Diseases of the Gallbladder and Biliary Tract
advertisement
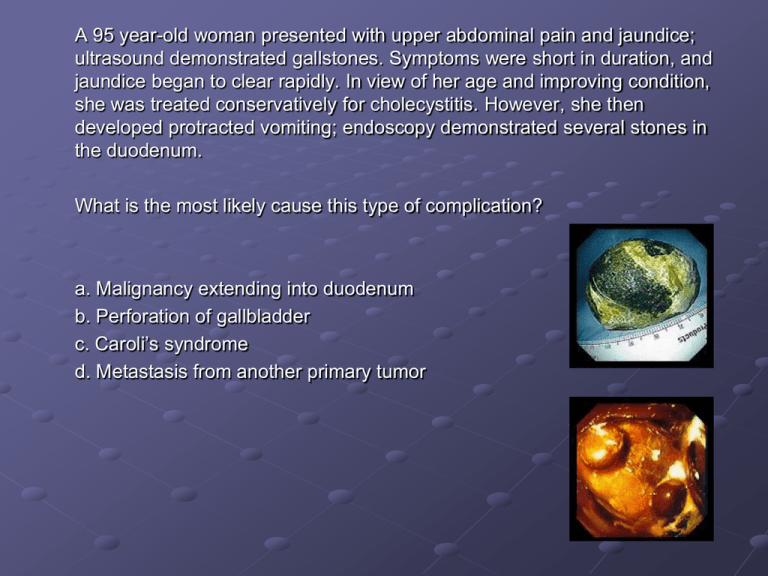
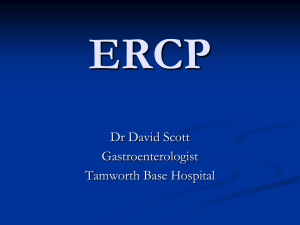
A 95 year-old woman presented with upper abdominal pain and jaundice; ultrasound demonstrated gallstones. Symptoms were short in duration, and jaundice began to clear rapidly. In view of her age and improving condition, she was treated conservatively for cholecystitis. However, she then developed protracted vomiting; endoscopy demonstrated several stones in the duodenum. What is the most likely cause this type of complication? a. Malignancy extending into duodenum b. Perforation of gallbladder c. Caroli’s syndrome d. Metastasis from another primary tumor Diseases of the Gallbladder and Biliary Tract Driss Raissi, MD New York State University Downstate Lecture Series Normal Biliary Physiology Liver produces 500-1500 mL of bile/day Major physiologic role of biliary tract and GB is to concentrate bile and conduct it in well-timed aliquots to the intestine. In the intestine: bile acids participate in normal fat digestion Cholesterol and other endogenous/exogenous cmpds in bile excreted in feces. Biliary Physiology Complex fluid secreted by hepatocytes Passes through hepatic bile ducts into common hepatic duct Tonic contraction of sphincter of Oddi during fasting diverts ~1/2 of bile through the cystic duct into the GB – stored and concentrated. CCK – released after food ingestion GB contracts, sphincter of Oddi relaxes Allows delivery of timed bolus of bile into intestine. Bile acids – detergent molecules Have both fat and water soluble moieties Convey phospholipids and cholesterol from liver to intestine Cholesterol undergoes fecal excretion Enterohepatic circulation Bile acids solubilize dietary fat and promote its digestion and absorption Enterohepatic circulation: Bile acids efficiently reabsorbed by SI mucosa (terminal ileum) recycled to liver for re-excretion Cholelithiasis Normal Gallbladder Velvety green mucosa Thin wall Tall columnar cells lining mucosal folds (right) Submucosa and muscularis at the left. Cholelithiasis Gallstones: MCC biliary tract disease in US (2035% by age 75) 2 types: Cholesterol (75%) Pigment Calcium bilirubinate and other calcium salts Cholesterol Stones Cholesterol: Insoluble in water Normally carried in bile solubilized by bile acids and phospholipids In most individuals, bile contains > cholesterol than can be maintained in stable solution “supersaturated” with cholesterol microscopic cholesterol crystals form Interplay of nucleation (mucus, stasis) and “anti-nucleating” (apolipoprotein A-I) factors determine whether cholesterol gall stones form Gradual deposition of cholesterol layers macroscopic cholesterol stones Cholesterol Stones Gallbladder: key to stone formation Area of bile stasis slow crystal growth Provides mucus or other material to act as a nidus for initiating cholesterol crystal. Mexican Americans and several American Indian tribes, particularly the Pima Indians in the Southwest high prevalence rates of cholesterol gallstones ↓bile acid secretion is believed to be the common denominator in these ethnic groups Pigment stones Pathophysiology less well understood production of bilirubin conjugates (hemolytic states) biliary Ca2+ and CO32Cirrhosis Bacterial deconjugation of bilirubin to less soluble form Predisposing Factors Factors that increase biliary cholesterol saturation: Estrogens Multiparity OCP’s Obesity Rapid weight loss Terminal ileal disease (decreases bile acid pool) Factors that increase bile stasis: Bile duct strictures Parenteral hyperalimentation Fasting Choledochal cysts Pregnancy – (GB hypomotility) Clinical Manifestations Most are asymptomatic Duct obstruction - underlying cause of all manifestations Cystic duct obstruction distends GB biliary pain Superimposed inflamm/ifx acute cholecystitis Common duct obstruction pain, jaundice, ifx(cholangitis), pancreatitis, and/or hepatic damage 2° to biliary cirrhosis