Jeronimo090910 (FILEminimizer)
advertisement
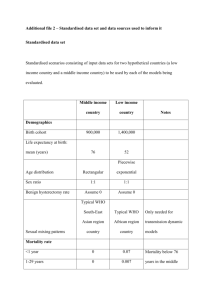
Welcome to I-TECH HIV/AIDS Clinical Seminar Series 9 September 2010 Cervical cancer screening in resourcelimited settings Jose Jeronimo, MD Cervical cancer screening in resource-limited settings Jose Jeronimo, MD I-Tech distance learning sessions September 9, 2010 1 Cervical Cancer Incidence Europe 59,931 North America 14,670 Central and South America 71,862 Africa 78,897 Asia 265,884 1. Ferlay J, Bray F, Pisani P, Parkins DM; International Agency for Research on Cancer (IARC). GLOBOCAN 2002: Cancer Incidence, Mortality, and Prevalence Worldwide. Lyon, France: IARCPress; 2004. CancerBase No. 5, version 2.0. Human Papillomavirus (HPV) Epsilon FPV PePV TmPV1 Condyloma 25 19 20 14D 21 5 36 47 RTRX7 12 8 93 24 96 92 76 75 49 23 22 38 37 17 A8 7 2 5 67 33 58 31 R 16 A9 35 73 34 PV Rh 97 45 18R 68 39 70 85 59 69 26 82a 51 53 30 66 56 78 10 94 28 A11 Neoplastic A7 Alpha A5 A6 A2 A15 84 86 87 BPV4 BPV935 BPV6 PsPV 50 48 60 65 3 29 7771a 90 6 0 1 57 27 2a 62 81 61 72 89 83 102 8 15 0 Vaginal Ha 1 0 9 O1P 3 0V 1 Beta Eq O PV v Ov PV 1 PV 2 1 R EE PV PV DP B V BP PV V BPV 2 5 A13 A1 6 1 741a 44 55 1C3h PC PV PV 54 a 32 42 43 9 40 1 Delta PV RO V P CR 63 PV1 Fd PV CO 11 PV4 Ed PPVV n Muin Eq Theta Eta Mu Kappa Lambda A10 Nu Lota Zeta New A3 Pi Genus GammaXi Omikron A4 ≥100 HPV genotypes ~40 mucotropic HPV genotypes ~15 Carcinogenic HPV genotypes Natural History of HPV infection and Cervical Cancer Peak Ages: 15-25 25-35 45-50 Schiffman, et al., Lancet, 2007 Primary prevention Secondary Prevention Current screening options Visual inspection PAP smear with acetic acid HPV testing (VIA) CervicalIncidencia Cancer Incidence, England de cáncer cervical invasor 1971-95 estandarizada por edad, Inglaterra 1975-95 100 18 90 80 70 14 60 Invasive cervical cancer 50 40 10 30 National call-recall introduced 20 10 0 Quinn et al, BMJ 1999 95 19 91 19 87 19 83 19 79 19 19 19 71 75 06 Percentage Incidence rate / 100,000 Coverage Sensitivity of Cytology: CIN2+ CIN 2+ HART Tuebingen Hannover Jena French Public French Private Seattle Canada Combined 0% Cuzick et al., IJC, 2006 Mayrand et al., NEJM, 2007 10% 30% 50% 70% 90% 100% VIA “VIA is a good alternative for settings where conventional cytology is not well implemented.” –IARC/WHO, 2005 IARC, WHO. IARC Handbooks of Cancer Prevention: Cervical Cancer Screening. Volume 10. IARC Press; 2005. VIA Negative Positive Unmagnified view Alternatives for screening: HPV DNA testing The digene®HC2 HPV DNA Test The careHPV™ Test HPV DNA testing CIN 2+ HART Tuebingen Hannover Jena French Public French Private Seattle Canada Combined 0% 10% 30% 50% 70% HPV sensitivity Cuzick et al., IJC, 2006 Mayrand et al., NEJM, 2007 90% 100% Follow-up time and HPV result 25% HPV16 + HPV18 + Acumulate Incidence ≥CIN3 20% 15% 10% 5% HPV + 0% 0.0 4.5 15.0 27.0 39.0 51.0 63.0 75.0 Follow-up (months) Khan et al., JNCI, 2005; Castle et al., AJOG, 2007 87.0 99.0 111.0 119.5 HPV- The careHPV™ Test: a new HPV DNA test for low-resource settings The careHPV™ Test: an alternative for developing countries START-UP* demonstration projects *Screening Technologies to Advance Rapid Testing for Cervical Cancer Prevention—Utility and Program Planning. Preliminary results Screening method Vaginal careHPV Cervical careHPV VIA Pap (ASCUS+) Sensitivity* Specificity* (95% CI) (95% CI) 87.8% 83.9% (73.8, 95.9) (82.3, 85.4) 85.4% 88.8% (70.8, 94.4) (87.4, 90.1) 73.2% 78.5% (57.1, 85.8) (76.8, 80.2) 48.9% 98.2% (32.9, 64.9) (97.6, 98.7) *Clinical sensitivity and specificity estimates. Based on results from 2,239 women with screening and final diagnosis completed in Nicaragua and Hyderabad. 41 cases of CIN2+. Cervical cancer in HIV infected women Higher prevalence of HPV infected women. Performance of screening tests is different than in general population: - Higher positive rates. Need for intervention. Need for evaluation of screening and treatment strategies in countries with high HIV prevalence. Conclusions • There is no screening test that is 100% effective for detecting cervical precancer. • There are more affordable options for secondary prevention in low-resource settings. • Screening for cervical cancer and treatment in HIV-infected women seems to be more challenging than screening and treating HIVnegative women. Thank you jjeronimo@path.org www.path.org www.rho.org Thank you! Listserv: itechdistlearning@u.washington.edu Email: DLinfo@u.washington.edu Welcome to I-TECH HIV/AIDS Clinical Seminar Series Next session: 23 September 2010 Mystery Opportunistic Infections Shireesha Dhanireddy MD