Odontogenic cysts and tumors
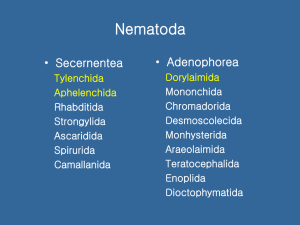
advertisement
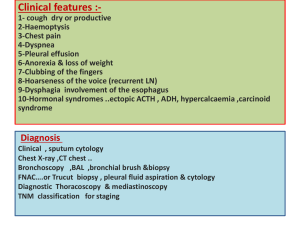
Odontogenic cysts and tumors น่ ารู้ • Gorlin’s syndrome and OKC : basal cell nevus syndrome • Solid ameloblastoma without cortical bone perforation : excision with bony margin 1 cm • Radiographic feature of benign odontogenic cyst and tumor • Multiple osteoma maybe Gardner syndrome : familial adenomatous polyposis (FAP) with the extracolonic manifestations of intestinal polyposis, desmoids, osteomas, and epidermoid cysts (ie, Gardner syndrome). Odontogeneis Primitive oral cavity : stomodeum develop from breakthrough of buccopharyngeal membrane , lined with ectoderm : ectomesenchyme = tissue of tooth develop Tooth bud 3 parts 1. Enamel organ : tooth enamel 2. Dental papilla : tooth pulp + dentin 3. Dental sac : cementum + periodontal ligament Odontogenesis Tooth development : 4 stages 1. Dental lamina stage 2. Bud stage 3. Cap stage 4. Bell stage * Bud,Cap,Bell,Crown •Interruptions in this sequence may lead to the formation of odontogenic tumors. Dental lamina stage • About 6 weeks old – Ridge of basal cell along oral ectoderm proliferation – Form band of epithelium : dental lamina ( future = dental arch ) Bud stage • Epithelial downgrowth and proliferation invagination into ectomesenchyme • Represent the beginning of tooth development appearance of a tooth bud without a clear arrangement of cells A: Epithelial downgrowth along the dental lamina in the upper and lower jaws. B: A magnified view of the bud stage of development. Cap stage • The first signs of an arrangement of cells in the tooth bud occur The peripheral cells are cuboidal the outer enamel epithelium (OEE) The cells in the concavity are tall columnar cells inner dental epithelium. Bell stage • The histodifferentiation and morphodifferentiation takes place A = enamel B = dental papilla C = dental follicle Crown stage • Maturation stage • Hard tissue formation – Enamel – Dentin – Cementum • Forming – Odontoblast – ameloblast Definition : Odontogenic • Derived from tooth forming structure Formation of odontogenic cyst and tumor Derived from : (1) the reduced enamel epithelium of the tooth crown (2) epithelial rests of Malassez, which are remnants of the Hertwig root sheath (3) epithelial rests of Serres, which are remnants of the dental lamina (4) the tooth germ itself, which includes the enamel organ, dental papilla, and dental sac Diagnosis • Complete history – pain, loose teeth, recent occlusal problems, delayed tooth eruption, swellings, dysthesias or intraoral bleeding – onset and course of the growth rate of a mass – parasthesias, trismus, and significant malocclusion Don’t forget : many of these lesions are associated with impacted or congenitally missing teeth • physical examination – careful inspection, palpation, percussion and auscultation of the affected part of the jaw and overlying dentition buccal expansion resulting from growth of an odontogenic tumor in the body of the mandible (arrows). • A panorex radiograph will often confirm clinical suspicions – well-demarcated lesions outlined by sclerotic borders suggest benign growth – ill-defined lytic lesions with possible root resorption : malignancy DDX • By radiographic presentation ( จาก clinical มักไม่แตกต่างกัน ) 1. Radiolucent lesions 2. Radiopaque lesions 3. Mixed radiopaque/radiolucent I. Radiolucent lesion of the jaws A. B. Lesions in the midline of the maxilla 1. Median palatine cyst 2. Nasopalatine duct cyst (incisive canal) Lesions at the apex of the tooth 1. Dental granuloma 2. Periapical cyst (inflammatory) C. Lesion around the crown of an 3. Residual cyst impacted