Asymptomatic Gallstones 60-80% patients with gallstones in US Over 20-year period: 18% of these develop biliary pain 3% require cholecystectomy Prophylactic cholecystectomy considered in 3 high-risk groups: 1. Diabetics – 10-15% greater mortality 2. Calcified (porcelain) GB – Associated w/CA of GB 3. Sickle cell anemia – hepatic crisis difficult to differentiate vs. acute cholecystitis Porcelain Gallbladder Treatment of Asx Gallstones Chenodeoxycholic acid or Ursodeoxycholic acid Dissolution of cholesterol stones Expectant management then cholecystectomy if symptomatic disease develops = more cost effective Alternatives: Dissove cholesterol stones: Instill Methyl-tert-butyl-ether or ethyl propionate into GB Fragment stones: extracorporeal shock wave lithotripsy Extracorporeal Shockwave Lithotripsy Chronic Cholecystitis and Biliary Pain Nonacute sx. caused by presence of gallstones Biliary Pain (misnamed biliary colic) GB from symptomatic patients may be grossly normal Mild histologic inflammation with fibrosis and thickening often from previous attacks of acute cholecystitis. Symptoms: From contraction of GB during transient obstruction of cystic duct by gallstones. Steady ache in epigastrium or RUQ comes on quickly plateau over a few minutes subsides gradually over 30 min-several hours Referred pain at tip of scapula or right shoulder N/V can accompany. (no fever, leukocytosis, or palpable mass) Attacks occur at variable intervals (days – years) Nonspecific symptoms: Dyspepsia, fatty food intolerance, bloating and flatulence, heartburn, belching Diagnosis Ultrasonography Sensitivity and specificity >95% Oral cholecystograpy 90% sensitivity, 75% specificity Reserved for ensuring cystic duct patency in pts whom dissolution therapy or extracorporeal shock wave lithotripsy is planned Treatment Laparoscopic cholecystectomy Treatment of choice for recurrent biliary pain May need preoperative endoscopic or radiologic examination of CBD for concomitant choledocholithiasis Open cholecystectomy Mortality rate <0.5% Might be required if difficulties during procedure i.e. adhesions, obesity NSAIDS Several reorts and trials suggest that use during biliary pain provides adequate pain relief and ↓ progression to acute cholecystitis Acute Cholecystitis Acute Cholecystitis Acute right subcostal pain and tenderness from obstruction of cystic duct Distension, inflammation, and 2° ifx of GB Acalculous cholecystitis (5%) Triad - Prolonged fasting, immobility, hemodynamic instability Critically ill patients (burns, trauma, sepsis) Parenteral hyperalimentation Acute Cholecystitis Epigastric or RUQ pain Gradually in severity and localizes to GB area Unlike biliary pain, does not spontaneously resolve Low grade fever, anorexia, n/v, right subcostal tenderness (+)Murphy’s sign subhepatic tenderness and inspiratory arrest during deep breath Tender enlarged gallbladder (1/3) Mild jaundice (20%) – concomitant CBD stones or BD edema Murphy’s Sign Complications Onset of fever, shaking chills, leukocytosis, abdominal pain or tenderness, or persistent severe symptoms = progression of disease and development of complications Emphysematous cholecystitis Diabetics with bacterial gas present in GB lumen and wall Empyema of gallbladder Gangrene Perforation Mirizzi’s syndrome Profound jaundice in which extrinsic CBD compression occurs from impacted stone in GB neck Emphysematous Cholecystitis Diagnosis Acute Cholecystitis Radionuclide scanning after administration of 99mTc-DISIDA or HIDA Most accurate test to confirm cystic duct obstruction If GB fills with isotope acute cholecystitis unlikely If bile duct visualized but gallbladder not Clinical diagnosis strongly supported Images taken shortly after injection of the radiolabeled tracer. Gallbladder (black spot) fills as radioactive material is secreted into bile and floods in. Images after gallbladder filled. Emptying stimulated by an injection of CCK Enlarging black streak representing the CBD appears below