Transcatheter vs. Surgical Aortic
Valve Replacement in High Risk
Patients with Severe Aortic Stenosis:
Results From The PARTNER Trial
Craig R. Smith, MD
on behalf of The PARTNER Trial Investigators
ACC 2011 | New Orleans | April 3, 2011
Presenter Disclosure Information
for PARTNER at ACC April 3, 2011
Craig R. Smith, MD
PARTNER Trial sponsor (Edwards LifeSciences)
reimburses customary travel and other expenses
Background
• Surgical aortic valve replacement (AVR) is the
standard of care for treating patients with
symptomatic aortic stenosis who are candidates
for operation.
• Although transcatheter aortic valve replacement
(TAVR) reduces mortality in patients who cannot
have AVR, there have been no randomized trials
comparing TAVR to AVR in patients who are at
high-risk for operation.
Purpose
To compare the safety and effectiveness of
TAVR (either transfemoral or transapical) to
surgical AVR in high-risk, operable patients
with symptomatic, severe aortic stenosis.
PARTNER Study Design
Symptomatic Severe Aortic Stenosis
ASSESSMENT: High-Risk AVR Candidate
3,105 Total Patients Screened
Total = 1,057 patients
N = 699
High Risk
Inoperable
2 Parallel Trials:
Individually Powered
N = 358
ASSESSMENT:
Transfemoral
Access
Yes
No
1:1 Randomization
N = 179
N = 179
TF TAVR
Standard
Therapy
Not In Study
VS
Primary Endpoint: All-Cause Mortality
Over Length of Trial (Superiority)
Co-Primary Endpoint: Composite of All-Cause Mortality
and Repeat Hospitalization (Superiority)
Inoperable PARTNER Cohort
Primary Endpoint: All-Cause Mortality
Standard Rx
All-cause mortality (%)
TAVI
∆ at 1 yr = 20.0%
NNT = 5.0 pts
HR [95% CI] =
0.54 [0.38, 0.78]
P (log rank) < 0.0001
50.7%
30.7%
Months
Leon et al, NEJM 2010; 363:1597-1607
Numbers at Risk
TAVI
Standard Rx
179
179
138
121
122
83
67
41
26
12
PARTNER Study Design
Symptomatic Severe Aortic Stenosis
ASSESSMENT: High-Risk AVR Candidate
3,105 Total Patients Screened
Total = 1,057 patients
N = 699
High Risk
Inoperable
2 Parallel Trials:
Individually Powered
ASSESSMENT:
Yes
Transfemoral
Access
Transfemoral (TF)
1:1 Randomization
ASSESSMENT:
No
Transfemoral
Access
Transapical (TA)
1:1 Randomization
Yes
No
1:1 Randomization
N = 244
N = 248
N = 104
N = 103
N = 179
N = 179
TF TAVR
AVR
TA TAVR
AVR
TF TAVR
Standard
Therapy
VS
N = 358
VS
Primary Endpoint: All-Cause Mortality at 1 yr
(Non-inferiority)
Not In Study
VS
Primary Endpoint: All-Cause Mortality
Over Length of Trial (Superiority)
Co-Primary Endpoint: Composite of All-Cause Mortality
and Repeat Hospitalization (Superiority)
Primary Endpoint
All-cause mortality at one year
• Analysis by intent-to-treat
• Event rates by Kaplan-Meier estimates
• Crossovers permitted only when assigned
therapy unsuccessful
• All patients followed for ≥ one year
Other Important Endpoints (1)
Safety:
• Neurologic events
– Prospective: Stroke and stroke plus TIA (all neuro events)
– Retrospective: Major stroke (modified Rankin Score ≥ 2 @
≥ 30 days)
• Major vascular complications (VARC definition)
• Major bleeding (modified VARC definition)
• Repeat hospitalization
• New pacemakers and new-onset atrial fibrillation (ECG core lab)
• Procedural events (assigned therapy aborted or converted to
AVR, multiple valves, etc.)
• Surgical complications (re-op for bleeding, sternal infection, etc.)
