Urinary tract Infections
advertisement

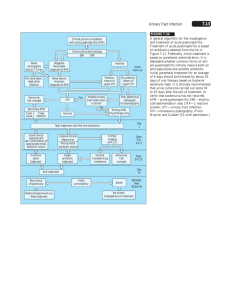
Urinary tract Infections: -At least 20% of all women experience an incident of Urinary tract infection (UTI) by the age of 30 years, and over 50% have one or more lifetime UTIs. One in ten women experience frequent recurrent infections for at least some period. -An estimated 3 million office visits for this infection take place each year in the United States. N -Nosocomial UTI accounts for about 40% of all infections acquired in acute care facilities. -From 25 to 50% of nursing home patients have bacteriuria at any time. Urinary tract infection UTI is more common in Women due to: 1-Anatomy of female Urinary tracts: Short urethra, and proximity of the urethral opening to the anus. 2-Lack of antibacterial prostatic secretions. 3- Bacterial invasion by sexual intercourse. N -UTI could be established in different sexes due to the following risk factors: 1-Poor personal hygiene. 2-Insertion of contaminated Catheter. -Physical and chemical barriers that protect human urinary tracts from infection: 1-The frequent flushing action of urine. 2- Urine acidity ( pH from 4.5 to 8 ). 3- The prostatic secretions (lysozyme and IgA). Definitions: UTI could occur at any site of urinary tract; including Kidney, bladder, and in men, the prostate. Upper UTI: Kidney infection. Lower UTI: 1-Urinary bladder infection. 2-Urethra infections are classified as sexually transmitted diseases. Pyelonephritis: (Pyelum: Renal pelvis, Nephro: kidney) : is an ascending urinary tract infection that has reached the pelvis of the kidney. N Pyelonephritis: 1-Acute non-obstructive pyelonephritis: Acute inflammation of renal pelvis and medullary tissue due to bacterial invasion. 2-Complicated pyelonephritis: -Underlying structural or functional abnormalities of Kidney. -Could be associated with obstruction of renal pelvis. -Tissue dysfunction or Renal abscess. N -Urinary tract Reinfection: Recurrent infection when a previously isolated organism is reintroduced into the urinary tract from the colonizing gut or genital flora. -Relapse: Recurrent infection with bacteria that persist within the urinary tract due to indwelling urologic devices; such as urethral catheter or nephrostomy tube. n -Biofilm: is a layer of bacteria, their extracellular substances, and urine components (protein, calcium, Mg+2) contaminating drainage bag grow along the exterior or internal catheter surface. -Biofilm is strongly associated with establishment of complicated pyelonephritis. Pathogenesis: Source of infecting organisms: 1-The colonizing flora from the periurethral area or, in woman, the vagina. 2-Bacteria originate from the normal gut flora. 3-Contaminated urologic devices. Pathogenesis: A-Lower urinary tract infection (Uropathogenic Escherichia coli). N B-Adherence of E.coli to mannosylated glycoprotein that line the bladder mucosa due to mannose sensitive fimbria FimH. C-Ascend to the kidney due to: 1-Reflux of infected urine up the ureter. -Short intravesical ureter. -Incompetent ureteral sphincters. 2-PMN cell influx up the ureter. D- Bacterial entry through the papillae into the renal parenchyma. N E-Adhesion of microbes to interstitial tissue surrounding the tubules and renal cells in kidney medulla due to P Fimbria (K polysaccharide) – glycosphingolipid disaccharide receptor interaction. N F-Damage of interstitial tissue due to: 1-Cytokines production, cellular infiltration; inflammation (Toxic O2 radicals, and lysozymes ). 2-Activation of clotting factors; ischemia. 