the gallbladder. As streak becomes visible, black spot representing the GB ↓ in size and almost disappears as bile is squeezed into the small intestine. Diagnosis Acute Cholecystitis Ultrasonagraphy: Gallstones (or sludge in acalculous) along with localized tenderness over the GB, pericholecystic fluid, and GB wall thickening strong supportive evidence for acute cholecystitis Oral cholecystograms = no clinical use Unreliable in acutely ill patient Management of Acute Cholecystitis Patients may improve over 1-7 days with expectant management NG suction for profound vomiting, and/or abdominal distension IV fluids, ABX, and analgesics Cholecystectomy Because of high risk of recurrent acute cholecystitis Within first 24-48 hours after acute episode Emergency surgery if advanced disease and complications, usually associated with infection and sepsis. Cholecystostomy (operative or percutaneous) Alternative to cholecystectomy in patients with high operative risk Prognosis Mortality of acute cholecystitis = 5-10% Almost entirely confined to patients >60 with serious associated diseases and those with supparative complications Complications Infection Cholecystoenteric fistula results in gallstone ileus. Choledocholithiasis and Cholangitis Choledocholithiasis & Acute Cholangitis ~15% of pts with gallstones have CBD stones (choledocholithiasis) CD stones usually originate from GB Less commonly stones form de novo in the biliary tree International incidence rate higher b/c primary CBD stones caused by parasites Asians Ascaris lumbricoides and Clonorchis sinensis Biliary tract lithiasis most often begins with a calculus (stone) in the gallbladder. A small enough calculus (or part of a calculus) may become impacted in the neck of the gallbladder or cystic duct acute cholecystitis. The stone may travel further down into the common bile duct, and impaction in this duct (choledocholithiasis) may produce obstruction with jaundice. The stone may travel further down and, near the ampulla, obstruct the pancreatic duct, leading to acute pancreatitis. The stone may pass through the ampulla and out into the duodenum. Symptoms and Signs Biliary colic From rapid in CBD pressure due to obstructed bile flow Charcot’s Triad = classic cholangitis 1. RUQ pain – frequently recurring, severe, persists for several hours 2. Chills and Fever - associated with severe colic 3. Jaundice - associated with abdominal pain Hepatomegaly – in calculous biliary obstruction Tenderness – RUQ and epigastrium Presentation of Choledocholithiasis Pain = MC presenting symptom colicky in nature, moderate in severity, and located in the RUQ intermittent, transient, and recurrent and may be associated with nausea and vomiting. Jaundice CBD becomes obstructed and conjugated bilirubin enters the bloodstream. History of clay-colored stools and tea-colored urine is obtained from such patients in approximately 50% The jaundice can be episodic. Fever Indication of cholangitis Charcot triad: fever, jaundice, and RUQ pain strongly favors the diagnosis. Pancreatitis Gallstones are responsible for 50% of all cases Conversely, 4-8% of patients with gallstones develop pancreatitis. Pancreatitis can be precipitated if CBD obstruction occurs at the level of the ampulla of Vater. Primary CBD Stones Caused by conditions leading to bile stasis and chronic bactibilia. Up to 90% of patients with brown pigment CBD stones have (+) bile culture results Usually brown pigment stones. Brown stones differ from black pigment stones by having a higher content of cholesterol. Brown stones are soft and earthy in consistency and take the shape of the duct. In Western populations, biliary stasis is secondary to factors such as: sphincter of Oddi dysfunction, benign biliary strictures, sclerosing cholangitis, and cystic dilatation of the bile ducts. In Asian populations, A lumbricoides and C sinensis promote stasis: Either blocking the biliary ducts or by damaging the duct walls Results in stricture