Other Important Endpoints (2)
Clinical Effectiveness and Valve Performance:
• NYHA symptoms
• Six-minute walk tests
• Quality-of-life measures and cost-effectiveness (core lab)
• Echocardiography assessment of valve performance
(core lab)
–
–
–
–
Peak and mean gradients
Effective orifice area
Bioprosthetic valve regurgitation (esp. para-valvular)
Other: LV ejection fraction, MR, LV mass, evidence of structural
valve deterioration
Study Administration
Co-Principal Investigators
Martin B. Leon, Craig R. Smith
Columbia University Medical Center
Executive Committee
Martin B. Leon, Michael Mack,
D. Craig Miller, Jeffrey W. Moses,
Craig R. Smith, Lars G. Svensson,
E. Murat Tuzcu, John G. Webb
Data & Safety Monitoring Board
Chairman: Joseph P. Carrozza
Tufts University School of Medicine
Clinical Events Committee
Chairman: John L. Petersen
Duke University Medical Center
Echo Core Laboratory
Chairman: Pamela C. Douglas
Duke University Medical Center
Quality of Life and Cost-Effectiveness
Chairman: David J. Cohen
Mid America Heart Institute, Kansas City
Independent Biostatistical
Core Laboratory
Stuart Pocock, Duolao Wang
London School of Hygiene and
Tropical Medicine
William N. Anderson
Publications Committee
Co-Chairman: Jeffrey W. Moses
Lars G. Svensson
Sponsor
Edwards Lifesciences: Jodi J. Akin
Executive Committee
Lars Svensson Craig Miller Michael Mack Jeff Moses
Murat Tuzcu
Craig Smith
John Webb
Marty Leon
Participating Study Sites
St. Paul's Hospital
Vancouver, Canada
Univ. of Washington
Seattle, WA
Stanford
University
Palo Alto, CA
Intermountain
Medical Center
Salt Lake City, UT
Cedars-Sinai
Medical Center
Los Angeles, CA
Scripps Clinic
La Jolla, CA
Hospital Laval
Quebec City,
Canada
Toronto Gen.
Hospital
Toronto, Canada
Mayo Clinic
Rochester, MN
Evanston Hospital
Northwestern Univ.
Chicago, IL
Barnes-Jewish Hospital
St. Louis, MO
St. Luke’s Hospital
Kansas City, MO
Medical
City Dallas
Dallas, TX
n = 1,057 patients
26 investigator sites
22 USA, 3 Canada, 1 Germany
Univ. of Penn
Phila., PA
Brigham & Women’s
Mass General
Boston, MA
Columbia University
Cornell University
New York, NY
Cleveland Clinic
Cleveland, OH
Univ. of Virginia
Charlottesville, VA
Washington
Hosp. Center
Wash., DC
Emory
University
Atlanta, GA
Ochsner Foundation
New Orleans, LA
Leipzig Heart Center
Leipzig, Germany
Univ. of Miami
Miami, FL
High-Risk Enrollment by Site
Cedars-Sinai Medical Ctr
116
Los Angeles, CA
G. Fontana, R. Makkar
Columbia University
97
95
67
Cleveland, OH
L. Svensson, M. Tuzcu
Barnes-Jewish Hospital
24
Stanford University
23
Palo Alto, CA
C. Miller, A. Yeung
52
Philadelphia, PA
J. Bavaria, H. Herrmann
Cleveland Clinic Found
25
St. Louis, MO
R. Damiano, J, Lasala
Atlanta, GA
P. Block, R. Guyton
University of Pennsylvania
University of Miami
Miami, FL
W. O’Neill, D. Williams
Dallas, TX
D. Brown, T. Dewey
Emory University
40
District of Columbia
P. Corso, A. Pichard
New York City, NY
M. Leon, C. Smith
Medical City Dallas
Washington Hospital Ctr
Northwestern University
20
Chicago, IL
C. Davidson, P. McCarthy
47
St. Paul's Hospital
Vancouver, BC, Canada
A. Cheung, J. Webb
19
High-Risk Enrollment by Site
Mass General Hospital
15
Boston, MA
I. Palacios, G. Vlahakis
St. Luke’s Hospital
13
8
7
7
Seattle, WA
M. Reisman, E. Verrier
2
Ochsner Foundation
2
Intermountain Med Center
1
Salt Lake City, UT
K. Jones, B. Whisenant
6
Rochester, MN
C. Rihal, T. Sundt
Univ of Washington
Brigham & Women’s Hosp
New Orleans, LA
E. Parrino, S. Ramee
Leipzig, Germany
F. Mohr, G. Schuler
Mayo Clinic
3
Boston, MA
M. Davidson, A. Eisenhauer
La Jolla, CA
S. Brewster, P. Teirstein
Herzzentrum Leipzig
University of Virginia
Charlottesville, VA
