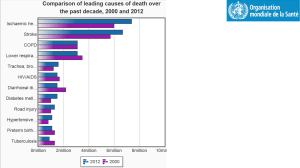
March 20-21 – Valve Disease in Older Adults (Part 2)
advertisement
Key Questions • Can AVR be performed? • Should AVR be performed? Can AVR Be Performed? • Identify Obstacles to Success – Technical: Prior Cardiac Surgery (patent LIMA), Prior XRT, PVD, etc – Organ Morbidity: Renal, Pulmonary, Neuro/Cognitive – Patient Frailty – Institutional: Presence of Multidisciplinary Care Team with Excellent Outcomes – Estimate Risks: STS, NYS, Euroscore, etc – Family/Social Support Should AVR Be Performed? • Is the AS severe? • Is there a clear indication for AVR (ie symptoms or CHF)? • Are there other causes for symptoms or for CHF? • Will success impact overall functional status and quality of life? If the Answer is Yes, Don’t Wait for Higher Risk! Case 1 • • • • • • • • 95 y/o woman History of hypertension and aortic stenosis NYHA class IV symptoms Multiple admissions for heart failure in the past year Echo with critical AS and decreased LV function Most recent admission, treated with diuretics and discharged home due to advanced age Readmitted within one week with CHF and BNP >5000 Renal function: BUN/Cr 24/0.9 Case 1: Echocardiogram • EF – 25% • Severe AS – Peak Velocity - 4.2 m/s – Mean Gradient - 45 mmHg – Valve Area - 0.6 cm2 • Moderate Pulm HTN ~ 50 mmHg Case 1: Cardiac Catheterization • • • • RA – 30 mmHg PA – 70/34/48 mmHg PCW – 35 mmHg C.O. – 2.0 L/min, C.I. – 1.2 L/min/m2 • Aortic Valve – Peak Gradient – 71 mmHg – Mean Gradient – 45 mmHg – Valve Area – 0.25 cm2 • Severe CAD Case 1: High Mortality Risk! • STS Risk Calculator – CABG/AVR – Mortality Risk – 33.8% – AVR Alone – Mortality Risk – 27.9% • Logistic EuroSCORE – CABG/AVR – Mortality Risk – 78.8% Case 1 What Would You Do? 1.BAV 2.TAVI 3.Surgical AVR – surgeons refused 4.Palliative Care Patient is now 100 years old and still lives independently. There have been no admissions for CHF in the last 5 years Case 2 • 80 y/o man with history of CABG 18 years ago presents with progressive dyspnea on exertion • Asymptomatic with negative stress tests until 3 years ago when his walking became limited by spinal stenosis • 1 year ago, his wife noted that he was SOB walking short distances indoors Case 2: Additional History • Progressive short-term memory loss • Multiple TIA’s over the past 2 years • CNS Imaging shows multiple old fronto-parietal infarcts • No significant extra-cranial vascular disease Case 2: Echocardiogram • • • • Severe AS Peak velocity 4.3 AVA 0.7 cm2 EF normal Case 2: Cardiac Catheterization • • • • • RA 7 mmHg PA 32/7 mmHg PCWP 12 mmHg PA Sat 68% Mean AV gradient 40 mmHg • AVA 0.68 cm2 • Coronary angiography: • Patent LIMA to LAD • Patent SVG to OM • Occluded SVG to RCA • Severe native 3VD Case 2 Risk Calculator • • STS 2.9% mortality, 20% morbidity Euroscore 26.8% mortality What Would You Do? 1.BAV 2.TAVI – not a PARTNER candidate 3.Surgical AVR – surgeons refused 4.Palliative Care Case 2: Balloon Aortic Valvuloplasty • Post BAV: – gradient 8 mmHg – AVA 1.4 cm2 Case 2 • Wife reported resolution of dyspnea for approximately 2 months • 2 months later, repeat Echo showed peak velocity 3.9 mmHg, AVA 0.9 cm2 • Underwent successful transfemoral TAVI with 26mm Edwards-Sapien Valve Case 2: Post-op Course • Persistent somnolence, but no new infarct by CNS imaging • Discharged after 5 days • 2 years later – Wife reports dyspnea resolved – Severe dementia Mitral Regurgitation in Older Adults • Moderate to severe MR is present in 10% of adults over 75. • Degenerative • Functional –Ischemic –Dilated cardiomyopathy Goals of Treatment • Degenerative MR: – Eliminate symptoms – Maintain normal survival • Functional MR: – Improve symptoms – Improve QOL – Decrease hospitalizations for CHF Degenerative MR • Primary disease of the valve leaflets and chordea – Myxomatous – Diffuse calcific degeneration • Regurgitation results from either excess leaflet motion or restriction of leaflets and annular contraction • LV function is initially normal Degenerative (myxomatous) MR O'Gara, P. et al. J Am Coll Cardiol Img 2008;1:221-237 Degenerative MR Surgical Indications • Severe MR prior to consequence (IIa) • Severe MR with consequence – – – – – Symptoms (I) LV Dysfunction (I) (30< EF < 60) Atrial Fibrillation (IIa) Pulmonary Hypertension (IIa) Severe MR with EF < 30 with structural mitral disease and high likelihood of repair (IIa) with NYHA III-IV Degenerative MR