tooth 4. Periapical (dental) abscess 5. Cementoma (first stage) 1. Follicular cyst 6. Odontogenic keratocyst 2. Ameloblastoma 3. Ameloblastic fibroma 4. Odontogenic adenomatoid tumor 5. Odontogenic myxoma 6. Odontogenic keratocyst E . D. Soap-bubble-like radiolucencies 1. Multilocular cyst 2. Aneurysmal bone cyst 3. Ameloblastoma 4. Odontogenic myxoma 5. Central giant-cell granuloma 6. Odontogenic keratocyst E. Lesions that destroy the cortical plate 1. Metastatic tumor 2. Primary malignant tumor 3. Osteomyelitis F. Miscellaneous radiolucent lesions 1. Lateral periodontal cyst 2. Idiopathic bone marrow cavity 3. Hematopoietic marrow 4. Gingival cyst 5. Hemangioma (central) 6. Osteoporosis 7. Stafne's bone cavity II. Radiopaque lesions of the jaws 1. Cementoma (third stage) 2. Compound or complex odontoma 3. Ossifying fibroma 4. Osteoma 5. Torus 6. Root fragment or foreign body 7. Focal sclerosing osteomyelitis 8. Osteogenic sarcoma 9. Chondrosarcoma 10. Metastatic tumor 11. Paget's disease III. Mixed radiolucent/radiopaque lesions of the jaws 1. Cementoma (second stage) 2. Cystic odontoma 3. Ossifying fibroma 4. Adenomatoid odontogenic tumor 5. Calcifying epithelial odontogenic tumor (Pindborg) 6. Calcifying odontogenic cyst (Gorlin) 7. Ameloblastic fibroodontoma 8. Ameloblastic odontoma 9. Osteogenic sarcoma 10. Chondrosarcoma Aspiration Biopsy • straw-colored fluid : most likely to be a cystic lesion • pus : an inflammatory or infectious process • White keratin-containing fluid : odontogenic keratocyst • Air may indicate a traumatic bone cavity • Blood represent several lesions : the most important is vascular malformation inability to aspirate (vacuum within the syringe) is usually indicative of a solid process such as a neoplasm. Indications for excisional biopsy • small • radiographically benign lesions • accessible and can be removed without encroachment on adjacent structures. Odontogenic cysts • Inflammatory Radicular (periapical) Cyst Paradental Cyst • Developmental – Dentigerous (follicular) Cyst – Developmental Lateral Periodontal Cyst – – Odontogenic Keratocyst (OKC Glandular Odontogenic Cyst (GOC • True cyst : epithelium lining a collagenous cyst wall • Histologically a fibrous connective tissue stroma with multiple cavernous and sinusoidal spaces with multinucleated giant cells within the stroma Enucleation is the treatment of choice CLASSIFICATION OF JAW CYSTS A. Developmental 1. Odontongenic a. Follicular cyst b. Odontogenic keratocyst c. Eruption cyst d. Alveolar cyst of infants e. Gingival cyst of adults f. Developmental lateral periodontal cyst 2. Nonodontogenic a. Nasopalatine duct cust b. Midpalatal cyst of infants c. Nasolabial cyst d. Globulomaxillary cyst, median mandibular cyst, and median alveolar cyst * B. Inflammatory a. Radicular cyst 1. Periapical cyst 2. Inflammatory lateral periodontal cyst C. Nonepithelial a. Idiopathic bone cavity (traumatic, solitary, hemorrhagic bone cyst) b. Aneurysmal bone cyst c. Stafne's mandibular lingual cortical defect CLASSIFICATION OF ODONTOGENIC TUMORS A. Benign epithelial odontogenic tumors 1. Tumors producing minimal inductive change in the connective tissue a. Ameloblastoma b. Calcifying epithelial odontogenic tumor (Pindborg tumor) c. Odontogenic adenomatoid tumor (adenoameloblastoma, adenomatoidodontogenic tumor) d. Calcifying odontogenic cyst (Gorlin's cyst) 2. Tumors producing extensive inductive change in the connective tissue a. Ameloblastic fibroma b. Ameloblastic fibroodontoma c. Ameloblastic odontoma (odontoameloblastoma) d. Odontoma 1. Compound-composite odontoma 2. Complex odontoma B. Mesenchymal odontogenic tumors 1. Odontogenic fibroma 2. Odontogenic myxoma 3. Cementoma a. Periapical cemental dysplasia b. Cementifying fibroma c. Benign cementoblastoma 4. Dentinoma C. Tumors of unknown origin 1. Melanotic neuroectodermal tumor of infancy D. Malignant odontogenic tumors 1. 