I. Kron, S. Lim
Laval, Quebec, CA
D. Doyle, J. Rodes-Cabau
Scripps Clinic
4
Evanston, IL
J. Alexander, T. Feldman
Kansas City, MO
K. Allen, D. Cohen
Universitaire de Quebec
Northshore Univ Health Sys
Cornell University
1
New York City, NY
K. Krieger, C. Wong
5
Toronto General Hospital
Toronto, Ontario, CA
C. Feindel, E. Horlick
0
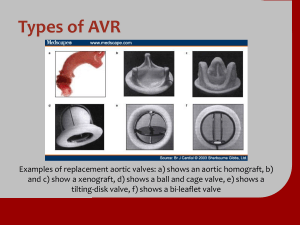
Study Devices
Edwards SAPIEN THV
23 and 26 mm valves
RetroFlex
Ascendra
22 and 24 F sheaths 24 and 26 F sheaths
TAVR
Transfemoral and Transapical
Transfemoral
Transapical
Inclusion Criteria
• Severe AS: Echo-derived AVA < 0.8 cm2 (or AVA index
< 0.5 cm2/m2) and mean AVG > 40 mm Hg or peak jet
velocity > 4.0 m/s
• Cardiac Symptoms: NYHA Functional Class ≥ II
• High surgical risk: Predicted risk of operative mortality
≥ 15% (determined by site surgeon and cardiologist);
guideline = STS score ≥ 10
Key Exclusion Criteria (1)
Anatomic:
• Bicuspid or non-calcified aortic valve
• Aortic annulus diameter (echo measurement) < 18 mm
or > 25 mm
• Aortic dissection or iliac-femoral dimensions or disease
precluding safe sheath insertion (esp. calcification)
• Severe LV dysfunction (LVEF < 20%)
• Untreated CAD requiring revascularization
• Severe AR or MR (> 3+) or prosthetic valve (any location)
Key Exclusion Criteria (2)
Clinical:
• Serum Cr > 3.0 mg/dL or dialysis dependent
• Acute MI within 1 month
• Upper GI bleed within 3 months
• CVA or TIA within 6 months
• Any cardiac procedure, other than BAV, within 1 month
or within 6 months for DES
• Hemodynamic instability (e.g. requiring inotropic support)
Statistical Analysis Plan
• Primary hypothesis is non-inferiority of test (TAVR)
vs. control (AVR) for all-cause mortality at 1 year
• Non-inferior if one-sided 95% upper confidence limit for
the treatment difference is < 7.5% (α =0.05)
• Primary Endpoint: All TF and TA patients
– Assuming true 1-year mortality 32% after AVR and 29% after TAVR
– Intended sample size = 650 patients for ≥ 85% power
• Powered Secondary Endpoint: Only TF patients
– Assuming true 1-year mortality 35% after AVR and 25% after TAVR
– Intended sample size = 450 patients for ≥ 85% power
Study Methodology
• Preliminary eligibility determined by site investigators
• Every case reviewed by web-based conference call
before enrollment
• Randomized to TF-TAVR vs. AVR, or
TA-TAVR vs. AVR, to be treated within 2 weeks
• Intent-to-treat (ITT) analysis for the primary and most
secondary endpoints; defined as the time of randomization
• As-treated (AT) analysis for some procedural endpoints
and for echo assessments; defined as the
time of procedural anesthesia induction
Study Flow
Randomized = 699 patients
TF = 492
TA = 207
Transfemoral
n = 492
Transapical
n = 207
TAVR (244)
AVR (248)
TAVR (104)
AVR (103)
30 Days (236)
30 Days (223)
30 Days (100)
30 Days (92)
Dead = 8
Withdrawal = 0
1 Year (189)
Dead = 46
Withdrawal = 1
Dead = 15
Withdrawal = 10
1 Year (168)
Dead = 47
Withdrawal = 8
Dead = 4
Withdrawal = 0
1 Year (73)
Dead = 26
Withdrawal = 0
LTFU = 1
42 Patients not treated as assigned
Dead = 7
Withdrawal = 4
1 Year (68)
Dead = 20
Withdrawal = 3
LTFU = 1
Reasons for Non-treatment
ITT = 699 patients │ AT = 657 patients
Reason
TAVR (N = 348)
AVR (N = 351)
Died before treatment - no. (%)
2 (0.6)
5 (1.4)
Deterioration before treatment - no. (%)
1 (0.3)
5 (1.4)
Refusal - no. (%)
1 (0.3)
17 (4.8)
0
11 (3.1)
4 (1.1)
38 (10.8)
Withdrawal - no. (%)
Total – no. (%)
NOTE: Time from randomization to treatment = TAVR 10.6 [SEM 0.7] days
vs. AVR 15.6 [SEM 1.1] days; P <0.001
Patient Characteristics (1)
Characteristic
TAVR (N = 348)
AVR (N = 351)
p-value
83.6 ± 6.8
84.5 ± 6.4
0.07
57.8
