Document
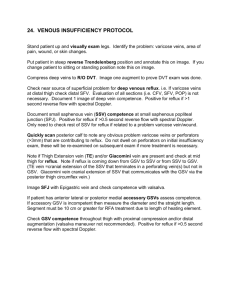
advertisement
Laser Therapy of Perforator Veins Michael F. Bardwil M.D.,F.A.C.S. Current Treatment of Veins Saphenous Veins Laser Ablation Varicose Veins •Phlebectomy •Foam Sclerotherapy Telangectasia and Reticular Veins Sclerotherapy Perforator Veins Next area in treatment of veins Why does Vein Surgery Have Such a Bad Reputation? • Historically the procedures were morbid • High incidence of recurrence perceived as bad results • Severe forms of venous insufficiency including refluxing perforators resulted in recurring stasis ulcers Perforators Give Veins A Bad Name • Linton procedure had a reported 19% wound complication rate Perforators Give Veins A Bad Name • Perforators are a more likely source for recurrent varicose veins than neo-vascularsation • Recurrence is perceived as bad results Perforators Give Veins A Bad Name • Severe forms of venous insufficiency including refluxing perforator veins resulted in recurring stasis ulcers Significance of Perforator Veins • Source for reflux in the superficial venous system • Reflux from perforator veins has been associated with venous stasis ulcers • Communication between deep and superficial venous Systems • Reflux from perforator veins can result in varicose veins Communication Between Venous Systems • Not all bad • Allows patients to recover from vein insults such as injuries and DVT • Allows us to perform vein ablative procedures on the saphenous and other superficial veins Communication Between Venous Systems • • • • Not all good Source for reflux in the saphenous vein Associated with venous stasis ulcers Reflux from perforators can cause non saphenous varicose veins • Source for new and recurrent varicose veins Types of Perforators • • • • • Hunterian Dodd’s Boyd Cockett’s New Nomenclature Hunterian and Dodd’s Perforator • Connect femoral and proximal popliteal perforators to the saphenous vein • Reflux from these perforator veins results in varicose veins in the middle and distal third of the medial thigh • Stripping reportedly interrupts all but 8%? Boyd’s Perforators • Perforator just distal to the knee • Connects saphenous veins to popliteal vein • Varicose veins medial leg upper third • May appear as first place isolated reflux • New nomenclature Paratibial perforators Cockett’s Perforators • Cockett’s I perforator posterior to medial malleolus • Cockett’s II perforator 7-9cm proximal • Cockett’s III perforator 10-12 cm proximal • New nomenclature posterior tibial Less Discussed Perforators Indications for Treatment • Venous Stasis Ulcer associated with perforator vein 2-4 mm in size Indication for Treatment • Large perforator vein 3-4mm noted at the time of saphenous ablation • Refluxing perforator 2-4 mm noted at saphenous ablation Indications For Treatment • Perforator veins refluxing into varicose veins that are not associated with long or short saphenous reflux Indications for treatment • Recurrent varicose veins that appear to originating from refluxing perforator Indication for Treatment • Perforator veins refluxing into varicose veins that are not associated with long or short saphenous vein reflux • Large perforator veins 2-4mm noted at time of saphenous ablation • Recurrent varicose veins that appear to be originating from perforator • Stasis ulcers associated with perforator History • Standard questions regarding symptoms • Previous vein surgery • Stasis Ulcers and previous treatment Examination • Physical exam with attention to pattern of varicose veins • Use the ultrasound as an extension of the physical exam • Photograph markings of perforator to be treated • Ulcers • PPG to physiologically document venous insufficiency Problems with Perforator Rx • Linton procedure problem with wound healing • SEPS general anesthesia required inconsistent results • Ultrasound guided foam multiple sessions inconsistent results, non approved solution no code for reimbursement Future Meets Past • • • • • In office procedure to treat perforators Less morbid Addresses non saphenous varicose Veins Addresses sources of recurrence Addresses stasis ulcers Endoluminal Ablation Perforators Endoluminal Ablation of Perforators • • • • • • Minimally invasive procedures Office based Local anesthesia VNUS Closure Laser ablation My experience VNUS Closure • Device FDA approved • Billing Code recommendation • Recommended protocol using ultrasound guidance and impedance to verify position Disadvantage VNUS Closure • Device awkward and expensive, especially for add on perforator veins • Protocol less effective than thought • Impedance less useful than flash • In general other closure procedures have inferior results to laser Laser Perforator • Technically simpler • Less expensive to perform; can treat perforator at time of other veins and not incur increase procedural costs • Results should be superior to closure Technical Issues • • • • Visualization Broad based neck Multiple perforator necks Long Perforator necks Technique My Experience • • • • • • • • Micro puncture kit Angio cath catheter 18 gauge thin wall angiogram needle 25 gauge “finder” needle 20 gauge needle with 400u fiber 20 gauge needle with 600u fiber Laser setting Use of foam Micro-Introducer • Advantage theoretically similar Elas • Disadvantage not enough room to place guide wire in far enough for introducer Dr. Murphy technique use stiff end of guide wire Angiocath • Advantage: Able to place without guide wire • Disadvantage: Needle may be in, but laser not. Work with VNUS device demonstrated proximity still only applies to horse shoes and hand grenades 18 gauge Angiogram Needle • Advantage: Direct access to vein • Disadvantage: Still bulky, at times difficult getting fiber through needle 20 Gauge Needle 400u Fiber • Advantage: Easier to use technically to access vessel • Can access vessel at more than one spot • Disadvantage: Inconsistent delivery of Energy if Laser system made for 600u fiber How I Do It • Always perform the venous duplex yourself • Mark the vein with patient standing or sitting with feet dangling • Strategically position patient • Put the bed in reverse trendlenberg How I Do It • Re-map and mark patient in new position • Use 25 gauge “finder” needle • Place previously 2 inch stripped fiber through 20 gauge needle and mark with steri-strip • Access vein with 20 gauge needle, use more than one needle if necessary • Inject local anesthesia after you are in vein How I Do It • Laser setting 15 watts intermittent 1.5 sec duration, 1 sec rest • Look for steam in vessel • I usually deliver 200-300 joules • Steri strip applied. 4x4,kerlex, co-ban Follow Up • 1-2 days remove wrap and ultrasound • Low threshold to use foam at time of this exam Results • In progress