need to get a better handle on replacement pneumococcal serotype invasive disease Page 4 of 4