56.7
0.82
11.8 ± 3.3
11.7 ± 3.5
0.61
29.3 ± 16.5
29.2 ± 15.6
0.93
5.7
6.0
94.3
94.0
0.79
CAD - %
74.9
76.9
0.59
Previous MI - %
26.8
30.0
0.40
Prior CV Intervention - %
72.1
71.6
0.93
Prior CABG - %
42.6
44.2
0.70
Prior PCI - %
34.0
32.5
0.68
Prior BAV - %
13.4
10.2
0.24
29.3
27.4
0.60
Age (yr)
Male sex - %
STS Score
Logistic EuroSCORE
NYHA
II - %
III or IV - %
Cerebrovascular disease - %
Patient Characteristics (2)
Characteristic
TAVR (N = 348)
AVR (N = 351)
p-value
Peripheral vascular disease - %
43.0
41.6
0.76
COPD
Any
43.4
43.0
0.94
Oxygen dependent
9.2
7.1
0.34
Creatinine > 2mg/dL - %
11.1
7.0
0.06
Atrial fibrillation - %
40.8
42.7
0.75
Permanent pacemaker - %
20.0
21.9
0.58
Pulmonary hypertension - %
42.4
36.4
0.15
Frailty - %
15.6
17.6
0.58
Porcelain aorta - %
0.6
1.1
0.69
Chest wall radiation - %
0.9
0.9
1.00
Liver disease - %
2.0
2.6
0.80
Baseline Echocardiography
Echo Findings
TAVR (N = 348)
AVR (N = 351)
p-value
AVA - cm2
0.7 ± 0.2
0.6 ± 0.2
0.13
AVG - mm Hg
42.7 ± 14.6
43.5 ± 14.3
0.45
Mean LVEF - %
52.5 ± 13.5
53.3 ± 12.8
0.45
19.8
21.3
0.63
Moderate or severe MR - %
Procedural Outcomes - TAVR vs AVR
AVR
TAVR
Anesthesia time - min
330
Anesthesia time - min
236
Total procedure time - min
230
Total procedure time - min
133
3 failed access
2 new TEE
Aborted procedure
- no. findings
(%)
2 died
0
Reoperation for bleeding - no. (%)
Aborted procedure - no. (%)
7 (2.0)
12 (3.4)
Reoperation for bleeding - no. (%)
2 (0.6)
Intra-procedural death - no. (%)
1 (0.3)
Intra-procedural death - no. (%)
3 (0.9)
Aortic perforation - no. (%)
1 (0.3)
Aortic perforation - no. (%)
0
Aortic dissection - no. (%)
3 (0.9)
Aortic dissection - no. (%)
3 (0.9)
Median ICU stay (days)
5.0
Median ICU stay (days)
*Converted to transapical TAVR due to porcelain aorta
3.0
Procedural Outcomes - TAVR vs AVR
AVR
Sternal wound infection - no. (%)
Total cross clamp time - min
TAVR
7 (2.0)
74
5 valve embolization
Pump time
- min
3 annulus
size on TEE 105
1 large sigmoid septum
5 converted to AVR
2 valve-in-valve
2 not treated
Access site infection - no. (%)
Fluoroscopy time - min
7 (2.0)
31
Converted to AVR - no. (%)
9 (2.6)
Multiple (≥2) valves - no. (%)
7 (2.0)
Valve embolization - no. (%)
9 (2.6)
*Converted to transapical TAVR due to porcelain aorta
Primary Endpoint:
All-Cause Mortality at 1 Year
0.5
HR [95% CI] =
0.93 [0.71, 1.22]
P (log rank) = 0.62
TAVR
AVR
0.4
26.8
0.3
0.2
24.2
0.1
0
0
6
No. at Risk
12
18
24
Months
TAVR
348
298
260
147
67
AVR
351
252
236
139
65
Primary Endpoint:
All-Cause Mortality at 1 Year
TAVR
AVR
(N = 348)
(N = 351)
24.2%
Difference
Upper 1-sided
95% CI
26.8%
-2.6%
Noninferiority
P value
3.0%
= 0.001
Zone of non-inferiority pre-specified
margin = 7.5%
Non-inferior
-3.0
-2.0
-1.0
0.0
1.0
2.0
3.0
4.0
5.0
6.0
7.0
8.0 %
Upper one-sided 95% CI
Primary Non-Inferiority Endpoint Met
All-Cause Mortality
Transfemoral (N=492)
HR [95% CI] =
0.83 [0.60, 1.15]
P (log rank) = 0.25
26.4
22.2
No. at Risk
Months
TAVR
244
215
188
119
59
AVR
248
180
168
109
56
Powered Secondary Endpoint (ITT):
TF All-Cause Mortality at 1 Year
TAVR
AVR
(N = 248)
(N = 244)
22.2%
Difference
-4.2%
Noninferiority
P value
2.3%
= 0.002
Upper 1-sided
95% CI
26.4%
Zone of non-inferiority pre-specified
margin = 7.5%
Non-inferior
-5.0
-4.0
-3.0
-2.0
-1.0
0.0
1.0
2.0
3.0
4.0
5.0
6.0
7.0
Upper one-sided 95% CI
Secondary TF Non-Inferiority Endpoint Met
8.0 %
All-Cause Mortality
Transapical (N=207)
HR [95% CI] =
1.22 [0.75, 1.98]
P (log rank) = 0.41
29.0
27.9
No. at Risk
Months
TAVR
104
83
72
28
8
AVR
103
72
68
30
9
Surgical AVR Outcomes
• Using an established predictive risk model (STS), the
expected (“E”) 30-day mortality after AVR was 11.8%.
