APPLIED ANATOMY OF LOWER LIMB BLOOD VESSELS
advertisement

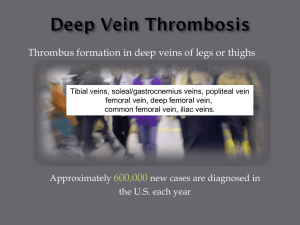
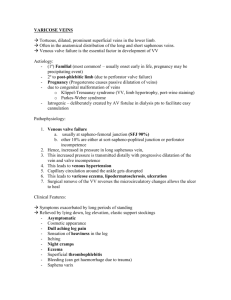
APPLIED ANATOMY OF LOWER LIMB BLOOD VESSELS LEARNING OBJECTIVES At the end of the lecture the student should be able to: • Revise main arterial and venous supply of lower limb • Know injuries or disease associated with vessels of lower limb ARTERIAL SUPPLY • FEMORAL ARTERY - Continuation of external iliac artery below the inguinal ligament - Ends at adductor hiatus by becoming popliteal artery - Gives of profunda femoris as its major branch • POPLITEAL ARTERY - Gives genicular branches to supply knee joint - Terminates in three branches (a) Anterior tibial (b) Posterior tibial (c) Peroneal artery ANGIOGRAM VENOUS SUPPLY • LONG SAPHENOUS VEIN – Continuation of dorsal venous arch – Passes anterior to medial malleolus – Passes through saphenous opening of fascia lata to drain into femoral vein – Tributaries: • Superficial epigastric • Superficial external pudendal • Superficial circumflex iliac vein • Communicating branches to small saphenous and deep veins • SHORT SAPHENOUS VEIN – Arises from lateral part of dorsal venous arch – Passes posterior to lateral malleolus – Asends up back of leg – Drains into popliteal vein – LONG SAPHENOUS VEIN IS USED AS DONOR VEIN IN CORONARY BYPASS GRAFTING. • • PERFORATING VEINS – Connects superficial great and small saphenous veins to deep veins – Possess valves allowing flow of blood from superficial to deep veins only VENOGRAM DEEP VEIN THROMBOSIS • • Coagulation of blood in deep veins, resulting in thrombus formation Causes impairment of blood flow through deep veins • Virchow's triad: Venous thrombosis occurs via three mechanisms: 1. Decreased flow rate of blood 2. Damage to blood vessel wall 3. Increased tendency of blood to clot PREDISPOSING FACTORS: • INCRESED THROMBOTIC TENDENCY 1.Deficiency of protein C, protein S, anti thrombin III. 2. Malignancy. 3. Dehydration • STASIS 1. Bedridden patients 2. Cardiac failure 3. Prolong surgery 4. Prolong flight • DAMAGE TO VESSEL WALL 1. Trauma PRESENTATION: 1. Silent 2. Pain in calf muscle 3. Swelling of calf 4. Redness of skin and tenderness 5. Increased temperature of skin EXAMINATION: Unreliable for excluding diagnoses of DVT INSPECTION: – Swollen leg – Redness of skin PALPATION: – Tenderness of calf muscles – Warm calves – Homan’s test INVESTIGATION: BLOOD TEST: • D- dimers IMAGING: • Doppler ultrasound • Duplex ultrasound • Venography TREATMENT: • Complete bed rest • Graduated compression stockings • Anti coagulation (Injection Heparin or oral warfarin) COMPLICATIONS: • Pulmonary embolism • Post DVT limb • Varicose veins ARTERIO-VENOUS FISTULA • Abnormal connection between an artery and a vein. CAUSES • Congenital • Surgically created for hemodialysis • Acquired due to pathologic process, such as trauma or erosion of an arterial aneurysm. THROMBOEMBOLISM • • • • • Peripheral vascular disease Usually affects lower leg Arteriosclerosis Stenosis of blood Leading to thrombus and embolus formation CAUSES: • Diabetes • Hypertension • Smoking • Increases cholesterol • Age • Decreased activity PRESENTATION • Intermittent claudication – pain on walking, relived by rest • Acute presentation – Pale – Pulseless – – – – • Painful Paralysed Paraesthetic Perishing cold INVESTIGATION – Ankle brachial pressure index – Angiography – Doppler ultrasound TREATMENT • Conservative – Lifestyle changes – Stop smoking – Healthy diet • Surgical – Angioplasty – Bypass graft – Amputation extreme cases TRAUMA MECHANISM: • Blunt injury • Penetrating injury • Blast injury • Iatrogenic injury DIAGNOSIS: Clinical • Pulseless, cold , pale limb • Expanding haematoma • Palpable thrill • Audible bruit • Active bleeding IMAGING: 1. Duplex 2. Ultrasonography 3. Contrast enhance CT 4. Digital subtractions angiography MANAGEMENT: 1. Haemorrhage control 2. Vascular repair