CASE PRESENTATION ON
SUBARACHNOID HEMORRHAGE
PREPARED BY:
TONI P TENI
STAFF NURSE, ICU DEPARTMENT
I.
DEMOGRAPHIC DATA
CASE NO: 193525
NAME: XYZ
AGE: 24YRS
SEX: MALE
DIAGNOSIS:H/O FALL WITH HEAD
INJURY, SAH,CRANIOTOMY DONE FOR
LEFT SIDE SAH,#C2,#T9-T12-L1,# RIGHT
ZYGOMATIC ARCH.
DOA: 01/01/2013
PHYSICAL ASSESSMENT
An assessment is conducted starting at the head and
proceeding in a systemic and efficient downward
(head to toe). The procedure varies according to age,
belief, religion of the subject, the severity of illness of
the patient, the location of the examination, the
priorities and procedures.
General Assessment:
The patient is 24 years of age, MALE,
approximately weighs 50kg.
He is unconscious on ventilator support. GCS
3/15, with the following Vital Signs:
BP= 120/70 mmHg
PR=110 bpm
RR= 20 mts
Temp=37.4 ⁰C
SPO²= 98%
Skin:
Warm.
Laceration on the right ear and left knee.
Redness on the right hand.
Head:
Scalp swelling in right parietal area.
No palpable masses and lesions.
Level of Consciousness and
Orientation:
Patient is unconscious.
On fully sedation.
On ventilator
Eyes:
Redness on the right eyes.
Pupils – R-1MM reactive.
L-5MM fixed and dilated.
Ears:
No unusual discharges noted.
Nose:
No unusual nasal discharges.
Neck and Throat:
No palpable lymph nodes.
No masses and lesions seen.
Chest and Lungs:
B/L good air entry.
Clear breath sounds.
Heart:
Tachycardia
Abdomen:
Soft abdomen
USG report:
Minimal free fluid in the abdomen
Genitals:
Minimal pubic hair.
No usual bleeding
Extremities:
Pulse full and equal
No lesions noted
III. PATIENT HISTORY
PAST MEDICAL HISTORY
24YRS Yemeni patient H/O fall down from
height, admitted the patient in ER via RED
CROSS ambulance. On the time of admission in
ER patient was unconscious and agitated, GCS
3/15, patient was intubated and sedated, after all
investigation (BLOOD+CT) patient shifted to
ICU.
PRESENT MEDICAL HISTORY
Received the patient from ER , patient was intubated
and sedated, keep the patient in ventilator IPPV mode
FIO2-100%,RATE-18,TV-450,PEEP-5,patient is on
Propofol,Morphin, Nimbex and Midazolam infusion
fully sedation. CT Scan of Brain shows subarachnoid
hemorrhage along left fronto-parieto-temporal areas
diffuse brain edema evidenced by sulcal and cisternal
effacement associated with midline shift to right side
15 mm and compression of the lateral and third
ventricles. Patient prepared for urgent craniotomy,
consent taken, 4 PRBC arranged, PAC done, head
shave done and patient shifted to OT.
After craniotomy with evacuation of SAH received
the patient in ICU. Patient is on ventilator and fully
sedated. After surgery pupils left 4MM nonreactive
and right 2MM reactive. Maxillofacial, ENT,
Opthalmo consultation done. Cervical collar and DVT
pump applied. After all management patient was
improved and patient was extubated and fully
conscious, pupils B/L 2MM reactive. Patient was
shifted to surgery ward.
IV. MEDICATION
DRUG
DOSE ROUTE ACTION
INJ:AUGMENTIN 1.2GM
I/V
ANTIBIOTIC (GENERATION2)
INJ:CEFTRIAXO
NE
2GM
I/V
ANTIBIOTIC (GENERATION2)
INJ:RISEK
40MG
I/V
H2RECEPTER
INJ:MANNITOL
100ML
I/V
DIURATICS
INJ:PHENYTOIN
100MG
I/V
ANTICONVELCENT
V. INVESTIGATION
TEST
PATIENT VALUE
NORMAL VALUE
UREA
6.1
1.8 TO 8.3
CREATININE
63.5
58 TO 110
SODIUM
140
135 TO 150
POTASSIUM
3.3
3.5 TO 5.0
MAGNESIUM
0.75
0.65 TO 1
WBC
13.72
4.23 TO 9.07
HGB
12
13.7 TO 17.5
PLT
197
163 TO 337
PT
13.6
10.9 TO 16.3 SEC
INR
1.00
2 TO 4
APTT
34.2
27 TO 39 SEC
CALCIUM
2.27
2.20 TO 2.55
Non Contrast CT Brain:
There is
subarachnoid hemorrhage along left
fronto-parieto-temporal areas.diffuse brain edema
evidenced by sulcal and cisternal effacement
associated with midline shift to right side 15 mm
and compression of the lateral and third ventricles.
