The Role of the Technologist in Pre
advertisement
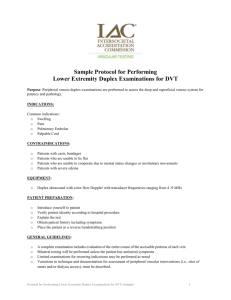
The Role of the Technologist in Pre-Op Surgical Planning for AVF/AVG David Lorelli, MD, RVT, FACS Medical Director Vascular Lab St John Hospital and Medical Center Detroit, Michigan Table of Contents • • • • • • • • • Upper Extremity Anatomy Basics of an Arteriovenous Fistula Arteriovenous Graft (AVG) Access Performance Upper Extremity Duplex Information for the Physician Vein Mapping Limitations Helpful Scanning Techniques Upper Extremity Anatomy • Deep Veins - Jugular - Subclavian - Axillary - Brachial - Radial - Ulnar • Superficial Veins - Cephalic - Basilic - Medial cubital vein What is an Arteriovenous Fistula (AVF) • Patients who are in kidney failure need hemodialysis to supplement their kidney function. • An arteriovenous fistula is the connection of a vein and an artery to allow access to the vascular system for hemodialysis. • The surgical creation of an AVF provides a long-lasting site through which blood can be removed and returned to the body during a hemodialysis treatment. • The fistula, which allows the person to be connected to a dialysis machine, must be prepared by a surgeon weeks or months before dialysis is started. • It takes approximatley 4-12 weeks for an AVF to fully mature. Basics of an Arteriovenous Fistula • The venous system contains Deep and Superficial veins. The Superficial system is most important for AVF creation. • Cephalic vein is most commonly utilized. - radiocephalic and brachiocephalic • All Cephalic options are considered before the proximal Basilic vein. • Basilic vein is second choice because it lies beneath the deep fascia and must be brought more superficial. This is known as a Transposed Basilic vein AVF. • Brachial veins can also be used for access. Arteriovenous Graft (AVG) • If all native vessels are not suitable for creating an AVF then a graft made of synthetic material is utilized. • Common material is Polytetrafluoroethylene (PTFE) • Types of loops include: Forearm loop, upper arm straight or loop, and thigh loop. Access Performance • Rate of blood flow varies depending on the anatomy of the access: AVF with radial artery 600-700 ml/min AVF with brachial artery 13001500 ml/min AVG 800-1200 ml/min Factors Affecting Blood Flow Rates • Performance of the blood pump (heart) Blood pressure, ejection fraction, cardiac rhythm • Cardiac output also affected by Fluid volume status, BP medications, cardiac disease • Atherosclerosis causing flow limiting stenosis Blood Flow Rates • Any factor which decreases the rate of intra access blood flow can lead to suboptimal hemodialysis treatments and may eventually increase patient morbidity and mortality. Upper Extremity Duplex • An ultrasound is done to determine the patency, size and condition of the veins. • Generally a full evaluation of the venous system is completed to rule out DVT. • Diameter measurements are taken of the superficial veins . - Proximal, mid, distal upper and lower Cephalic. -Proximal, mid, distal upper and lower Basilic. - If visualized, measure the medial cubital vein. • Depending on the physician, diameter measurements are taken of specific arteries. Diameter measurement of the Cephalic Vein. Information for the Physician • Dominant arm of the patient • Any branches that come off the superficial veins • Any dilations in the veins • Thickening of the vessel walls • If DVT or SVT is visualized • Any areas of stenosis. • Any limitations Information for the Physician • Once the duplex is finished, the physician makes the decision of which fistula or graft is best for the patient. • 2-2.5 mm and above are acceptable diameter measurements for a fistula. • The non-dominant hand is preferable. Vein Mapping • The day of the surgery the technologist needs to mark the exact location and where the vein courses down the arm. • With a permanent marker, the tech keeps the vein in the middle of the screen and writes on the patients arm at the center of the probe to ensure the right area is being mapped. • Follow the vein as far proximal and distal as possible. • Also mark any branches that might be coming off the vein. • The physician may also need to know how far the vein is from the skin. Measure from the top of the vein to the top of the screen. Limitations • • • • • Obese patients with deep vessels A cast that limits the scanning area Trauma or open wounds Severe edema Central venous line or dialysis access Helpful Scanning Techniques • If the vein is very superficial and the weight of the probe is collapsing the vein, stabilize your hand on the patients arm to release some pressure from the probe. • Switch to a higher frequency probe to visualize the superficial veins better. • When mapping for surgery, a tourniquet can be used to better visualize the veins. • Do not leave the tourniquet on for too long or have it too tight, just enough to help the veins be more visible. New Alternatives • HeRO catheter/graft Allows upper extremity access even with peripheral venous outflow obstruction. The HeRO Graft (Hemodialysis Reliable Outflow) HeRO Graft is the only fully subcutaneous HeRO bypasses central venous stenosis AV access solution clinically proven to maintain long-term access for catheterdependent patients with central venous stenosis. New Alternatives • TEVG (Tissue Engineered Vascular Graft) Built to tolerate hemodynamic loads, heal and remodel in response to needle sticks, resist infection, no post op maturation period. Currently the major draw back is cost effectiveness. References ACR–AIUM–SRU Practice Guideline for the Performance of Peripheral Venous Ultrasound Examination. 2010. American College of Radiology. http://www.acr.org/SecondaryMainMenuCategories/qualitysafety/guidelines/us/us_peripher al_venous.asp Atlas of Dialysis Vascular Access. Tushar J. Vacharajani. 2010. Mayo Foundation for Medical Education and Research (MFMER).March 2010. http://www.mayoclinic.com/health/arteriovenous-fistula/DS01171 Upper Extremity Venous Duplex Evaluation R/O Deep/Superficial Vein Thrombosis. Society for Vascular Ultrasound. January 2010. http://www.svunet.org/files/positions/Upper_Extremity_Venous_ Duplex_Eval_2010.pdf Vascular Access to Hemodialysis. National Kidney and Urologic Disease Information Clearinghouse, Home Health Information. December 1999. http://www.niddk.nih.gov Questions