Duplex ultrasound investigation of the veins in CVD of the lower limbs
advertisement
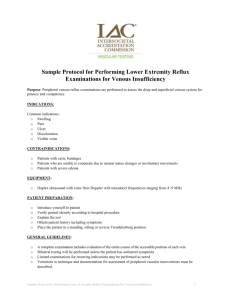
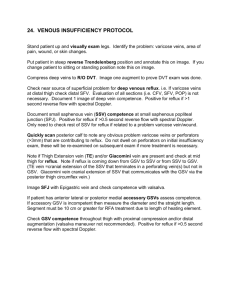
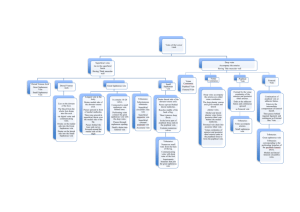
Endovenous Treatment of Venous Diseases: Preprocedural assessment, indications and contraindications Athanasios D. Giannoukas MD, MSc(Lond.), PhD(Lond.), FEBVS Professor of Vascular Surgery Faculty of Medicine, University of Thessalia, Greece Chairman, Dept. of Vascular Surgery, University Hospital of Larissa Larissa, Greece GSV Before Treatment Image courtesy of Olivier Pichot, MD, CHU de Grenoble, France. GSV After Treatment Image courtesy of Olivier Pichot, MD, CHU de Grenoble, France. CEAP Clinical Classification Class 0: Asymptomatic; no visible or palpablesigns 1: Spider veins, reticular veins, telangiectasias 2: Varicose veins 3: Edema 4a: Skin changes with hyperpigmentation and eczema 4b: Skin changes with lipodermatosclerosis and atrophie blanche 5: Healed ulcer 6: Active ulcer CEAP Clinical Classifications Clinical Etiology Anatomy Pathophysiology Varicose Veins CEAP 2 Swelling CEAP 3 Skin Changes CEAP 4 Skin Ulcer CEAP 6 Is pre-op duplex assessment important for varicose vein surgery? Ultrasonic assessment Explanation Information provided by DS will have significant impact on the selection of appropriate treatment Failure to identify all sources of venous filling is likely to result in early recurrence Indications for Duplex Scan Recommendation: both limbs should be studied Primary uncomplicated GSV VVs Debated whether all pts – if not 30% of important connections between deep and superficial veins will be missed Primary uncomplicated LSV VVs Essential Non-saphenous & Recurrent VVs Essential CVD with complications Essential Surveillance after treatment the only way to obtain level I evidence as to outcome in the future Venous malformations anatomical information about the extent of the malformation and its relationship to other vessels may be used to guide treatment by sclerotherapy Position of the patient Greater saphenous Position of the patient Lesser saphenous Anatomy of superficial veins of the lower limb Important anatomical details Anatomical structures on B-mode GSV Bound anteriorly by superficial fascia & posteriorly by deep fascia Often called “saphenous eye” Fascial layers creating “saphenous eye” Images courtesy of Olivier Pichot, MD GSV Variables Tortuosity Images courtesy of Olivier Pichot, MD Side branches GSV Variables Aneurysmal segments SFJ Tributary Veins SCI: Superficial Circumflex Iliac SE: Superficial Epigastric SEP: Superficial External Pudendal AASV: Anterior Accessory Saphenous PASV: Posterior Accessory Saphenous Image adapted from: Chandler JG et al. Defining the role of extended saphenofemoral junction ligation: A prospective comparative study. JVS 2000;32:941-53 Initial Catheter Tip Positioning Position catheter tip approximately 2.0 cm distal to SFJ ◦ Confirm with measurement calipers ◦ Distance does not need to be precise at this time because catheter position may shift during tumescent fluid infiltration Final Tip Position Verification Recommendation is 2.0 cm distal to SFJ Confirm tip position with ultrasound: ◦ In both transverse and longitudinal imaging planes ◦ Use measurement calipers to confirm distance to SFJ Important step to avoid misaligning catheter relative to deep venous system Image courtesy of Pranay Ramdev, MD Anatomical structures on colour facility Small Saphenous Vein (SSV) Courses from lateral ankle up posterior calf Terminates in popliteal fossa at Saphenopopliteal Junction (SPJ) ◦ Variable confluence with Popliteal Vein (PV) ◦ Proximal portion lies between superficial & deep fascial layers SPJ Pop V SSV Figure adapted from: Weiss RA, et al eds. Vein diagnosis and treatment: A comprehensive approach. McGraw-Hill Companies, Inc.; 2001. Anatomical structures on colour facility Detection of reflux on colour facility Detection of reflux on colour facility Detection of reflux on colour facility Detection of reflux on colour facility Perforating vein If reflux is present measure the diametre but this cannot distinguish competent from incompetent Duration of reflux Detection of reflux on Doppler Reflux is present when retrograde flow lasts for at least 1 sec Patient selection for Endovenous Alation Identification of all refluxing venous segments and their ablation is the key to minimise recurrence Diametre of central GSV > 15 mm may be associated with thrombus extension to CFV Uncorrectable coagulopathy Liver dysfunction limiting local anaesthetic use Immobility Pregnancy Breastfeeding Contraindication Thrombus in the vein segment to be treated Choosing the Closure Candidate Preoperative ultrasound evaluation ◦ Reflux > 0.5 seconds in superficial venous system ◦ Assess GSV, noting: Vein depth and maximum diameter Presence of tortuous or aneurysmal segments Other significant anatomy Duplicate systems Large side branches Incompetent perforators or tributaries Vein depth from the skin: Why is so important? The aim of ablation procedures is to damage the inner vein wall without causing a full-thickness burn, which could lead to perforation of the vein resulting in bruising or haematoma formation If vein lies superficially, close to skin the ablation may cause burn Pre-op Ultrasound Assessment Map and mark ◦ ◦ ◦ ◦ Maximum diameter Tortuous segments Aneurysmal segments Areas where vein is very close to skin ◦ Large branches or perforators ◦ Potential access sites Infiltration Technique Do not leave any vein segments unprotected ◦ Re-scan to ensure: • >10 mm distance between skin surface and vein wall • Circumferential black “halo” appearance in fascial compartment Perivenous vs. subcutaneous infiltration Image courtesy of Carolyn Menendez, MD Vein Mapping Make indentions in skin using a straw Remove US gel from leg Connect marks on leg with marker to identify pathway of vein and important anatomy Image courtesy of Nick Morrison, MD Pre-op Descending Venography Selective descending ovarian and hypogastric venogram Significant ovarian vein reflux but No hypogastric vein reflux was detected Hypogastric vein reflux Ovarian vein reflux Descending Ovarian Venogram 4 weeks after embolisation Hypogastric vein embolisation CT venography Chronic Venous Obstruction DP=8 mmHg DP=22 mmHg DP=2 mmHg IVC filter placement Indications DVT and covtraindication for anticoagulation Reccurent PE being on adequate anticoagulation Pre-procedural evaluation MR or CT venography is required for IVC and iliac vein patency and IVC diametre measurement Thank you for your attention