CT Chest with IV Contrast:
Suspected fracture is seen in the left scapula
CT Lumbosacral Spine:
Compression fracture is seen in the body of L1
CT Thoracic Spine:
Fracture is seen in the right lamina of T9
Compression fracture is seen in the bodies of T9
and T12
Fracture is seen in both transverse processes of T9
CT Cervical Spine:
Normal Study
USG Abdomen:
Minimal free fluid in the abdomen
VII.
INTRODUCTION
In subarachnoid hemorrhage (SAH), ruptured vessels
lead to bleeding into the subarachnoid space. The
blood mixes with the cerebrospinal fluid, and can be
irritating to the meninges. Blood quickly fills the area
immediately surrounding the brain and spinal cord
(called the subarachnoid space). This space contains
the cerebrospinal fluid. The fluid cushions and bathes
the brain and spinal cord.
VIII.
DEFINITION
Subarachnoid hemorrhage: A bleeding into the
subarachnoid, the space between the arachnoid and the
pia mater, the innermost membrane surrounding the
central nervous system. Subarachnoid hemorrhage
typically occurs when an artery breaks open in the brain,
such as from a ruptured aneurysm.
Subarachnoid hemorrhages are classified into two
general categories: traumatic and spontaneous.
IX.
ILLUSTRATION
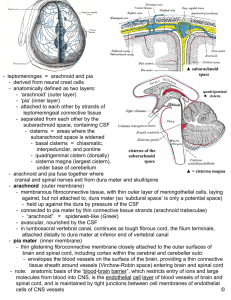
X. ANATOMY AND PHYSIOLOGY
The meninges is the system of membranes which envelops
the central nervous system. In mammals, the meninges
consist of three layers: the dura mater, the arachnoid
mater, and the pia mater. The primary function of the
meninges and of the cerebrospinal fluid is to protect the
central nervous system.
Dura mater:
The dura mater (also rarely called meninx fibrosa) is a
thick, durable membrane, closest to the skull. It consists of
two layers, the periosteal layer which lies closest to the
calvaria (skull), and the inner meningeal layer which lies
closer to the brain. It contains larger blood vessels which
split into the capillaries in the pia mater. The dura mater
surrounds and supports the large venous channels (dural
sinuses) carrying blood from the brain toward the heart.
Arachnoid mater:
The middle element of the meninges is the
arachnoid mater, so named because of its spider
web-like appearance. It provides a cushioning effect
for the central nervous system. The arachnoid mater
is a thin, transparent membrane. It is composed of
fibrous tissue and, like the pia mater, is covered by
flat cells also thought to be impermeable to fluid.
The arachnoid and pia mater are sometimes
together called the leptomeninges.
•
Pia mater:
The pia mater [is a very delicate membrane. It is the meningeal
envelope which firmly adheres to the surface of the brain and spinal
cord. It is a very thin membrane composed of fibrous tissue covered
on its outer surface by a sheet of flat cells thought to be impermeable
to fluid. The pia mater is pierced by blood vessels which travel to the
brain and spinal cord, and its capillaries are responsible for
nourishing the brain.
Spaces:
The subarachnoid space is the space which normally exists between
the arachnoid and the pia mater, which is filled with cerebrospinal
fluid.
Normally, the dura mater is attached to the skull, or to the bones of
the vertebral canal in the spinal cord. The arachnoid is attached to the
dura mater, while the pia mater is attached to the central nervous
system tissue. When the dura mater and the arachnoid separate
through injury or illness, the space between them is the subdural
space.
XI. ETIOLOGY
Aneurysm: a balloon-like bulge or weakening of an artery
wall that ruptures, releasing blood into the subarachnoid space
around the brain.
•
Arteriovenous malformation (AVM): an abnormal tangle
of arteries and veins with no capillaries in between. The
weakened blood vessels can rupture and bleed
•
About 1% of people have a congenital defect which
affects their blood vessels in the brain. Some blood vessels have
weak and thin walls.
•
There is a greater risk of an aneurysm rupturing if you
smoke, drink alcohol regularly in large quantities, and suffer from
hypertension (high blood pressure) and do not control it properly.