• The observed (“O”) 30-day mortality in the as-treated AVR
control group was 8.0%.
• O:E = 0.68 indicates better than predicted surgical
outcomes in the control AVR patients.
• There were no significant site or surgeon differences.
All-Cause Mortality at 30 Days and 1 Year
ITT and ATT by Subgroup
All-Cause Mortality at 30 Days
All Patients
TF Patients
TA Patients
no. of patients ( %)
no. of patients ( %)
no. of patients ( %)
TAVR
AVR
p-value
TAVR
AVR
p-value
TAVR
AVR
p-value
ITT
12 (3.4)
22 (6.5)
0.07
8 (3.3)
15 (6.2)
0.13
4 (3.8)
7 (7.0)
0.32
AT
18 (5.2)
25 (8.0)
0.15
9 (3.7)
18 (8.2)
0.05
9 (8.7)
7 (7.6)
0.79
All-Cause Mortality at 1 Year
All Patients
TF Patients
TA Patients
no. of patients ( %)
no. of patients ( %)
no. of patients ( %)
TAVR
AVR
p-value
TAVR
AVR
p-value
TAVR
AVR
p-value
ITT
84 (24.2) 89 (26.8)
0.44
54 (22.2) 62 (26.4)
0.29
30 (29.0) 27 (27.9)
0.85
AT
81 (23.7) 78 (25.2)
0.64
51 (21.3) 55 (25.2)
0.33
30 (29.1) 23 (25.3)
0.55
Clinical Outcomes at 30 Days and 1 Year
All Patients (N=699)
30 Days
Outcome
TAVR
(N = 348)
1 Year
AVR
TAVR
p-value
(N = 351)
(N = 348)
AVR
p-value
(N = 351)
All mortality – no. (%)
12 (3.4)
22 (6.5)
0.07
84 (24.2)
89 (26.8)
0.44
Cardiac mortality – no. (%)
11 (3.2)
10 (3.0)
0.90
47 (14.3)
40 (13.0)
0.63
Rehospitalization – no. (%)
15 (4.4)
12 (3.7)
0.64
58 (18.2)
45 (15.5)
0.38
Death or rehosp – no. (%)
25 (7.2)
33 (9.7)
0.24
120 (34.6)
119 (35.9)
0.73
0
2 (0.6)
0.16
1 (0.4)
2 (0.6)
0.69
10 (2.9)
10 (3.0)
0.95
18 (5.4)
20 (6.5)
0.56
MI – no. (%)
Acute kidney inj* – no. (%)
* Renal replacement therapy
Clinical Outcomes at 30 Days and 1 Year
All Patients (N=699)
30 Days
Outcome
TAVR
(N = 348)
1 Year
AVR
TAVR
p-value
(N = 351)
(N = 348)
AVR
p-value
(N = 351)
Vascular complications
All – no. (%)
59 (17.0)
13 (3.8)
<0.01
62 (18.0)
16 (4.8)
<0.01
Major – no. (%)
38 (11.0)
11 (3.2)
<0.01
39 (11.3)
12 (3.5)
<0.01
Major bleeding – no. (%)
32 (9.3)
67 (19.5)
<0.01
49 (14.7)
85 (25.7)
<0.01
Endocarditis – no. (%)
0 (0.0)
1 (0.3)
0.32
2 (0.6)
3 (1.0)
0.63
New AF – no. (%)
30 (8.6)
56 (16.0)
< 0.01
42 (12.1)
60 (17.1)
0.07
New PM – no. (%)
13 (3.8)
12 (3.6)
0.89
19 (5.7)
16 (5.0)
0.68
Neurological Events at 30 Days and 1 Year
All Patients (N=699)
30 Days
Outcome
TAVR
(N = 348)
1 Year
AVR
p-value TAVR
(N = 351)
(N = 348)
AVR
p-value
(N = 351)
All Stroke or TIA – no. (%)
19 (5.5)
8 (2.4)
0.04
27 (8.3)
13 (4.3)
0.04
TIA – no. (%)
3 (0.9)
1 (0.3)
0.33
7 (2.3)
4 (1.5)
0.47
All Stroke – no. (%)
16 (4.6)
8 (2.4)
0.12
20 (6.0)
10 (3.2)
0.08
Major Stroke – no. (%)
13 (3.8)
7 (2.1)
0.20
17 (5.1)
8 (2.4)
0.07
Minor Stroke – no. (%)
3 (0.9)
1 (0.3)
0.34
3 (0.9)
2 (0.7)
0.84
Death/maj stroke – no. (%)
24 (6.9)
28 (8.2)
0.52
92 (26.5)
93 (28.0)
0.68
All-Cause Mortality or Stroke
All Patients (N=699)
HR [95% CI] =
0.95 [0.73, 1.23]
P (log rank) = 0.70
28.0
26.5
No. at Risk
Months
TAVR
348
289
252
143
65
AVR
351
247