Surgical Indications • Severe MR prior to consequence (IIa) • Severe MR with consequence – – – – – Symptoms (I) LV Dysfunction (I) (30< EF < 60) Atrial Fibrillation (IIa) Pulmonary Hypertension (IIa) Severe MR with EF < 30 with structural mitral disease and high likelihood of repair (IIa) with NYHA III-IV Survival of operative survivors after MR surgery stratified by age at surgery Detaint D et al. Circulation 2006;114:265-272 Trends in operative mortality for MR surgery Contemporary Results in Age > 80 • 30 day mortality 5% • 3 month mortality 13% • Complications • Stroke: 5% repair, 7% replacement • Prolonged ventilation 50% • Acute renal failure 10% In patients over 80 7.7% stroke rate for MVR Detaint D et al. Circulation 2006;114:265-272 DiGregorio, Annals of Thoracic Surgery, 2004 Nioga L, Euro J CT Surg, 39 (2011) 875-880 Functional MR • Primary disease of LV: Local-ischemic MR Global-dilated cardiomyopathy • MR results from restricted valve leaflet motion • LV function is initially depressed Mechanisms of Ischemic Mitral Regurgitation Papillary muscle traction Increased tethering Decreased closing force Bulging MR Annular dilatation Degree of MR predicts Survival in CHF (Ischemic and Dilated Cardiomyopathy) Functional MR Current Treatment Options • Medical • RAAS inhibition (ACE inhibition, ARB) • Beta-Blockers • Relieve ischemia • Cardiac resynchronization therapy • Surgical/Transcatheter techniques - Reduction annuloplasty - Alfieri, Chordal, LV remodeling, LV restraint, posterior leaflet extension, mitral valve replacement - Catheter-based annuloplasty and restraint devices Surgical Outcomes • Ischemic MR – in general – Operative mortality 5-10% overall – ~50% five year survival with surgery – Symptomatic benefit in many – Recurrence rate problematic – Effect on mortality unknown • Ischemic MR – paucity of data in elderly – Less than 50% 1 year survival in octogenarians1 – Effect on symptoms and quality of life unknown 1Nioga L, Euro J CT Surg, 39 (2011) 875-880 Decision Not To Operate In Symptomatic Severe MR n = 546 49% of patients in the Euro Heart Survey on valvular heart disease with symptomatic severe MR were not operated on. Mirabel et al. Eur Heart Journal 2007;28:1358-1365 Percutaneous Mitral Valve Repair: Mitral Clip MR High Risk Registry: Mitral Clip • Mean age 76 • 60% functional MR • Ejection fraction: 54% • STS Score 14% • In hospital mortality = 7.2% • No strokes CHF hospitalizations reduced by 26% Whitlow, P. L. et al. J Am Coll Cardiol 2012;59:130-139 Older Adult with MR Case • 75 y/o man with CAD s/p CABG 14 years ago after inferior MI • Post CABG noted to have progressively decreased LV function, MR, and CHF • 3 years ago CRT-D with marked improvement in symptoms • 6 months of progressive fatigue, dyspnea on exertion, orthopnea, edema, and ascites despite maximal medical therapy • Rapid loss of independence, yet still working Physical Exam • VS: BP 90/60, P 70 • Ill appearing elderly man • JVP elevated to angle of the jaw with prominent V wave • Bilateral pleural effusions • PMI in anterior axillary line • Loud systolic murmur at the apex • Pulsatile liver and ascites • Pedal edema to the knees Studies • Labs: BUN 60/Cr 1.9 • EKG: BiV paced • CXR: enlarged heart and bilateral pleural effusions Cardiac Catheterization • Coronary angiography: Patent LIMALAD, Patent SVG OM1-OM2, Occluded SVG-PDA and Occluded RCA • LVEF 35%, Moderate MR • Hemodynamics: RA 12, PA 45/26/32, PCWP 20, CI 2.2, PVR 5 • With exercise: PA 60/36, mean PCWP 28, V wave to 45 Referred for Surgery • Tissue MVR and Tricuspid Valve Repair • 1 month later, exercise tolerance had improved and orthopnea and edema had resolved • Lasix dose decreased from 80 mg bid to 80 mg daily • BUN and Cr normalized 3 Year Follow-up • Patient had to cancel his last visit because he was too busy running a retailing business. • Patient works daily. • Patient lives independently. • Symptom free. Conclusions • Valvular disease is an important cause of morbidity and mortality in older adults • Treatment should focus on symptom relief and maintenance of functionality • Improvement in surgical outcomes and emerging percutaneous therapies make treatment available to more high risk patients • Optimizing the timing and selection of the appropriate therapies is evolving AS in older adults Reasons for Treatment Allocation Wenaweser, P. et al. J Am Coll Cardiol 2011;58:2151-2162