PN 3/Cardiac/Vascular/Peripheral vascular disturbances part one
advertisement

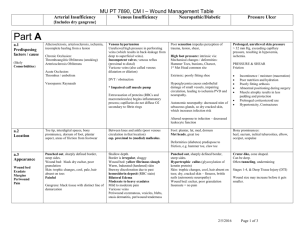
Disorders In Tissue Perfusion Disorders Of The Peripheral Vascular System Liz Mathewson Summary • • • • • • • normal A&P of peripheral vasc. system risk factors and causes prevention and health teaching assessments nsg. diagnosis medical/surgical/pharmatherapeutic nursing measures Categories of Disorders • Obstruction: thrombus, embolus, lymphedema • Inflammation: phlebitis, thrombophlebitis • Degeneration: arteriosclerosis, atherosclerosis, aneurysm, varicose veins, stasis ulcer • Unknown causes: Buerger’s disease, Raynauds Disease Pharmacology Classifications: • anticoagulants (and their reversal agents) • antilipidemics (antihyperlipidemic) • platelet inhibitors • thrombolytics • peripheral vasodilators Obstructive Disease • Can affect both venous and arterial circulation as well as lymph system To the Brain To the liver To the stomach To the Kidneys Iliac Artery Femoral Artery Arterial Obstructive Disease • (degenerative condition leading to obstructive condition) • Arteriosclerosis: “hardening of the arteries” – muscle fibers and the endothelial lining of the walls of small arteries and arterioles become thickened Obstructive Arterial Disease Atherosclerosis: affects the intima of the large and medium-sized arteries – caused by an accumulation of lipids, calcium, blood components, carbohydrates, and fibrous tissue on the intima layer = plaque Direct effects: Indirect effects: Atherosclerosis • Risk factors: – – – – – – diet high blood pressure diabetes stress sedentary lifestyle smoking - age - gender - family hx Assessment • Health history and clinical manifestations • Pain (where) • Skin appearance and temperature – Rubor – cyanosis – brittle nails, – dry scaling skin, atrophy, decrease hair growth, ulceration Signs and Symptoms • Occur when vessel is 60% occluded • Early include pain, changed appearance, or changed sensation • Pain or “intermittent claudication” • Pain on exertion or pain at rest? • Chronic = collateral circulation Assessment • Pulses – present or absent, volume, quality, symmetry “pedal pulses present bilaterally” – Posterior tibial; dorsalis pedis; popliteal; Assessment • Mental status • Edema (Pitting or non-pitting) • Risk factors: – controllable (modifiable) – not controllable (non-modifiable) Arterial Assessment Tools • • • • • • • Doppler U/S flow Studies Ankle blood pressures Exersize tests CT CT Angiography MRI Angiography Progression of Disease • Decreased oxygen leads to ischemia • Ischemia leads to infarction • Infarction leads to necrosis • Ischemia Infarction Necrosis Arterial ulcers Ischemia Infarction Necrosis Venous Ulcers (characteristics) Nsg. Diagnosis • Alteration in peripheral tissue perfusion related to compromised circulation • Pain related to impaired ability of peripheral vessels to supply tissues with oxygen • Risk for impaired skin integrity related to compromised circulation • Knowledge deficit regarding self-care activities Nursing Diagnosis • Alteration in peripheral tissue perfusion related to compromised circulation – Goal: Increase arterial blood supply to extremities Medical Management • Medical: modification of risk factors; a controlled exercise program to increase circulation; and medication Surgical Management • Surgical: Inflow procedures and outflow procedures – Bypass (artificial graft/insitu graft) – Endarterectomy Grafts Endarterectomy Post-op Care • Maintaining circulation – how? • Assessment: pulses, colour, temperature, capillary refill, sensory and motor functions • use doppler (at PRCH, use doppler on Dr.Thompson pts.) • Complications: decreased urinary output, CVP, mental status, pulse rate and volume = fluid imbalance Post-op Care • Bleeding, hematoma • Edema • Infection • Discharge planning Upper extremity Obstruction • Arm fatigue and pain with exercise and inability to hold or grasp objects. • Avoid venopuncture, injury, using tape, taking BP, protect from cold. Assess frequently • May need bypass Arterial Embolism • Usually originate in the chamber of the heart as a result of atrial fibrillation, or CHF, infective endocarditis or MI. • Carried to left side of heart and into arterial system • May be caused by catheters, stents, intraaortic balloon pump. • Trauma, crush injury, penetrating wound Signs and Symptoms • 6 “P”s – – – – – – pain pallor pulselessness paresthesia paralysis poikothermia X Treatment • • • • FAST to prevent tissue infarction heparin surgery (embolectomy) ? Thrombolytic therapy if no contraindications Venous Obstruction • • • • Venous Thrombosis Deep Vein Thrombosis Thrombophlebitis Phlebothrombosis • * not identical disease processes but for clinical purposes used interchangeably Pathophysiology Stasis of Blood Virchow’s Triad Altered Blood Coagulation Vessel Wall Injury Venous Stasis • Reduced Blood Flow due to : – heart failure or shock – dilated veins due to medications – decreased skeletal muscle contractions due to paralysis, anesthesia, and bed rest Vessel Wall Injury • Damage to the Intima Due to: – direct trauma (fractures, dislocations) – diseases of the veins, (infection/inflammation) – chemical irritation (IV meds and solutions Increased blood coaguability • Due to: – abrupt withdrawal of anticoagulants – oral contraceptives – blood dyscrasias (abnormalities) Clinical Manifestations Often Non-Specific: • inflammation or redness along a superficial vein • limb pain, feeling of heaviness • functional impairment • ankle engorgement, edema • unilateral increase in leg circumference • increased warmth to touch of leg/foot • tenderness to touch, rosy colour Thrombus to Embolus • Platelets attach to vein wall with a tail-like appendage containing fibrin, RBC, WBC • grows in direction of blood flow • elevation in venous pressure (sudden movement, increased muscle movement) cause