formation. Bactibilia is also common in these instances, probably secondary to episodic portal bacteremia. Secondary CBD Stones Arise from the gallbladder migrate to the CBD Have a typical spectrum of cholesterol stones and black pigment stones. Bacteria can be cultured from the surface of cholesterol and pigment stones but not from the core, suggesting that bacteria do not play a role in their formation. Laboratory Diagnosis WBC nonspecific. Serum and urine bilirubin - indicate obstruction of the CBD the higher the bilirubin level, the greater the predictive value. CBD stones are present in approximately 60% of patients with serum bilirubin levels greater than 3 mg/dL. Serum amylase and lipase acute pancreatitis complicating choledocholithiasis. Alkaline phosphatase and gamma-glutamyl transpeptidase obstructive choledocholithiasis good predictive value for the presence of CBD stones. Prothrombin time In prolonged CBD obstruction, secondary to depletion of vitamin K (the absorption of which is bile-dependent). Liver transaminases choledocholithiasis complicated by cholangitis, pancreatitis, or both. Blood culture positive in 30-60% of patients with cholangitis. Preoperative Diagnosis Transabdominal ultrasonography It is usually the first modality used in the diagnosis of patients with biliary-related symptoms. Ultrasonography findings are accurate in the diagnosis of gallbladder stones, but CBD stones are missed frequently (sensitivity 15-40%). On the other hand, CBD dilatation is identified accurately, with up to 90% accuracy. Endoscopic ultrasonography Introduction of a high-frequency (7.5-12 MHz) ultrasonic probe advanced into the duodenum under endoscopic guidance. A water-filled balloon is used to provide an acoustic window. Sensitivity and specificity of CBD stone detection are reported in range of 85100%. Invasive, $$$, need experienced enoscopist/ultrasonographer Computed tomography scan very accurate in the detection of biliary tree obstruction and ductal dilatation sensitivity of 75-90% in the detection of CBD stones = essential in evaluation of jaundice. Capable of defining the level of the obstruction and provides information about the surrounding structures, especially the pancreas. MRCP noninvasive tool with 97% accuracy, 92% sensitivity, and 100% specificity. $$$, inconvenience, and limitations (eg, obesity, presence of metal objects, eg, pacemakers) Endoscopic Ultrasound (EUS) MRCP Cholangiography Criterion standard for the detection of CBD stones Endoscopic Retrograde Cholangiopancreatography (ERCP) The CBD is cannulated through the ampulla, contrast injected, and films are obtained. Experience of the endoscopist is best predictor of success, (90-95% in expert hands) Complications = hyperamylasemia and cholangitis. Percutaneous Transhepatic Cholangiography (PTC) may be the modality of choice in patients in whom ERCP is difficult (eg, previous gastric surgery) percutaneously and transhepatically into an intrahepatic duct, and cholangiography is performed. Complications Biliary Cirrhosis: CBD obstruction >30 days liver damage cirrhosis Hypoprothrombinemia: Pts may bleed excessively d/t PT Responds to 10mg parenteral vitamin K or water soluble oral vitamin K within 24-36h. Treatment of Choledocholithiasis CBD stone in pt with cholelithiasis and cholecystitis: endoscopic papillotomy and stone extraction followed by laparoscopic cholecystectomy. ERCP before cholecystectomy in patients with: Gallstones and jaundice (serum bili >2 mg/dL) Dilated CBD (>7mm) Stones in bile duct seen on ultrasound or CT Primary Biliary Cirrhosis Primary Biliary Cirrhosis Chronic disease of liver with autoimmune destruction of intrahepatic bile ducts and cholestasis Insidious onset Often detected by chance finding of Alkaline Phosphatase Women aged 40-60 Disease is progressive and complicated by: Steatorrhea, xanthomas, xanthelasma, osteoporosis, osteomalacia, and portal hypertension Associated with Sjögren’s