2. 3. 4. Primary intraosseous carcinoma Ameloblastic fibrosarcoma Ameloblastic dentinosarcoma Ameloblastic odontosarcoma Dentigerous (follicular) Cyst Definition: assosiated with crown of unerupted tooth • accumulation of fluid between reduced enamel epithelium and a completed tooth crown • most common developmental cyst (24%) Dentigerous (follicular) Cyst • Teenage, early childhood • mandibular 3rd molars, maxillary canines, and maxillary third molars • asymptomatic , impacted tooth , bony expansion Treatment : • enucleation • decompression followed by enucleation if large. Radiographic Features • Unilocular radiolucency • well defined sclerotic margins encircling the crown of an unerrupted tooth • Mandibular cyst can displace into ramus/inferior border of mandible • Maxillary cyst can displace tooth into maxillary sinus Radiographic Features • Histologically: a cyst composed of thin connective tissue walls lined by stratified nonkeratinizing squamous epithelium over a fibrocollagenous cyst wall Neoplastic potential • Turn to true neoplasm – SCCA – Mucoepidermoid CA • 17% of Ameloblastoma from dentigerous cyst Odontogenic keratocyst (OKC) Parakeratinizing Odontogenic Keratocyst Keratocystic Odontogenic Tumor (WHO) • WHO classify as tumor – Soft tissue extension, extension to adjacent bone, bony destruction • Thought to develop from remnants of dental lamina(rests of Seres) , may no tooth associated Odontogenic keratocyst (OKC) Clinical : • any age, peak incidence 2nd- 3rd decades • 75% at mandible – mostly 3rd molar and ramus • Symptomatic Swelling, pain, trismus, sensory deficit, infection (most common) Odontogenic keratocyst (OKC) • Diagnosis : histologic • High recurrence rate : – Only enucleation : 62.5% – Enucleation + careful curettage: < 10% Why high recurrence ? 1. 2. 3. 4. 5. **Daughter/ Satellate cyst formation** Collagenase activity of the cyst Remnant of dental lamina rest at the cyst wall PG- induced bone resorption Increase mitotic activity ** OKC need aggressive treatment ** Radiographic Features unilocular/ multilocular radiolucency well circumscribed with sclerotic border teeth may displaced may seen cortical perforation Radiographic Features • CT scan – Assess large lesion – Assess maxillary lesion • Gorlin syndrome metachronous, synchronous cyst Histologic : specific criteria 1. Thin,stratified squamous epithelium 2. Prominent columnar or cuboidal basal cell layer with dense nuclear staining with palisading “tombstone appearance” 3. 4. Corrugated surface Parakeratinizing stratified squamous epithelium Not pathognomonic Luminal material : straw-colored clear to creamy white keratin –filled material Treatment • Careful enucleation + partial bone removal • Curretage • Peripheral ostectomy with rotary blur • Excision – Bone penetration remove periosteum • Remove cyst lining, satellite cyst, dental lamina rest Treatment – Recurrent: within 5 years – Close radiographic F/U • Early detection • Decrease complication of recurrent • > 1 cyst Family history (Gorlin syndrome) • Carnoy’s solution – Controversial – Chemical cauterization Basal cell nevus syndrome (Gorlin syndrome) •Autosomal dominant •Large variation in expression •Mutation of PTCH tumor supp gene •Multiple OKC of jaw multiple basal cell CA Frontal bossing, mandibular prognathism Palmar,plantar pitting, bifid ribs Calcification of falx cerebri Basal cell nevus syndrome (Gorlin syndrome) • Recurrence new occurrence • Large lesion decompression • Teeth should be saved – Canine, incisor, 1st molar Radicular cyst • Periapical cyst, periradicular cyst Clinical Asymptomatic • the most common odontogenic cyst (65%) • Arise from the epithelial cell rests of Malassez in response to inflammation Associated with Nonvital tooth Radiographic findings Microscopically cyst with a connective a pulpless, nonvital tooth that has a small welldefined periapical radiolucency at its apex tissue wall that may vary in thickness, a stratified squamous epithelium lining, and foci of chronic inflammatory cells within the lumen Treatment is extraction of the affected tooth and its periapical soft tissue or root canal if the tooth can be preserved. (1,2)Periapical cyst in 60-year-old woman. CT scan demonstrate radiolucent lesion (arrows) surrounding the apex of molar. defect with denfilling (arrowhead) is present within the crown of the tooth. (3) Periapical cyst in 40-year-old man. Panorex imdemonstrates circular radiolucent lesion (arrow) at the apex of molar. Note the dental filling (arrowhead) Odontogenic tumor Ameloblastoma • Unicystic • Interosseous • Peripheral Ameloblastoma Interosseous type • Solid, not peripheral • Arised from lining odontogenic cyst, reduced enamel epithelium, odotogenic rest Ameloblastoma Interosseous type • 80% mandible • Maxilla may involve sinonasal region • Location of tumor are important for long term prognosis – Anterior maxilla/ body of mandible – Posterior ramus of mandible Ameloblastoma Interosseous type Radiographic findings • Small unilocular radiolucency, well dermacrate • Large “Soap bubble”, honeycomb appearance – May resorp root in long-standing lesion • Desmoplastic type – Mixed radiolucent radiopaque lesion – Maxilla and anterior portion of jaws Histopathology : 6 patterns 1. Follicular 2. Plexiform The two most frequent patterns are the follicular and plexiform 3. Basal cell 4. Acanthomatous 5. Granular cell 6. Desmoplastic Histologic subtypes are not of therapeutic and prognosis important Vickers & Gorlin criteria • • • • Columinar basilar cells Palisading of basillar cells Polarization of basillar cells Hyperchromatism of basal cell nuclei in the epithelial lining • Subnuclear vacuolization of cytoplsam in basillar cells (c) High-power photomicrograph hematoxylin-eosin [H-E] stain) reveals numerous well-defined islands of odontogenic epithelium with palisading and polarizing nuclei (arrows) Natural history • Ability to infiltrate medullary bone and relative inability to infiltrate compact bone – Dense compact bone • Inferior border of mandible, ramus – Outer periosteum is barrier • The location of tumor – Posterior maxilla, involve orbit Treatment • High recurrance – Tumor infiltrate trabeculae of cancellous bone Mandibular ameloblastoma • 1cm of medullary margin – Proximal &distal – Lingual & buccal cortical bone sacrificed • Not include soft tissue outside periosteum Ameloblastoma Interosseous type Maxillary Ameloblastoma • Margin is more important – Fossen section for soft tissue margin – Margin 1-2 cm • Spare vision, vital structure • F/U extremely important Ameloblastoma Unicystic type • Unicystic – Intraluminal – Mural – Intramural Ameloblastoma Unicystic type Definition • Unilocular • Unicystic • Patho lining of ameloblastoma – Vickers & Gorlin criteria • * not invade connective tissue * Therapeutic planning & clinical behaviors Ameloblastoma Unicystic type • 15% of Ameloblastoma • Posterior mandible • Asymtomatic • Radiographic feature – Radiolucent, unilocular – Well dermacrate Treatment • Enucleation – Histo Vickers & Gorlin criteria for Dx Ameloblastoma • Histo: characteristic of luminal or