UPDATE
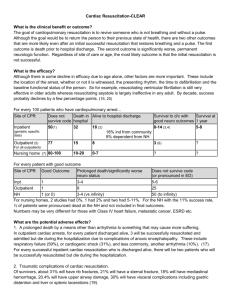
advertisement
UPDATE: IN-HOSPITAL CARDIOPULMONARY RESUSCITATION Cardiac Arrests at JHH • 85 cardiac arrests in 2011: – – – – excluding ED, ICU and theatres 3 in the cath lab (1 survived) 26 in CCU (58% survived, 32% died) 9 in G3 (1 survived to get to ICU) • Of the remaining 47 patients: – 72% died – 11% made it to discharge Australian Resuscitation Council 2010 DRS ABCD (S=send for help) • When to commence CPR – Unresponsiveness and abnormal breathing – Check for central pulse for 10 seconds [A, ECO] • Hand placement – Lower half of the sternum – Inter-nipple line • Depth of compression – 1/3 chest wall depth or greater than 5cm [A, animal] Cardiopulmonary resuscitation for advanced life support providers. ARC and NZRC Guidelines 2010, Emerg Med Aust, 2011,23:264-70 Australian Resuscitation Council 2010 • Compression rate – 100 per minute, no evidence for faster rate [A, animal] • Compression:relaxation ratio – Equal time spent in compression and release – Aim to achieve complete recoil of chest between compressions • Provision of a firm surface – [A, manikin] Australian Resuscitation Council 2010 • Minimise interruptions to CPR [A, human] – – – – Continue without interruption unless evidence of return to breathing or specific task Attempts at intubation should NOT interrupt Planned pauses for rhythm/pulse analysis <10sec • Compression ventilation ratio – – – – – – Before airway is secured, 30:2 [A, EO] After secured, ventilate with 100% O2 need to assess chest rise with EACH breath 6-10 ventilations per minute with airway [A, EO] Don’t interrupt compressions, but time with compressions Don’t ventilate at same time as compression Australian Resuscitation Council 2010 • Fatigue – Chest compressions become shallower at one minute but providers only become aware at 5 minutes – Swap pumpers every two minutes • Perform CPR right up to the point of shock • Recommence CPR immediately after shock – If rhythm compatible with spont circulation, check pulse – Otherwise, keep pumping • Shock – Monophasic =360J, biphasic =200J Australian Resuscitation Council 2010 • Precordial thump – Doesn’t work in VF, might work in VT • Vasopressors – Increase return of spontaneous circulation – No improvement in longer term outcome – Adrenaline 1mg IV at time of commencement • Anti-arrhythmics – No evidence of improved mortality – Give amiodarone after 3rd unsuccessful defib Australian Resuscitation Council 2010 • Monitor adequacy of CPR – – – – Technique End-tidal CO2 - low CO2 = breathing too fast ABG - only for electrolytes, NOT for acid base state Real-time feedback devices • Harm to patient during CPR • Audit, feedback and quality improvement Australian Resuscitation Council 2010 • Guidelines also encompass: – Seek reversible causes – Special circumstances • Anaphylaxis, avalanches, pregnancy, tamponade, etc. – Managing acute dysarrhythmias – Evidence for equipment – Post resuscitation therapy • • • • • • PCI in STEMI Use of amiodarone prophylactic anti-arrhythmic [A, EO] BP, BSL, O2 and CO2 ,neuro, temperature etc Consider resuscitation related injuries Prognosis Organ donation American guidelines Differences • • • • ABC becomes CAB Atropine has been officially removed Cricoid pressure has been removed Consider all for cardiac catheterisation Evidence • Evolution in understanding over the past decade – The longer someone is in VF, the harder to cardiovert – The better perfused the myocardium is prior to a shock, the more likely cardioversion is to work – A single dose of adrenaline is the only drug which can help return of spontaneous circulation, except for MgSO4 in torsades – Over-ventilation is harmful, “lazarus syndrome” Evidence for training to improve technique and outcomes • Teaching hand placement improves technique1 • Teaching ALS results in improved technique for at least 6 months2 1. Owen et al, A randomised control trial comparing two techniques for locating chest compression hand position in adult basic life support, Resuscitation 2011, 82:944-6 2. Ettl et al, Updated teaching techniques improve CPR performance measures: a cluster randomised control trial, Resuscitation 2011, 82:730-5 Technique • Important not to “lean” on patient between compressions as reduces chest expansion1 • Supraglotic airways are adequate in an emergency and reduce “hands off time”2 • Pause for ECG analysis <10 seconds3 1. Editorial, Leaning is common in chest compressions but remains a relatively unknown entity, Resuscitation 2011, 82:971-2 2. Hands-off time during insertion of six airways devices during cardiopulmonary resuscitation: a randomised manikin trial, Resuscitation 2011, 82:1060-3 3. Editorial, Pauses during CPR are breaks hinering our efforts? Resuscitation 2011, 82:1379-80 Longer pauses between compressions and defib decrease survival 815 out of hospital arrests treated by paramedics • Longer pre-shock periods were associated with decreased survival1 • Longer than 20 seconds vs <10sec OR=0.47 • For peri-shock pause: – >40 seconds, 45% decrease in survival compared to – peri-shock pause <20sec Cheskes et al, Circulation 2011, 124:58-66 Evidence for Drugs in Resus • Adrenaline doubles chance of return to spont. circulation but no mortality benefit: – Survival to hospital d/c - 10.5% vs 9.2% – Survival with favourable neuro - 9.8% vs 8.1% • Vasopressin and terlipressin are as good as adrenaline • Short-term benefit