syndrome, scleroderma, hypothyroidism, and celiac disease Infection with Chlamydia pneumoniae may be trigger or causative agent Xanthoma in PBC Clinical Findings Many asymptomatic for years Fatigue and pruritis Hepatomegaly with progression Xanthomatous lesions In skin and tendons and around eyelids Jaundice and signs of portal HTN (late) Risk of osteoporosis increased Laboratory findings in PBC Signs of cholestasis AlkPhos, cholesterol (HDL), later bilirubin Anti-mitochondrial Antibodies (95%) Directed against PDH in mitochondria Serum IgM Diagnosis of PBC Based on cholestatic liver chemistries and antimitochondrial antibodies in serum combined with characteristic histology in liver biopsy Liver biopsy Permits histologic staging Stage I: Portal inflammation with granulomas Stage II: Bile duct proliferation Stage III: Interlobular fibrous septa Stage IV: Cirrhosis Biliary Fibrosis Portal area with marked ductular proliferation and minimal inflammation in a case of chronic biliary obstruction. Treatment of PBC Ursodeoxycholic Acid Preferred medical treatment slows progression, improves long-term survival, ↓risk of esophageal varices Symptomatic Treatment Cholestyramine or Colestipol - for pruritis Can aggravate steatorrha leading to vitamin A,D,K deficiency Rifampin inconsistently beneficial Opiod antagonists Naloxone, naltrexone – show promise for treating pruritis 5-HT3 antagonists Ondansetron Calcium supplementation Helps prevent osteomalcia Colchicine and Methotrexate Some benefit improving symptoms and serum levels of AP Liver transplant Treatment of choice for advanced disease Prognosis of PBC Without transplant, survival = 7-10 years once symptoms develop Adverse prognostic indicators: Older age High serum bilirubin Edema Low serum albumin Prolonged PT Variceal hemorrhage The Mayo risk score: R = 0.871 loge (bilirubin in mg/dL) + (–2.53) loge (albumin in g/dL) + 0.039 age in years + 2.38 loge(prothrombin time in seconds) + 0.859 (edema score of 0, 0.5, or 1) Primary Sclerosing Cholangitis Primary Sclerosing Cholangitis Uncommon disease characterized by diffuse inflammation of biliary tract leading to fibrosis and strictures of biliary system. Most common in men age 20-40 and closely associated with ulcerative colitis (present in ~2/3 of pts with PSC) Only 1-4% of patients with UC develop PSC. Like UC, smoking is associated with a ↓risk of PSC Associated with HLA-B8 and DR3 or DR4 ANCA (70%), with fluorescent staining characteristics and target antigens distinct from those in Wegener’s In AIDS, PSC may result from infections caused by CMV, cryptosporidium, or microsporum. PSC is usually progressive, leading to cirrhosis, portal hypertension, and liver failure. Symptoms and Signs Progressive obstructive jaundice Frequently associated with malaise, pruritus, anorexia, and indigestion. Complications of chronic cholestasis Osteoporosis Malabsorption of fat soluble vitamins Laboratory Diagnosis of PSC AP or GGT – MC abnormality Serum transaminases can be normal or serum bilirubin in advanced PSC Hepatic synthetic tests (albumin, PT, etc) abnormal in advanced PSC Serum cholylglycine (bile salt) out of proportion to the elevation of serum bilirubin. p-ANCAs in 60-82% of patients with PSC. (Frequency in UC is similar.) CA 19-9 level greater than 100 U/mL has 75% sensitivity and 80% specificity in identifying PSC patients with cholangiocarcinoma. Imaging Diagnosis of PSC ERCP Cholangiography remains criterion standard Cholangiography remains the criterion standard for establishing the diagnosis of PSC. irregularly distributed, multifocal strictures and dilatations of the intrahepatic and extrahepatic bile ducts = beading MRCP Noninvasive, but less sensitive (90%) than ERCP(97%) for visualizing intrahepatic ducts Imaging of PSC The radiographic pattern of PSC is that of strictures of varying lengths in the intrahepatic and extrahepatic ducts. There may intervening areas of minimal dilatation of the ducts with a resulting "beaded" appearance. Usually