Paediatric Resuscitation Guidelines 2010 - Vula
advertisement
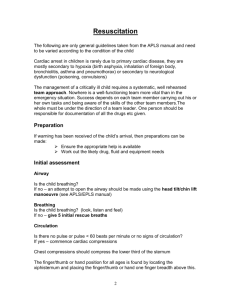
Cardiopulmonary Resuscitation Shamiel Salie Paediatric Intensive Care Unit Red Cross Children’s Hospital, University of Cape Town Basic Life Support SAFE approach Are you alright? Airway opening manoeuvres Look, listen, feel 5 rescue breaths Check pulse Check for signs of circulation CPR 15 chest compressions 2 ventilations 1 minute Call emergency services Age Definitions: • Newborn • Infant - under 1 year • Child - from 1 year to puberty 2005 BLS Changes: • Lay rescuers should start compressions for an unresponsive child who is not breathing/moving • Universal compression-ventilation ratio of 30:2 for the lone rescuer of infants, children and adults • Increased evidence on the importance of uninterrupted chest compressions Compression Techniques Position: for all ages: compress the lower third of the sternum number of hands: • In infants: two thumbs or two fingers • in children: use one or two hands: depressing the sternum by approximately one third of the depth of the chest Chest Compressions • Push hard • Push Fast • Complete chest recoil • Minimize interruptions Calling for help!! • Perform 5 cycles or about 2 minutes of CPR before calling for help • Indications for activating EMS before BLS by a lone rescuer are: – witnessed sudden collapse with no apparent preceding morbidity – witnessed sudden collapse in a child with a known cardiac abnormality Choking Assess Ineffective cough Effective cough Conscious Unconscious 5 back blows Open airway 5 chest/abdo thrusts 5 rescue breaths Assess and repeat CPR 15:2 Check for FB Encourage coughing Support and assess continuously Universal Algorithm Stimulate and assess response Open airway Check breathing 5 rescue breaths Check pulse Check for signs of circulation CPR 15 chest compressions 2 ventilations VF/VT Assess rhythm Asystole and PEA Asystole and PEA Ventilate with high concentration O2 Continue CPR Intubate IV/IO access Adrenaline 10 mcg/kg IV or IO 4 min CPR Check monitor every 2 minutes Consider 4 Hs & 4 Ts Consider alkalising agents DC Shock 4J/kg VF/VT 2 min CPR, check monitor Intubate, High flow O2 IV/IO access DC Shock 4J/kg 2 min CPR, check monitor Intubate IV/IO access Adrenaline then DC Shock 4J/kg 2 min CPR, check monitor Amiodarone then DC Shock 4J/kg 2 min CPR, check monitor Adrenaline then DC Shock 4J/kg 2 min CPR, check monitor DC Shock 4J/kg 2 min CPR, check monitor Adrenaline dose 10 mcg/kg Consider 4 Hs 4 Ts Consider alkalising agents Neonatal Resuscitation Drugs in Cardiac Arrest • 10mcg/kg of adrenalin as the first and subsequent iv doses. • high dose iv adrenalin is not recommended and may be harmful • Insufficient evidence to recommend for or against the routine use of vasopressin in children Route of drug delivery in ALS • where possible give drugs intra-vascularly rather than via the tracheal route – lower adrenaline concentrations may produce transient beta adrenergic effects resulting in hypotension. • Intra-osseous access is safe for fluid resuscitation and drug delivery. Airway Management • guedel airways • laryngeal airways • Cuffed or uncuffed endotracheal tubes Do children have Ventricular fibrillation? Number of Defibrillating Shocks • one shock rather than three “stacked” shocks • Modern biphasic defibrillators have a high first shock efficacy • Most patients have a non perfusing rhythm after successful defibrillation European Resuscitation Council AED IN CHILDREN • Age > 8 years • use adult AED • Age 1-8 years • use paediatric pads / settings if available (otherwise use adult mode) • Age < 1 year • use only if manufacturer instructions indicate it is safe Fluid Resuscitation • Boluses of fluid may be required to maintain systemic perfusion • Crystalloids - ringers or normal saline • Septic children may require in excess of 100ml/kg fluid resuscitation Family Presence during Resuscitation • Evidence suggests that the majority of parents would like to be present during resuscitation, that they gain a realistic understanding of the efforts made to save the child, and they subsequently show less anxiety and depression. When do you start? When do you stop? • In the absence of reversible causes eg drowning with severe hypothermia, poisoning, prolonged CPR in children is unlikely to result in intact neurological survival. • One should consider stopping resuscitation after 20 minutes. Post Resuscitation Care • Ventilate to normo-capnoea • Hypothermia for 12-24 hours post arrest may be helpful, whilst hyperthermia should be treated aggressively • Vaso-active drugs should be considered to improve haemodynamic status. • Maintain normoglycaemia Conclusions: • The 2005 guidelines minimizes the differences in the steps and techniques of CPR used for infants, children and adults. • Push hard, push fast, minimizing interruptions • Respiratory failure and hypoxia is the commonest reason for paediatric arrests. • There are usually warning signs of impending doom, and early and effective therapy will prevent cardiac arrest Questions