Health-Related Quality of Life After Transcatheter vs.
Surgical Aortic Valve Replacement in High-Risk
Patients With Severe Aortic Stenosis
Results From The PARTNER Trial (Cohort A)
David J. Cohen, M.D., M.Sc.
On behalf of The PARTNER Investigators
Saint Luke’s Mid-America Heart Institute
University of Missouri-Kansas City
Kansas City, Missouri
Harvard Clinical Research Institute
Harvard Medical School
Boston, MA
TCT 2011 | San Francisco | November 7, 2011
Disclosures
The PARTNER Trial was funded by a research grant
from Edwards Lifesciences, Inc.
Background
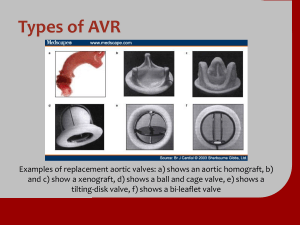
• Transcatheter aortic valve replacement (TAVR) has been
developed as a less invasive alternative to surgical valve
replacement for high-risk patients with severe aortic stenosis
• In PARTNER Cohort A, TAVR was found to be non-inferior to
surgical AVR for the primary endpoint of 1-year mortality among
patients at high surgical risk
• There were differences in procedure-related complications and
valve performance at 1 year – with some endpoints favoring
TAVR and others favoring surgical AVR
• The overall impact of these alternative treatments on healthrelated quality of life from the patient’s perspective has not yet
been reported
3
Study Objectives
1. Compare health-related quality of life outcomes
among patients with severe aortic stenosis and
high surgical risk treated with either TAVR or
surgical AVR
2. Determine whether the QOL benefits of TAVR vs. AVR
vary over time
3. Examine whether the QOL benefits of TAVR vs.
AVR differ according to access site or other patient
characteristics
4
PARTNER Study Design
Symptomatic Severe Aortic Stenosis
ASSESSMENT: High-Risk AVR Candidate
3,105 Total Patients Screened
Total = 1,057 patients
N = 699
High-Risk
Inoperable
2 Parallel Trials:
Individually Powered
ASSESSMENT:
Yes
Transfemoral
Access
Transfemoral (TF)
1:1 Randomization
ASSESSMENT:
No
Transfemoral
Access
Transapical (TA)
1:1 Randomization
Yes
No
1:1 Randomization
N = 244
N = 248
N = 104
N = 103
N = 179
N = 179
TF TAVR
AVR
TA TAVR
AVR
TF TAVR
Standard
Therapy
VS
N = 358
VS
Primary Endpoint: All-Cause Mortality at 1 yr
(Non-inferiority)
Not In Study
VS
Primary Endpoint: All-Cause Mortality
Over Length of Trial (Superiority)
Co-Primary Endpoint: Composite of All-Cause Mortality
and Repeat Hospitalization (Superiority)
Methods: Quality of Life
Instrument
Kansas City
Cardiomyopathy
Questionnaire (KCCQ)
6
Description/Role
• Heart failure-specific QOL
• Domains: symptoms, physical limitations,
quality of life, social limitations
• Scores: 0-100 (higher = better)
Methods: Quality of Life
Instrument
7
Description/Role
Kansas City
Cardiomyopathy
Questionnaire (KCCQ)
• Heart failure-specific QOL
• Domains: symptoms, physical limitations,
quality of life, social limitations
• Scores: 0-100 (higher = better)
SF-12
• General physical and mental health
• Scores standardized such that mean = 50,
standard deviation = 10 (higher = better)
Methods: Quality of Life
Instrument
8
Description/Role
Kansas City
Cardiomyopathy
Questionnaire (KCCQ)
• Heart failure-specific QOL
• Domains: symptoms, physical limitations,
quality of life, social limitations
• Scores: 0-100 (higher = better)
SF-12
• General physical and mental health
• Scores standardized such that mean = 50,
standard deviation = 10 (higher = better)
EQ-5D (EuroQOL)
• Generic instrument for assessment of utilities
and QALYs
• Scores: 0-1 (0 = death; 1 = perfect health)
Assessments performed by self-administered
questionnaires at baseline and at 1, 6, and 12 months
KCCQ: Development and Validation
• 23 items that measure 5 clinically relevant domains of
health status from the patient’s perspective
– Symptoms
– Quality of life
– Self-efficacy
Physical limitation
Social limitation
• Extensive validation and reliability testing
• Individual scales combined into a global summary scale
(KCCQ Overall Summary)
– Independently predictive of mortality and cost among patients
with HF
9
Green CP, et al. JACC. 2000;35:1245-55.