there are multiple areas of involvement. In this case almost all of the visualized ducts are abnormal in contour. ERCP ERCP image shows multifocal strictures and irregularity of the right intrahepatic bile ducts. Treatment of PSC No effective medical therapies exist Ciprofloxacin Episodes of acute bacterial cholangitis Ursodeoxycholic acid (UDCA) improves symptoms and LFTs in adult patients with PSC. ERCP Balloon dilation of localized strictures. Repeated procedures improves survival. If major stricture – short term stent relieves symptoms and improves LFTs Surgical resection In patients without cirrhosis, resection of dominant bile duct stricture may improve survival vs. ERCP because of ↓risk cholangiocarcinoma. Prognosis of PSC Averages 10 years once symptoms appear Adverse prognostic markers: Older age Higher serum bilirubin and AST Lower albumin levels History of variceal bleeding Complications: Cholangiocarcinoma (10-15%) of adults with PSC. Colon CA/dysplasia In patients with ulcerative colitis, PSC is independent risk factor Strict adherence to colonoscopic surveillance program avised Neoplasms in the Biliary Tract Carcinomas of Biliary Tract Manifestations weight loss (77%) nausea (60%) anorexia (56%) abdominal pain (56%) fatigue (63%) pruritus (51%) fever (21%) malaise (19%) diarrhea (19%) constipation (16%) abdominal fullness (16%) Symptomatic patients usually have advanced disease, with spread to hilar lymph nodes before obstructive jaundice occurs. It is associated with a poor prognosis. Carcinoma of the Gallbladder Uncommon malignancy – 2.5/100,000 Most common of biliary tract cancers (54%) >90% are adenocarcinomas In Native Americans, GB carcinoma is the most commonly seen GI malignancy Male:Female = 1:3 Overall mean survival rate = 6 months, 5-year survival rate is 5% At diagnosis, most of the GB is replaced or destroyed by the cancer Risk Factors for GB Cancer Cholelithiasis often large and symptomatic stones present Chronic infection of gallbladder Salmonella Typhi Genetic Factors GB polyps >1cm in diameter Mucosal calcification of GB (Porcelain GB) carcinoma in 25% Anomalous pancreaticobiliary ductal junction Congenital biliary cysts Environmental carcinogens Anabolic Steroids I'm not a crazy person. I'm not stupid. No hablo ingles! Baseball be very good to me Symptoms and Signs Jaundice skin or icteric sclerae Early Pain in RUQ with radiation into back Anorexia, weight loss, fever and chills (cholangitis), supraclavicular LN Courvoisier’s Law Palpable GB with obstructive jaundice signifies malignant disease This generalization accurate only 50% of time Hepatomegaly Usually present and associated with liver tenderness Ascites Can occur with peritoneal implants Hematemesis or melena From erosion of tumor into blood vessel (hemobilia) Carcinoma of Gallbladder Location: fundus (60%), body (30%), neck (10%) Notoriously insidious Diagnosis made incidently at surgery Spread Early lymphatic spread retroperitoneal, right celiac, and pancreaticoduodenal nodes. Direct invasion of the liver, extrahepatic biliary ducts, and duodenum and colon (less common) occurs. Intraperitoneal seeding may occur. TNM Staging Tis = Carcinoma in situ Stage 0: Tis N0 M0 T1a = GB wall: invades lamina propria T1b = GB wall: invades muscle layer Stage I: T1 N0 M0 T2 = Perimuscular connective tissue Stage II: T2 N0 M0 Stage III: T1-2 T3 N1 N0-1 M0 M0 Stage IVA: T4 N0-1 M0 Stage IVB: T1-4 T1-4 N2 N0-2 M0 M1 T3 = Perforates serosa or directly invades liver or adjacent organ T4 = Invades main portal vein or hepatic artery or multiple organs N1a = Hepatoduodenal ligament nodes N1b = Other regional lymph nodes M0 = No distant metastases M1= Distant metastases Carcinoma of Bile Ducts (Cholangiocarcinoma) Tumor that arises from the intrahepatic or extrahepatic biliary epithelium 3% of all cancer deaths in the US > 90% are adenocarcinomas, remainder are squamous cell CA 3 Geographic Locations: Intrahepatic Least common Extrahepatic (ie, perihilar) Perihilar (Klatskin tumors) = Most common At bifurcation of R and L hepatic ducts Distal extrahepatic Upper border of pancreas ampulla The etiology of most bile duct cancers remains undetermined. Possible Etiologies Infections In SE Asia, chronic infx with liver flukes Clonorchis sinensis, Opisthorchis viverrini and Fasciola Hepatica Inflammatory bowel disease CCC generally develops in patients with long-standing ulcerative colitis and PSC. Chemical exposures primarily among workers in the aircraft, rubber, and wood finishing industries. Thorotrast Congenital diseases of the biliary tree choledochal cysts and Caroli disease Pathophysiology of CCC Long-standing inflammation as with PSC, chronic parasitic infection suggested to play a role by inducing hyperplasia cellular proliferation malignant transformation. Grow slowly and infiltrate walls of the ducts, dissecting along tissue planes Local extension: liver, porta hepatis, regional LN of the celiac and pancreaticoduodenal chains. Symptoms and Signs Progressive jaundice MC manifestation of bile duct cancer The obstruction and subsequent cholestasis tends to occur early if the tumor is located in the common bile duct or common hepatic duct. Jaundice often occurs later in perihilar or intrahepatic tumors and is often a marker of advanced disease. The excess of conjugated bilirubin is associated with bilirubinuria and clay colored stools. Pruritus usually is preceded by jaundice, but itching may be the initial symptom of CCC. related to circulating bile acids. Weight loss Abdominal pain common in advanced disease and often is described as a dull ache in the RUQ Courvoisier’s Sign If CCC located distal to the cystic duct takeoff the patient may have a palpable gallbladder, (Courvoisier sign) Laboratory Examination Biliary Neoplasms Conjugated Bilirubin Total serum bilirubin from 5-30mg/dL Alkaline Phosphatase and GGT Serum Cholesterol AST normal or mildly elevated CA 19-9 If elevated – may help distinguish CCC from benign biliary stricture Imaging in Biliary Neoplasms Ultrasonagraphy and CT: Show GB mass in GB Carcinoma Intrahepatic masses or biliary duct dilation CT also shows involved regional LN MRI with MRCP Visualization of biliary tree Detection of vascular invasion Positron Emission Tomography (PET) Can detect CCC as small as 1cm The most helpful diagnostic studies before surgery are either PTC or ERCP with biopsy and cytology Treatment of Biliary Neoplasms Curative Surgery (Gallbladder CA) May be attempted in young and fit pts if tumor is well localized. 5 year survival for localized (stage 1, T1a, N0, M0) is as high as 80% with laparoscopic cholecystectomy Only 15% if muscular invasion (T1b) If tumor unresectable at laparotomy Cholecystoduodenostomy or T-tube drainage of CBD Curative Surgery (CCC) Curable in <10% Palliation - place self-expandable metal stent via ERCP or PTC Photodynamic therapy – palliative Radiotherapy Relieve pain and contributes to biliary decomression Chemotherapy with gemcitabine – limited response In general, prognosis is poor, with few patients surviving >12 months after surgery A 95 year-old woman presented with upper abdominal pain and jaundice; ultrasound demonstrated gallstones. Symptoms were short in duration, and jaundice began to clear rapidly. In view of her age and improving condition, she was treated conservatively for cholecystitis. However, she then developed protracted vomiting; endoscopy demonstrated several stones in the duodenum. What is the most likely cause this type of complication? a. Malignancy extending into duodenum b. Perforation of gallbladder c. Caroli’s syndrome d. Metastasis from another primary tumor Answer B. This stone could not be removed endoscopically. Surgery confirmed the suspicion that the gallbladder had perforated into the duodenum, releasing the stones into the duodenal lumen. Measurement of the largest stone after surgical removal revealed it to be over 5 cm in length (right).