193_fullpaper - Stanley Radiology
advertisement
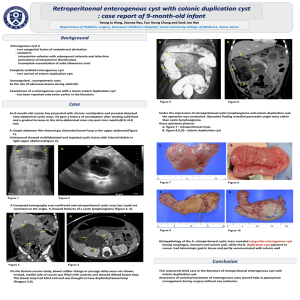
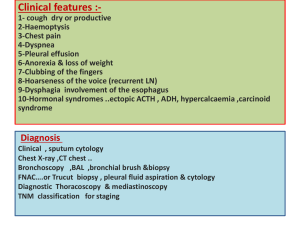
To analyze symptomatic and asymptomatic patients for assessing adnexal lesions Comparison is done with ultrasound and magnetic resonance imaging and final diagnosis is made with histopathology / FNAC findings. A retrospective study was done involving 6 women of various age groups who presented with adnexal lesions. Ultrasound scans were evaluated according to sonographic scoring systems. Transverse and sagital T1 weighted magnetic resonance images were obtained before and after administration of contrast with a fat saturation technique and T2 weighted images were acquired. Adnexal lesions were first assessed with each modality and final diagnosis was made with histopathology / FNAC reports. The ovaries are suspended on either side of the uterus in the petitoneal cavity. The broad ligaments, consisting of two layered folds of peritoneum, run betweent he uterus and the lateral pelvic walls. Other ligamentous connections between the ovaries. Uterine tubes, and the surrounding structures are the mesosalpinx, the mesovarium, the ovarian ligament, and the suspensory ligament of the ovary. This diagram shows the progression of the ovarian follicle from a primordial follicle, to a priamary follicle , to a secondary follicle. The matures follicle eventually ruptures to release the oocyte, and the follicle remnants become the corpus luteum, which releases progesterone. If no fertilization event occurs, the corpus luteum involutes into whits fiberous tissue(corpus albicans), and the next cycle of ovulation continues. Next we will view the appreance of the normal ovary on ultrasound. A normal follicle in premenopausal women appears as a <20-25mm simple, anechoic, fluid filled cyst. A normal corpus luteum appears as a cystic mass with a thick crenulated wall and peripheral blood floe, or “ring of fire” Here is the characteristic appearance of a postmenopausal ovary, which is small and homogenous in echotexture. PATIENTS NAME AGE USG MRI HPE/FNAC PATIENT 1 21 Bilateral dermoid Features suggestive of immature/ malignant ovarian teratoma Left : Immature teratoma grade II Right : Benign cystic teratoma PATIENT 2 30 Right hemorrhagic cyst / adenomyoma Right hemorrhagic cyst / adenomyoma Ovaries showed corpus albicantes and corpus follicular cyst PATIENTS NAME AGE USG MRI HPE/FNAC PATIENT 3 55 Left ovarian simple cyst Left ovarian simple cyst Benign serous cystadenoma PATIENT 4 39 Bilateral complex / endometriotic cyst Bilateral endo metriotic cyst Features suggestive of bilateral endomeriotic cyst PATIENTS NAME AGE USG MRI HPE/FNAC PATIENT 5 14 Left mesenteric / complex cyst Left paraovarian cyst / mesenteric cyst / left ovarian cyst Features suggestive of simple cyst of ovary PATIENT 6 39 Right complex cyst Right complex cyst Featyres suggestive of corpus luteal cyst A 21 year old nulliparous women, was diagnosed with ovarian mass incidentally on ultrasound a month ago She complained of weight loss (6 kgs in 3 weeks), fatigue and loss of appetite. Her menstrual cycles were uneventful. She is not a known case of diabetes mellitus / hypertension / epilepsy / tuberculosis / thyroid disorders She is a known case of bronchial asthma for the past 4 years on irregular treatment. No history of previous surgeries No history of malignancy in family Her Ca125 (Tumour marker) was 115.9 U/ml USG FINDINGS A hyperechogenic solid cystic lesion measuring 3.4 x 3.6 cm seen in the right adnexa. A large heterogeneous hyperechogenic lesion with multiple cystic components measuring 14.3 x 9 cm seen in the pelvis and periumbilical region, in the midline. Multiple calcified foci noted within the lesion. Both ovaries were not separately visualized. Possibility of BILATERAL DERMOID was considered Both ovaries in relation to the uterus Right ovary showing both solid and cystic components Abundant vascularity on color doppler MRI FINDINGS A well defined right adnexal mass lesion showing mixed sinal (fat/ soft tissue) with internal solid nodules. Peripheral curvilinear T2 hypointense signal calcification. seen suggesting Large mixed signal cystic solid midline abdominopelvic mass with internal fat signal and multiple T2 hypointense calcification.. Uterus was displaced to the left side by the lesion. Features suggestive of bilateral immature / malignant teratoma. Arrow marks show bilateral immature / malignant teratoma. OPERATIVE FINDINGS Cystic mass of size 20 x 15 cm found occupying the mid line upto the epicgastric region. A few cysts were removed and this mass was seen arising from the left ovary. And the mass was found to be both solid and cystic. Left ovary was not separately visulaised. Right ovary enlarged to 5 x 5 cm and found to be solid. HPE FINDINGS LEFT OVARY : Left ovarian solid and cystic mass shows a neoplasm composed of islands of cartilage and bone, cystic spaces lined by stratified squamous respiratory epithelium, fibrous tissue, fatty tissue and glandular elements adhered to immature neuro ectodermal tissue and myxoid areas. Impression : Immature teratoma grade II RIGHT OVARY : Right ovary shows ovarian stroma enclosing a cystic lesion lined by stratified squamous epithelium and pilo sebaceous glands. No evidence of immature elements. Impression : Benign cystic teratoma. Islands of cartilage with respiratory epithelium Mature and immature glial tissue Sections shows skin with pilosebaceous glands Section shows bone tissue The sensitivity to MRI for identifying malignancy was 100 % Excellent agreement was seen between MRI and the final HPE/FNAC diagnosis for determining the origin, tissue content and tissue characteristics of a mass. Sonography had poor agreement with the final diagnosis for the origin and tissue content of a mass. The prime reason for indeterminate sonographic diagnosis was the inability to exactly determine the origin of the lesion because of location and mass size and the appearance of purely solid or complex cystic masses. The above study reveals that ultrasound can be used as a screening technique, while magnetic resonance imaging remains the modality of choice for diagnosis and assessment of symptomatic and asymptomatic adnexal lesions. THANK YOU