232
138
63
NYHA Functional Class
P < 0.001
P = 0.05
P = 0.75
Baseline
30 Days
6 Months
1 Year
Patients Surviving, %
P = 1.00
I
II
III
IV
Six-Minute Walk Test
All Patients (N=699)
Median Distance, meters
P = 0.73
P = 0.002
P = 0.33
P = 0.76
Subgroup Analyses of Treatment Effect
All-Cause Mortality at 1 Year
TAVR (%)
n=348
AVR (%)
n=351
Overall
24.1
25.4
0.95(0.73-1.23)
Age
<85
>85
21.6
27.0
24.9
26.1
0.87(0.60-1.27)
1.03(0.72-1.47)
0.52
Sex
Male
Female
28.4
18.4
24.2
27.2
1.17(0.84-1.63)
1.17(0.84-1.63)
0.045
BMI
<26
>26
27.3
21.0
27.4
23.8
0.68(0.44-1.04)
0.99(0.71-1.40)
0.66
STS score
<11
>11
19.9
28.1
21.7
29.3
0.88(0.59-1.31)
0.92(0.61-1.38)
0.87
LV ejection
fraction
<55
>55
26.2
22.4
27.7
22.1
0.96(0.69-1.34)
1.01(0.68-1.50)
0.80
Subgroup
RR
(95% CI)
0.5
1
TAVR better
RR
(95% CI)
2
AVR better
P-value for
interaction
Subgroup Analyses of Treatment Effect
All-Cause Mortality at 1 Year
Subgroup
Pulmonary
hypertension
No
Yes
Mitral
regurgitation
No
Yes
Prior CABG
No
Yes
Peripheral
vasc disease
No
Yes
Cohort
TA
TF
TAVR (%)
n=348
AVR (%)
n=351
21.3
27.4
RR
(95% CI)
RR
(95% CI)
P-value for
interaction
21.7
29.9
0.98(0.64-1.50)
0.92(0.66-1.28)
0.80
24.6
24.2
22.1
35.2
1.11(0.82-1.52)
0.69(0.41-1.17)
0.12
22.2
25.9
30.7
19.1
0.72(0.52-1.01)
1.35(0.88-2.08)
0.02
22.4
26.4
25.1
25.4
0.89(0.63-1.27)
1.04(0.70-1.54)
0.57
28.8
22.1
26.2
25.0
1.10(0.71-1.71)
0.89(0.64-1.22)
0.43
0.5
1
TAVR better
2
AVR better
Echo Findings
Aortic Valve Gradients
80
Peak Gradient - AVR
Peak Gradient - TAVR
70
Mean and Peak Gradient
As-Treated Trial Arms (mmHg)
Mean Gradient - AVR
Mean Gradient - TAVR
60
50
40
30
20
10
0
Baseline
TAVR
n = 327
AVR
n = 301
30 Days
TAVR
n = 287
AVR
n = 231
6 Months
TAVR
n = 246
AVR
n = 170
1 Year
TAVR
n = 227
AVR
n = 159
Echo Findings
Hemodynamic Assessments
30 Days
1 Year
TAVR
AVR
p-value
TAVR
AVR
p-value
AVG – mmHg
9.9 ± 4.8
10.8 ± 5.0
0.04
10.2 ± 4.3
11.5 ± 5.4
0.008
AVA - cm2
1.7 ± 0.5
1.5 ± 0.4
0.001
1.6 ± 0.5
1.4 ± 0.5
0.002
Finding
LVEF - %
55.5 ± 11.4 56.0 ± 11.4
0.63
56.6 ± 10.5 57.1 ± 10.3
0.64
Paravalvular Aortic Regurgitation
P < 0.001
P < 0.001
30 Days
6 Months
1 Year
Patients, %
P < 0.001
None
Trace
Mild
Moderate
Severe
Study Limitations
• 8% of the control (AVR) group withdrew or refused assigned
therapy
• 5% of patients randomized to TAVR did not receive
assigned therapy (procedure aborted or converted to AVR)
• Significantly longer interval between randomization and
treatment in controls (AVR)
• An early version large TAVR delivery system was used
• Most sites had no previous TAVR experience - learning
curve impact inherent in TAVR, but not in AVR
• Insufficient statistical power to compare TA to either AVR
or TF
• Long-term follow-up not available to assess TAVR durability
Conclusions (1)
• The primary endpoint of the trial was met:
– In patients with aortic stenosis at high risk for operation,