Soto G, et al. Circulation. 2004;110:546-51.
KCCQ: Interpretation
Change in KCCQ-Overall Summary Score
• 546 outpts with HF
• KCCQ assessed at
baseline and 5 weeks
• Extent of deterioration
or improvement
assessed by physician
based on sx and exam
and correlated with
KCCQ-Overall
Summary
Clinically Important Change
Large Medium Small
Deterioration
10
• Small = 5 points
Small
Medium
Large
No
• Moderate = 10 points
Change
Improvement• Large = 20 points
Am Heart J. 2005;150:707-15.
Analytic Approach
Analytic Population
• All patients with baseline QOL assessment, analyzed by
assigned treatment (ITT)
Primary QOL Endpoint
• KCCQ Overall Summary Score
• All other QOL scales considered secondary endpoints
11
Statistical Methods
• Scores at each time point compared within treatment group
using paired t-tests
• Scores between groups compared using random effect
growth curve models, adjusted for baseline, age, sex, and
access site (TA vs. TF)
• Analytic plan specified that separate analyses would be
performed for the TA and TF groups in case of a significant
interaction between treatment effect and access site
12
Baseline Characteristics
TAVR
AVR
(n = 328)
(n = 300)
Age (yrs)
84 7
84 6
Male gender
57.6%
56.7%
11.8 3.4
11.5 3.2
Prior MI
27.4%
27.7%
Prior CABG
42.7%
45.0%
Cerebrovascular Dz
26.8%
24.7%
COPD (O2 dependent)
9.1%
7.3%
Frailty
15.4%
17.1%
STS risk score
13
P = NS for all comparisons
Results
• There were highly significant interactions between
treatment effect and access site for the primary endpoint
(P = 0.001) and multiple secondary endpoints (P < 0.01) –
mainly at the 1 month and 6 month time points
• Therefore, all QOL analyses were performed separately for
TF and TA subgroups
14
KCCQ Overall Summary (Primary Endpoint)
TF Subgroup
Treatment Difference (TAVR - AVR)
30
20
10
0
-10
-20
D = 9.9
P < 0.001
D = -0.5
P = NS
D = -1.2
P = NS
1 month
6 months
12 months
-30
15
P-values are for mean treatment effect of TAVR vs. AVR
KCCQ Subscales
TF Subgroup
Physical Limitations
Symptom Score
30
20
10
0
-10
-20
D = 10.9
P = 0.001
D = -0.5
P = NS
D = 2.3
P = NS
Treatment Difference (TAVR - AVR)
Treatment Difference (TAVR - AVR)
30
-30
20
10
0
-10
-20
6 months
12 months
6 months
12 months
D = 10.6
P = 0.006
D = -2.9
P = NS
D = -2.9
P = NS
1 month
6 months
12 months
Social Limitations
Quality of Life
30
20
10
0
-10
D = 9.8
P < 0.001
D = 0.3
P = NS
D = -1.9
P = NS
6 months
12 months
Treatment Difference (TAVR - AVR)
Treatment Difference (TAVR - AVR)
D = -1.1
P = NS
1 month
30
20
10
0
-10
-20
-30
-30
16
D = -2.1
P = NS
-30
1 month
-20
D = 6.6
P = 0.006
1 month
Generic QOL and Utilities
TF Subgroup
SF-12 Mental
10.0
7.5
7.5
5.0
2.5
0.0
-2.5
-5.0
-7.5
D = 2.0
P = 0.04
D = -0.4
P = NS
D = -0.9
P = NS
Treatment Difference (TAVR - AVR)
Treatment Difference (TAVR - AVR)
SF-12 Physical
10.0
5.0
2.5
0.0
-2.5
-5.0
-7.5
D = 5.4
P < 0.001
D = 0.4
P = NS
-10.0
-10.0
1 month
6 months
1 month
12 months
EQ-5D Utilities
Treatment Difference (TAVR - AVR)
0.20
0.15
0.10
0.05
0.00
-0.05
-0.10
-0.15
D = 0.061
P = 0.008
D = 0.012
P = NS
D = 0.028
P = NS
6 months
12 months
-0.20
1 month
17
D = 1.2
P = NS
6 months
12 months
KCCQ Overall Summary (Primary Endpoint)
TA Subgroup
Treatment Difference (TAVR -AVR)
30
20
10
0
-10
-20
D = -5.8
P = NS
D = -7.9
P = 0.04
1 month
6 months
D = 0.8
P = NS
-30
18
12 months