•
A severe head injury can also be a cause of a
subarachnoid hemorrhage
•
Traumatic brain injury. Traumatic SAH usually occurs
near the site of a skull fracture or intracerebral contusion.
•
VI. PATHOPHYSIOLOGY
XII. SIGNS AND SYMPTOMS
The main symptom is a severe headache that starts
Stiff neck
Nausea
Vomiting
Slurred speech
Depression, confusion, delirium, and possibly apathy
Impaired consciousness, sometimes total loss of consciousness
Seizures (in about 1 in every 14 cases)
Sometimes there may be intraocular hemorrhage (bleeding into the eyeball)
Some patients may find it hard to lift an eyelid
Sharp increase in blood pressure
Other symptoms:
Mood and personality changes, including confusion and irritability
Muscle aches (especially neck pain and shoulder pain)
Vision problems, including double vision, blind spots, or temporary vision
loss in one eye
Pupil size difference
XIII.
INTERVENTION
Nursing intervention includes:
24 hours vital sings observation will be monitored and
documented.
Assess neurological status especially pupils through Glasco coma
Scale daily.
Helps the patient to do ADL activities
Give all due medication on time
Institute safety of the patient:
Fall prevention: Side rails up
Bed in low position
Prevent infection and other potential complications
Provide client and family education about treatment and recovery
of the patient.
XIV.
TREATMENT
Treatment for SAH varies, depending on the underlying
cause of the bleeding and the extent of damage to the
brain. Treatment may include lifesaving measures,
symptom relief, repair of the bleeding vessel, and
complication prevention.
For 10 to 14 days following SAH, the patient will remain
in the neuroscience intensive care unit (NSICU), where
doctors and nurses can watch closely for signs of
renewed bleeding, vasospasm, hydrocephalus, and other
potential complications.
Medication:
Pain medication will be given to alleviate headache, and
anticonvulsant medication may be given to prevent or treat
seizures, antibiotics give to prevent infection after surgery.
Surgery:
If the SAH is from a ruptured aneurysm, surgery may be
performed to stop the bleeding. Options include:
Surgical clipping: an opening in the skull (craniotomy) is made
to locate the aneurysm. A small titanium clip is placed across
the neck of the aneurysm to stop blood flow from entering.
Endovascular coiling: a catheter is inserted into an artery in the
groin during an angiogram. The catheter is advanced through
the blood stream to the aneurysm. Platinum coils or liquid glue
(Onyx) are packed into the aneurysm to stop blood flow from
entering.
XV. COMPLICATIONS
Hydrocephalus
Rebleeding
Delayed cerebral ischemia from vasospasm
Intracerebral hemorrhage
Intraventricular hemorrhage
Left ventricular systolic dysfunction
Subdural hematoma
Seizures
Increased intracranial pressure
Myocardial infarction
XVI. PRIORITIZATION OF NURSING
PROBLEMS
Headache associated with vascular disease like subarachnoid hemorrhage.
Risk for infection related to surgery.
In effective feeding pattern related to Impaired ability of the patient to coordinate swallow response resulting inadequate nutrition, Impaired
swallowing, Deficient fluid volume, Imbalanced nutrition less than body
requirement, Risk for electrolyte imbalance.
Impaired urinary elimination due to urinary retention, bowel incontinence.
Impaired sleep pattern related due to impaired physical mortality, Risk for
activity intolerance, Ineffective peripheral tissue perfusion, Self care deficit.
Alteration in consciousness due to decreased nerve and brain function.
Risk for fall due to semiconscious.
Risk for developing pressure ulcers due to prolonged bed ridden.
Disturbed sensory perception (photophobia) related to severe headache.
Self-care deficit due to weakness and numbness in body part.
XVIII. NURSING HEALTH TEACHING
Remain on modified bed rest
Take medication prescribed.
Follow up regularly
Take adequate nutrition
Maintain personal hygiene
Maintain skin care
Regularly checkup vitals.
XIX. CONCLUSION
SAH is a medical emergency which is prevented
if the risk factors are reduced. In case of head
injury, the patient brought immediately to the
hospital and give immediate care, we can save
the life. The manifestations and recovery depend
on the location and severity of the damage or
bleeding in the patient brain.
XX. BIBLIOGRAPHY
Wikipedia.
Medical and surgical nursing book volume 1 and
2 of Brunner.
Luck man and Sorensen’s Medical-Surgical
Nursing a Physiologic Approach 4th edition
Lippincott Manual of Nursing Practice 9th
edition.