fragment to break off and travel Deep Vein Thrombosis • Sign and symptoms are non specific, sometimes PE is the first sign • deep veins have thinner walls and less muscle mass in the media than superficial veins • run parallel to arteries and have the names • have valves as do the superficial veins Deep Vein Obstruction • Creates swelling and edema in extremity because the outflow of venous blood is inhibited • limb may be warm and superficial veins appear more prominent • tenderness • Howman’s sign Superficial thrombosis • Pain or tenderness, redness and warmth in involved area • embolus rare as these thrombi usually dissolve spontaneously • treated with bed rest at home, elevation of leg, analgesics, and sometimes anti inflammatory Medical Management for DVT • Medication • Surgery: only if anticoagulant or thrombolytic therapy is contraindicated, the danger of PE is extreme, and the venous drainage is so severely compromised that permanent damage to the extremity will result. Nursing Interventions • • • • • Assessing and monitoring meds observing for complications providing comfort applying elastic stockings positioning pt and encouraging exercise Venous Ulcers (characteristics) Anticoagulants • Heparin: two types – fractionated, low-molecular - weight heparin – fractionated heparin is given IV 5 to 7 days and coumadin (orally) started concurrently – sometimes given prophylactically SC – regulated by monitoring the partial thromboplastin time, the INR, and the platelet count Heparin • • • • LMWH, more $ SC longer 1/2 life does are adjusted by wt, does not bind with plasma proteins • fewer bleeding complications • can be given to pregnant women Heparin Nursing responsibilities: • monitor blood work • observe for bleeding • to reverse heparin = protamine sulfate • to reverse warfarin = vit K • drug interactions Thrombolytic Agents • i.e. Streptokinase • lyses thrombi and emboli • observe for bleeding • contraindicated: recent bleed, trauma, Lymphedema • Primary or secondary • results from an obstruction of lymph vessels and an accumulation of lymph • noticed in dependent position • starts of as soft, pitting and treatable • progresses to firm, non pitting and does not respond to treatment Lymphedema • Obstruction may be in the node or vessel • often seen in the arm following a mastectomy • treatment may include bedrest, elevation, active and passive exercise, custom fitted stockings • Pharm: diuretic, antibiotics, • Surgery: excision of tissue and fascia Venous insufficiency • Chronic venous insufficiency: • results from venous valve obstruction and a result of venous hypertension • wall of the vein become distended resulting in reflux • post thrombotic syndrome • edema altered pigmentation, pain and stasis dermatitis Leg ulcers • 75% of leg ulcers from CVI • inflamed necrotic tissue sloughs off • arterial insufficiency ulcers account for approx.. 20% the remaining 5% from SSE, burns and other factors Arterial Ulcers • Small circular, deep ulcerations on the tips of toes or in the web spaces between toes • medial side of hallux or lateral 5th toe • may result in gangrene of toe • gangrene usually left alone Venous Ulcers • Ulcers are usually in the area of the medial or lateral malleolus and are large, superficial, and highly exudative. • See pictures on pg 710 of Brunner Nursing Diagnosis • Impairment of skin integrity related to vascular insufficiency • Impaired physical mobility related to activity restrictions of he therapeutic regimen and plan • Altered nutrition, less than body requirements, related to increased need for nutrients that promote wound healing Goals • Demonstrates restored skin integrity • Increases physical mobility • Attains adequate nutrition • How???? Patient Teaching • • • • • • • venus ulceration from CVI antigravity activities elevate legs during the day sleep with foot of bed elevated no prolonged standing no cross legs, no trauma foot care, stockings Varicose veins • Abnormally dilated, tortuous superficial veins caused by incompetent venous valves • predisposing factors – hereditary – occupation/lifestyle – gender (female) May be primary or secondary Varicose Veins • May result in chronic venous insufficiency: edema, pain, pigmentation and ulceration • susceptibility to injury and infection is increased • treatment: surgical, sclerotherapy, stockings Degeneration of the Vascular System Aneurysm • A localized sac or dilation involving an artery formed at a weak point in a vessel wall • classified by its shape or form • most common saccular or fusiform • saccular projects from one side of the vessel only • fusiform is when entire arterial segment dilates Aneurysm • Small aneurysm caused by localized infection is called mycotic aneurysms • most common is the abdominal aortic (AAA) • serious because they can rupture leading to hemorrhage and death Thoracic Aneurysm • Most common site for a dissecting aneurysm • common in men between age 40-70 • 1/3 of pts with thoracic aneurysms die from rupture Signs and symptoms • Depends on how rapid the aneurysm dilates and how the pulsating mass affects surrounding intrathoracic structures. • Usually pain is the prominent symptom • shortness of breath, dysphasia, loss of voice • hoarseness, stridor • dx by chest xray, ct, mri S & S of AAA • • • • • • • • Common in whites, 4:1 men to women most occur below the renal arteries c/o “heart beating in stomach” abd mass “blue toe” syndrome as a result of embolus 80% can be palpated impending rupture include sever pain 50 to 75% mortality rate for ruptured AAA AAA • • • • surgical repair put in a graft may be bifurcated better if it is below renal arteries Dissecting Aorta • A tear develops in the intima or the media degenerates, resulting in dissection • onset sudden, severe persistent pain, tearing feeling, pain in shoulders, chest, epigastric or abd. Raynauds Disease Buerger’s Disease