P-values are for mean treatment effect of TAVR vs. AVR
KCCQ Subscales
TA Subgroup
Physical Limitations
Symptom Score
30
20
10
0
-10
-20
D = -5.8
P = NS
D = -9.6
P = 0.04
D = -4.1
P = NS
Treatment Difference (TAVR -AVR)
Treatment Difference (TAVR -AVR)
30
20
10
0
-10
-20
1 month
6 months
1 month
12 months
Quality of Life
6 months
12 months
Social Limitations
20
10
0
-10
D = -4.7
P = NS
D = -8.4
P = 0.06
D = 4.8
P = NS
1 month
6 months
12 months
-30
Treatment Difference (TAVR -AVR)
Treatment Difference (TAVR -AVR)
D = -2.3
P = NS
30
30
19
D = -13.2
P < 0.001
-30
-30
-20
D = -5.1
P = NS
20
10
0
-10
-20
D = -5.8
P = NS
D = -3.8
P = NS
D = 6.1
P = NS
-30
1 month
6 months
12 months
Generic QOL and Utilities
TA Subgroup
SF-12 Mental
10.0
7.5
7.5
5.0
D = 0.3
P = NS
D = 0.2
P = NS
D = -3.3
P = 0.05
2.5
0.0
-2.5
-5.0
-7.5
Treatment Difference (TAVR -AVR)
Treatment Difference (TAVR -AVR)
SF-12 Physical
10.0
5.0
D = -4.3
P = 0.02
D = -2.5
P = NS
D = -2.5
P = NS
1 month
6 months
12 months
2.5
0.0
-2.5
-5.0
-7.5
-10.0
1 month
6 months
-10.0
12 months
EQ-5D Utilities
Treatment Difference (TAVR -AVR)
0.20
0.15
0.10
D = -0.057
P = NS
D = -0.065
P = 0.05
D = -0.051
P = NS
1 month
6 months
12 months
0.05
0.00
-0.05
-0.10
-0.15
-0.20
20
KCCQ-Summary: Substantial Improvement*
TF Subgroup
P = NS
P = NS
P = 0.008
21
* Improvement ≥ 20 points vs. baseline among patients with available QOL data
KCCQ-Summary: Substantial Improvement*
TA Subgroup
P = NS at all timepoints
22
* Improvement ≥ 20 points vs. baseline among patients with available QOL data
Sensitivity Analyses
Results similar when:
• Analysis restricted to patients who underwent attempted
valve treatment (“As treated” cohort; n = 607)
• “Worst case” values (at the 90th percentile) were imputed
to all patients with missing data
• Outcomes analyzed categorically according to either
significant improvement (≥ 10-point change from baseline)
or a multilevel ordinal outcome
23
Summary-1
• Among patients with severe AS who were at high risk for
standard valve replacement, both surgical and
transcatheter AVR resulted in substantial improvement in
disease-specific and generic HRQOL over 1 year follow-up
– KCCQ Summary Scale ~ 25-30 points (MCID = 5)
– SF-12 Physical ~ 6 points (MCID = 2)
– SF-12 Mental ~ 5 points (MCID = 2)
24
Summary-2
• Although the extent of improvement at 1 year was similar
with TAVR and AVR, there were important differences in
the rate and extent of recovery at the earlier time points
• For patients eligible for the TF approach, TAVR resulted in
substantial QOL benefits compared with AVR at 1 month
with similar QOL at later time points
• For patients eligible only for the TA approach, there was
no benefit of TAVR over AVR at any time point, and QOL
tended to be better with AVR both at 1 and 6 months
25
Conclusions
• Taken together with previous data, these findings
demonstrate that for patients suitable for a TF approach,
TAVR provides meaningful clinical benefits compared with
surgical AVR from the patient’s perspective
• The lack of benefit (and suggestion of worse QOL) among
patients ineligible for the TF approach suggests that the
TA approach may not be preferable to surgical AVR in
such patients
• Whether further experience and refinements in the TA
approach can overcome these limitations should be the
subject of future investigation
26