TAVR was non-inferior to AVR for all-cause mortality at
1 year (24.2% vs. 26.8%, p=0.001 for non inferiority)
– Transfemoral TAVR subgroup was also non-inferior to
AVR (p=0.002 for non-inferiority)
• Death at 30 days was lower than expected in both
arms of the trial:
– TAVR mortality (3.4%) was the lowest reported in any
series, despite an early generation device and limited
previous operator experience
– AVR mortality (6.5%) was lower than the expected
operative mortality (11.8%)
Conclusions (2)
• Both TAVR and AVR were associated with important
but different peri-procedural hazards:
– Major strokes at 30 days (3.8 vs. 2.1%, p=0.20) and
one year (5.1% vs. 2.4%, p=0.07) and major vascular
complications were more frequent with TAVR
(11.0% vs. 3.2%, p<0.001)
– Major bleeding (9.3% vs. 19.5%, p<0.001) and new
onset atrial fibrillation (8.6% vs. 16.0%, p<0.001) were
more frequent with AVR
• TAVR and AVR are both acceptable therapies in these
high-risk patients; differing peri-procedural hazards should
influence case-based decision-making
Conclusions (3)
• Symptom improvement (NYHA class and 6-min walk
distance) favored TAVR at 30 days and was similar
to AVR at one year
• Echo findings indicate:
– Small hemodynamic benefit with TAVR vs. AVR at 1 year
(mean gradient p=0.008, AVA p=0.002)
– Increased para-valvular regurgitation associated with
TAVR (p<0.001)
• Preliminary subgroup analyses should be interpreted
cautiously:
– Possible TAVR benefit in women and patients without
prior CABG
Implications
• A multidisciplinary valve team approach benefits patients
and is recommended for all future valve centers.
• TAVR is already the standard-of-care for inoperable
patients with severe aortic stenosis. These results
indicate that TAVR is an acceptable alternative to AVR
in selected high-risk operable patients.
• Future randomized studies should focus on lower risk
patients who are candidates for operation.
Back-up Slides
Per Cent (%)
PARTNER Comparison of Outcomes
High-Risk vs. Inoperable Patients
11.0
5.0
Neurological Events and Mortality
at 30 Days and 1 Year (as treated)
TAVR
Complication
AVR
With
Without
With
Without
31
313
16
297
2 (6.5)
16 (5.1)
1 (6.3)
24 (8.1)
10 (32.3)
71 (22.8)
3 (18.8)
75 (25.6)
18
326
11
302
Died ≤ 30 days – no. (%)
2 (11.1)
16 (4.9)
1 (9.1)
24 (8.0)
Died ≤ 1 year – no. (%)
9 (50.0)
72 (22.2)
3 (27.3)
75 (25.1)
Stroke or TIA
All Patients – no.
Died ≤ 30 days – no. (%)
Died ≤ 1 year – no. (%)
Major Stroke
All Patients – no.
Vascular/Bleeding Events and Mortality
at 30 Days and 1 Year (as treated)
TAVR
Complication
AVR
With
Without
With
Without
38
306
11
302
Died ≤ 30 days – no. (%)
6 (15.8)
12 (3.9)
2 (19.2)
23 (7.6)
Died ≤ 1 year – no. (%)
14 (37.3)
67 (22.0)
5 (49.5)
73 (24.4)
52
292
88
225
2 (3.8)
16 (5.5)
15 (17.1)
10 (4.5)
16 (31.1)
65 (22.3)
36 (41.3)
42 (18.9)
Major Vascular
All Patients – no.
Major Bleeding
All Patients – no.