intaluminal involvement – Radiograph singular unilocular radiolucency • No septate – Intra-op confirm of unilocular – No multilocular, multicystic, cortical perforation, soft tissue involvement – Size < 2 cm Peripheral Ameloblastoma • Mucosal mass from gingiva/ alveolar mucosa • From dental lamina rests/ basal cells of mucosa • ** Not infiltrate underlying bone** • Bone involvement intaosseous ameloblastoma Peripheral Ameloblastoma Diagnosis • CT / MRI • Excision, patho comfirm margin Malignant ameloblastoma • Classic benign histopatho feature • Metastasis to distant location – Lung ( most common) – Cervical LN • Treatment Depend on degree and site of involvement – Excision – RT (option) Radiographics a unilocular or multilocular radiolucency with ill-defined borders, (making it difficult to determine the exact size of the lesion) Buccal and lingual cortical expansion is common, even progressing to cortical perforation Root resorption occurs infrequently. Histopathology • The ameloblastoma is unencapsulated, so it typically exhibits “ an infiltrative growth pattern into surrounding tissues ” The basal cells in the epithelium are columnar and hyperchromatic and demonstrate reverse polarity, ( in which the nuclei move from the basement membrane pole of the cell to the opposite pole) • The two most frequent patterns are the follicular and plexiform Odontoma most common odontogenic tumor of the mandible approximately 67% of all cases consists of various tooth components, including dentin and enamel 50% associated with an impacted tooth Forming between the roots of teeth, the tumor is initially radiolucent but evolves to contain small calcifications.orms radioopaque mass with alucent rim Malignant Odontogenic Tumors • Primary Intraosseous Carcinoma • extremely rare tumor • may be of three different types : 1. Arising from an odontogenic cyst 2. Developing from an ameloblastoma Well differentiated (malignant ameloblastoma) Poorly differentiated (ameloblastic carcinoma) 3. Arising from odontogenic epithelium SURGICAL MANAGEMENT OF ODONTOGENIC CYSTS AND TUMORS goals of management of benign odontogenic cysts and tumors : (1) remove all abnormal tissue (2) conserve healthy bone and dental structures (3) preserve adjacent structures such as the inferior alveolar nerve (4) restore the surgical defect to its presurgical state of anatomic form and function (5) prevent recurrence of the lesion. • Enucleation of a lesion : involves local removal of the lesion by instrumentation in direct contact with the lesion • Resection : involves incision or osteotomy through uninvolved tissue adjacent to the lesion without disruption of the lesion • Composite resection : involves removal of tumor, adjacent bone, soft tissue, and contiguous lymph node channels • Enucleation and curettage – Odontogenic cysts: Virtually all unless recurrent – Odontogenic tumors: Odontoma Ameloblastic fibroma Ameloblastic fibroodontoma Adenomatoid odontogenic tumor Calcifying odontogenic cyst Cementoblastoma Central cementifying fibroma Unicystic ameloblastoma (except mural type) • Marginal or partial resection – Odontogenic cysts: Recurrent odontogenic keratocyst – Odontogenic tumors: Ameloblastoma (solid and mural type unicystic) Calcifying epithelial odontogenic tumor (Pindborg tumor) Odontogenic myxoma Ameloblastic odontoma Squamous odontogenic tumor • Composite resection * – Odontogenic tumors: Malignant ameloblastoma Ameloblastic fibrosarcoma Ameloblastic odontosarcoma Primary intraosseous carcinoma These lesions are malignancies and may be treated variably and with additional modalities such as radiation or chemotherapy. management of odontogenic lesion of mandible