of amiodarone • MgSO4 for torsades works Morley, Drugs during cardiopulmonary resuscitation, Cardiopulm Resus, 2011, 17:214-18 Evidence of damage secondary to CPR • 65% of patients have rib fractures • 30% of patients have sternum fractures • Patients >60yrs old much greater risk Kim et al, Multidetector CT findings of skeletal chest injuries secondary to cardiopulmonary resuscitation, Resuscitation 2011, 82:1285-88 Evidence of damage secondary to CPR • 1987 study of 705 autopsies after CPR – 18% had mediastinal hemorrhage – 3% had abdo visceral / oesophageal rupture – 10% had pericardial bleeding or lacerations of the great vessels or myocardium Bardy, A ciritcs assessment of our approach to cardiac arrest, NEJM 2011, 364:374-5 Krischer et al, Complications of cardiac resuscitation, Chest 1987, 92:287-91 Evidence of damage secondary to CPR • Recognition of gastric rupture secondary to use of laryngeal mask in CPR Haslam et al, Gastric rupture associated with use of the laryngeal mask during cardiopulmonary resuscitation, BMJ 2004, 329:1225-6 Evidence of damage secondary to CPR • Extreme oxygen tension associated with increased mortality • Hypothesized to be global ischaemia / reperfusion injury Kilgannon et al, Relationship between supranomral oxygen tension and outcome after resuscitation from cardiac arrest, Circulation 2011, 123:2717-22 Treatment protocols for post arrest improve outcomes • Out-of-hospital arrest, favourable outcome can be achieved (25% vs 56%) by following stardard protocol1 including – PCI for all ST elevation ECG – Mild therapeutic hypothermia (MTH) – Standard ICU protocols 1. Tomte et al, Strong and weak aspects of an established post-resuscitation treatment protocol - a five year observational study, Resuscitation 2011, 82:1186-93 Rhythms and outcomes • American Heart Association National Registry for Cardiopulmonary Resuscitation • 51,919 pts with pulsless cardiac arrest between 1999 and 2005 – – – – VT 7% VF 17% PEA 37% Asystole 39% • Survival to hospital discharge was – 37% in VF/VT and – 12% PEA, – 11% asystole Evidence for CCU and Monitoring • Good evidence that monitoring improves outcomes in cardiac arrest • Cerebral performance caregory 1 or 2 at discharge compared to non-witnessed: • OR 2.4 if monitored and witnessed • OR 2.12. if monitored only • OR 2.42 if witnessed only Brady et al, In-hospital cardiac arrest: impact of monitoring and witnessed event on patient survival and neurologic status at hospital discharge, Resuscitation 2011, 82:845-52 Resuscitation in elderly hospital inpatients? • Individuals with certain characteristics automatically opted out1 • Better education for healthcare workers re decision to resuscitate and the right of medic to withhold2 • If a patient enters hospital and there is a plausible risk of cardiac arrest, physician should recommend against it when there is a low likelihood of benefit3 1. 2. 3. Opt in not out. BMJ 2011, 343:5251 Progress towards fewer inappropriate attempts at cardiopulmonary resuscitation. BMJ 2011, 343:5942 Blinderman et al, Time to revise the approach to determining CPR status, JAMA 2012, 307:917-18 Opt in not out • Vocal criticism of “the slow code” although • Some ethicists state that the “slow code” may be a method of meeting the needs of family and patient1 Lantos et al, Should the slow code be resuscitated? Am J Bioeth 2011, 11:8-12 Resuscitation in the elderly Predictors of survival following in-hospital cardiopulmonary resuscitation, CMAJ 2002, 167:343-8 Resuscitation in the elderly In a 1989 study, 503 inpatients over 70: •22% survived initially, 9.6% survived to discharge •Unwitnessed arrest – 1/116 survived •PEA or asystole – 1/237 survived •CPR > 15 minutes – 1/360 survived •Acute care hospital inpatients – 17/259 survived •Most survivors had VT or VF that was witnessed Outcomes of cardiopulmonary resuscitation in the elderly, Annals of Internal Medicine, 1989, 111:199-205 When is it futile? Cardiac arrest Respiratory arrest Predictors of survival after cardiac or respiratory arrest, CMAJ, 2011, 183:1589-94 Greek Cardiologist’s Knowledge of CPR Pantazopolous et al, Carrdiologists’ knowledge of the 2005 American Heart Association Guidelines, Heart and Lung 2011, 40:278-84 The Quilty Take – GIVE UP • No CPR on unwitnessed arrest in patients > 80 • All inpatients not monitored and >80 are NFR • Discussion with susceptible patients who are unlikely to benefit from CPR before arrest situation – Should the patient be give an option? • If over 70 and >10 minutes, call it quits • If PEA or asystole and over 70, call it quits The Quilty Take – GIVE ‘EM A GO • Early defibrillation if witnessed • High quality chest compressions of: – adequate depth – rate – complete chest wall release b/n compressions – minimal hands off time • Keep pumping until defib ready to go • Go slowly with resps, aim for SaO2 88-95% • ED form documenting resus status for all over 70? • Always consider the damage that might have occurred The Quilty Take • Formalise resuscitation processes in the hospital, including expanded register to include outcomes • Train all medical registrars • In-hospital protocol for cardiac arrest, ie immediate revascularization, immediate ECHO, use of ultrasound etc? Quilty Take • Average age of 99 resuscitated in 2005? – 71 • Average age of the 85 resuscitated 2011? – 71 • Age of the oldest survivor in 2011? – 90 (G1) • How many were over 90 in 2011? –4