File
advertisement

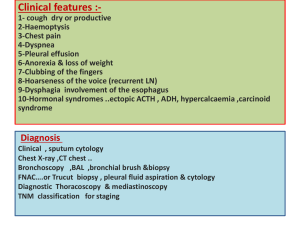
Neck masses in children Block 12 – Head and Neck 2012 Dr EW Müller Aetiology • Infections with acute or chronic lymphadenitis • Tumors • Congenital – – – – – Thyroglossal cyst Epidermoid cyst Branchial cyst or fistula Lymphangioma Haemangioma and arterio-venous malformations Infection: Acute lymphadenitis • Most common cause: Bacterial infection of the oropharynx, face or scalp: Tonsillitis, Pharyngitis, impetigo of the scalp • Organisms: Staph aureus, Streptococcus • Clinic: Multiple tender lymph nodes in the submandibular or anterior cervical region. The lymph nodes are smooth, soft, not matted, mobile. Fever, systemic illness. • Initial treatment with antibiotics (Cloxacillin, Ampicillin) often results in resolution without suppuration. • Without (and with) treatment, the lymph node may become enlarged and fluctuant, leading to abscess formation. • An abscess needs surgical drainage. Drainage pathways • Face, anterior scalp, forehead drain into facial, preauricular, submental LNs • Tonsills, posterior pharynx drain into jugulodigastric, deep cervical LNs • Posterior scalp, back of ear, external ear drain into posterior superficial cervical, posterior auricular, occipital LNs Infection: Chronic lymphadenitis • Clinic: Chronically enlarged, non-tender lymph nodes. • Differential diagnosis: Tb, atypical mycobacterial infection, cat scratch disease; malignancy • A single, dominant lymph node (>2cm big) present longer than 6 – 8 wks, which has not responded to antibiotic therapy, should be excised, cultured, and submitted for histological examination. • HIV – often associated with Tb, lymphoma. Look for abnormally large lymphnodes Neoplasms • Lymphoma: By far the most common childhood neoplasm presenting with enlarged lymph nodes in the neck. • Lymph nodes are usually rubbery, non tender and fixed. They may enlarge quickly. • Diagnosis: By biopsy of enlarged lymph node. Congenital neck masses • • • • Branchial Cysts and Sinuses Thyroglossal duct cyst Dermoid and epidermoid cyst Lymphangioma Branchial Cysts and Sinuses • These are remnants of the branchial apparatus which develops between the 4th and 8th week of pregnancy. • The apparatus consists of 4 branchial arches separated by branchial clefts. If the clefts fail to regress, a sinus or cyst will form. Embryonic branchial apparatus Mandibula and Maxillary process of the upper jaw Hyoid Inferior parathyroid and thymus Superior parathyroid and parafollicular cells Branchial remnants • Present as fistulas or cysts anywhere on the anterior border of the sternocleidomastoideus muscle • Cyst presents with nontender enlarging swelling • Fistula presents with drainage of saliva from the ostium • Treatment: Early excision • Complication: Cysts and fistulas can become infected if not resected early in childhood Thyroglossal cyst - Embryology The foramen caecum is the site of the development of the thyroid at the base of the prospective tongue. As the tongue develops, the thryroid diverticulum descends in the neck, maintaining its connection to the foramen caecum. A cyst can be located anywhere along the migratory tract if it fails to become obliterated. Thyroglossal cyst - Clinic • Thyroglossal cysts are located in the midline at or just below the hyoid bone. • Due to communication with the mouth via the foramen caecum the cyst can become infected. • The cyst is smooth, soft and non-tender. • Owing to its attachment to the foramen caecum, the cyst does move upwards when the tongue protrudes. Thyroglossal cyst Thyroglossal cyst - Treatment • Early surgical excision to avoid the complications of infection • Surgery entails complete excision of the cyst and its tract upward to the base of the tongue (Sistrunk Operation) Epidermoid cysts • Represent ectodermal elements, which where trapped beneath the skin • Epidermoid cysts contain sebaceous material within the cyst cavity. • Most common location is at the lateral corner of the eyebrow. Presents with a characteristic swelling. • Midline epidermoid cysts develop due to entrapment of epithelium of branchial arch origin at the time of embryologic midline fusion. They might be confused with midline thyroglossal duct cysts. Lymphangioma • Lymphangiomas are congenital malformations of lymph tissue that result from the failure of lymph spaces to connect to the rest of the lymphatic system. • Lymphangiomas present as a soft, smooth, nontender mass that is compressible and can be transilluminated. • Depending on the size and location, there might be respiratory compromise and difficulty in feeding. Lymphangioma: Treatment • Goals: Improvement of cosmetic appearance, relieve of impaired breathing and eating. • Big lesions causing respiratory embarrassment might need urgent intubation at birth. • Surgery is difficult because of the infiltrative nature of these lesions. • Preferred treatment is infiltration with Bleomycin, alcohol or other scerosing agents. Haemangiomas • Haemangiomas are benign tumors of the capillary vessels of the skin • They can occur anywhere, but are common in the face and neck • Typical growth, stationary and involutionary phase • Treatment : conservative (wait and see); excision or sclerosation