Died ≤ 30 days – no. (%)
Died ≤ 1 year – no. (%)
All-Cause Mortality (As Treated TAVR Trial Arm)
Stratified by Major Stroke
1
No Event
0.9
Event
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0
0
6
12
Months
18
24
All-Cause Mortality (As Treated TAVR Trial Arm)
Stratified by Major Vascular Event
1
No Event
0.9
Event
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0
0
6
12
Months
18
24
All-Cause Mortality (As Treated TAVR Trial Arm)
Stratified by Major Bleed
1
No Event
0.9
Event
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0
0
6
12
Months
18
24
All-Cause Mortality (As Treated AVR Trial Arm)
Stratified by Major Stroke
1
No Event
0.9
Event
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0
0
6
12
Months
18
24
All-Cause Mortality (As Treated AVR Trial Arm)
Stratified by Major Bleed
1
No Event
0.9
Event
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0
0
6
12
Months
18
24
All-Cause Mortality (As Treated AVR Trial Arm)
Stratified by New Atrial fibrillation
1
No Event
0.9
Event
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0
0
6
12
Months
18
24
All-Cause Mortality (As Treated)
Pooled Implant Approaches (N= 657)
HR [95% CI] =
1.02 [0.77, 1.36]
P (log rank) = 0.88
25.2
23.7
No. at Risk
Months
TAVR
344
291
258
139
64
AVR
313
243
226
128
60
Primary Endpoint: (As Treated)
All-Cause Mortality at 1 Year
TAVR
AVR
(N = 344)
(N = 313)
23.6%
Difference
Upper 1-sided
95% CI
25.2%
-1.6%
Noninferiority
P value
4.0%
= 0.004
Zone of non-inferiority pre-specified
margin = 7.5%
Non-inferior
-3.0
-2.0
-1.0
0.0
1.0
2.0
3.0
4.0
5.0
6.0
7.0
8.0 %
Upper one-sided 95% CI
Primary Non-Inferiority Endpoint Met
All-Cause Mortality (As Treated)
Transfemoral (N=461)
HR [95% CI] =
0.90 [0.64, 1.26]
P (log rank) = 0.53
25.2
21.3
No. at Risk
Months
TAVR
240
209
186
112
58
AVR
221
172
161
100
53
Powered Secondary Endpoint (AT):
TF All-Cause Mortality at 1 Year
TAVR
AVR
(N =240 )
(N = 221)
21.3%
Difference
-3.9%
Noninferiority
P value
2.6%
= 0.002
Upper 1-sided
95% CI
25.2%
Zone of non-inferiority pre-specified
margin = 7.5%
Non-inferior
-5.0
-4.0
-3.0
-2.0
-1.0
0.0
1.0
2.0
3.0
4.0
5.0
6.0
7.0
Upper one-sided 95% CI
Secondary TF Non-Inferiority Endpoint Met
8.0 %
All-Cause Mortality (As Treated)
Transapical (N=196)
HR [95% CI] =
1.36 [0.82, 2.26]
P (log rank) = 0.23
29.1
25.3
No. at Risk
Months
TAVR
104
82
72
27
6
AVR
92
71
65
28
7
All-Cause Mortality
Stratified by ITT Trial Arm and Patient Gender
1
0.9
0.8
TAVR Female
0.7
AVR Female
0.6
0.5
0.4
0.3
0.2
0.1
0
0
6
12
Months
18
24
All-Cause Mortality
Stratified by ITT Trial Arm and Prior CABG
1
0.9
0.8
AVR: CABG No
0.7
0.6
AVR: CABG Yes
0.5
0.4
0.3
0.2
0.1
0
0
6
12
Months
18
24
All-Cause Mortality
Stratified by ITT Trial Arm and Prior CABG
1
0.9
0.8
TAVR: CABG No
0.7
0.6
AVR: CABG No
0.5
0.4
0.3
0.2
0.1
0
0
6
12
Months
18
24
All-Cause Mortality
Stratified by ITT trial arm and Moderate/Severe MR
1
0.9
0.8
TAVR MR No
0.7
TAVR MR Yes
P = 0.027
(log rank)
AVR MR No
0.6
AVR MR Yes
0.5
0.4
0.3
0.2
0.1
0
0
6
12
Months
18
24
Echo Findings
Valvular Regurgitation
30 Days
1 Year
Finding – no. (%)
TAVR
AVR
p-value
TAVR
AVR
p-value
Transvalv. Regurg.
Mod/Severe
3 (1.0)
2 (0.9)
<.0001
2 (0.9)
0 (0.0)
<.0001
Paravalv. Regurg.
Mod/Severe
35 (12.2)
2 (0.9)
<.0001
15 (6.8)
3 (1.9)
<.0001
All Regurg.
Mod/Severe
21 (7.7)
4 (1.7)
<0.001
12 (5.5)
3 (1.9)
<0.001
Echo Findings
Paravalvular Regurgitation
30 Days
Finding – no. (%)
TAVR
AVR
1 Year
p-value
None
65 (22.6)
168 (73.7) <.0001
Trace/Mild
187 (65.2)
58 (25.4)
Mod/Severe
35 (12.2)
2 (0.9)
TAVR
73 (32.9)
<.0001 134 (60.4)
<.0001
15 (6.8)
AVR
p-value
123 (77.8) <.0001
32 (20.3)
<.0001
3 (1.9)
<.0001
Aortic Valve Area
As Treated Trial Arms
2.00
1.75
Valve Area, cm2
1.50
1.25
1.00
0.75
0.50
AVR
0.25
TAVR
0.00
Baseline
TAVR
n = 319
AVR
n = 297
30 Day
TAVR
n = 279
AVR
n = 228
6 Month
TAVR
n = 235
AVR
n = 165
1 Year
TAVR
n = 219
AVR
n = 155