3-Microbial virulence: Hemolysin, and urease activity. G-Tubulointerstitial nephritis. Pathogenesis: N Types of Tubulointerstitial Nephritis: 1-Acute TIN: - Inflammatory infiltrate and edema affecting the renal interstitial tissue that often develops during days to months. - Over 95% of cases result from infection or an allergic drug reaction. - Renal abscess could be illustrated microscopically in some cases (Rare). - Renal abscess (uncommon) mainly caused by bacteremic spread of infection from other body site. N -Interstitial renal abscesses : Necrosis contains neutrophils, and central germ colonies (hematoxylinophils). -Tubules are damaged and may contain neutrophil casts. -In the early stages, the glomerulus and vessels are normal. Causes of Pyelonephritis and TIN: 1- Escherichia coli. The most common cause of UTI ( 85-90%). 2- Staphylococcus saprophyticus. It is considered as a second causative agent of UTI (5-20%). 3- Other genera of Enterobacteriaceae : Klebsiella, Enterobacter, Proteus, and Serratia. 4- Pseudomonas aeruginosa ( Hospital-acquired infection). 5- Enterococcus faecalis ( Hospital-acquired infection). n 2-Chronic TIN: -Gradual interstitial infiltration and fibrosis, tubular atrophy and dysfunction, and a gradual deterioration of renal tissue, usually over years. -Glomerular involvement is much more common in chronic nephritis than acute type. -Causes: immunologically mediated disorders, infections, and drug interaction. Glomerulonephritis : GN: GN: is the inflammation of the Glomeruli of the nephron. Types: 1-Infective: Source of infection: Hematogenous dissemination. Pathologic feature: One or more renal cortical abscesses. Pathogenesis: Insoluble antigen Inflammatory destruction of the Glomeruli. trapped in the glomerulus Antibodies attack the structural components of the kidney and antigen. N 2-Non-Infective GN: Soluble antigen in blood stream; Antibodies react with soluble antigen; Serum sickness disease; Precipitation of complexes in glomeruli; inflammatory destruction. Types of soluble antigen: 1- Exogenous: A-Drugs, toxoid, or serum. B-Infectious agent antigen: - Post-Streptococcal glomerulonephritis: Anti-Streptolysin-O complexes. n Other infections: Bacterial: Staphylococci, Streptococcus pneumoniae, Klebsella, Yersinia enterocolitica, Treponema, Salmonella. Parasites: Malaria, Schistosoma, and Toxoplasma. Viral : Hepatitis, and E.B.V. Fungal: Candidiasis. 2- Endogenous: Self antigen. Differential Diagnosis: Urine analysis: 1- Physical properties: -Appearance: turbidity or milky: pus in urine -Color: 1-white color: Pus in urine: Pyuria :infection 2-Red color: RBCs in urine: (Hematuria): kidney stones, infections , or tumors? N 2-Chemical properties: -Glucose in urine: (Glycosuria) : : considered as a risk factor for bacterial infection; bacteria utilize glucose during binary fission. -Nitrite in urine: (Nitrituria): : indicates the presence of Coliform bacteria in urine. Note: Enterobacteriaceae species reduce Nitrate to Nitrite. n Protein in urine: Proteinuria: - In Pyelonephritis, and lower UTI: Proteinuria (trace from pus or bacterial origin) and Pyuria. - In interstitial nephritis and Glomerulonephritis: Proteinuria , Hematuria, lower number of Pus in urine. 3-Microscopic properties: -WBCs: Normal : 2-3 /HPF. -RBCs: Normal : 3-4 cells/HPF. - Casts: A- Granular , fatty cast, Hemoglobin, and RBCs cast: Acute Glomerulonephritis due to immune system response. C- WBCs cast: acute pyelonephritis, acute tubulointerstitial nephritis due to infection. Infective TIN and Infective or Non-infective GN: n Infective TIN Immune-GN Infective -GN +++++ + Low number. Urine Culture Positive or negative negative Nitrite in urine Positive or negative negative Usually negative negative +++++ ++++ Pyuria Hematuria Hemoglobinuria Proteinuria Casts Trace from pus and bacteria or tubular origin. WBCs Cast (Neutrophil cast( +++++ (kidney origin) Hemoglobin or RBCs Casts.