Best Disease - University of Louisville Department of Ophthalmology
advertisement
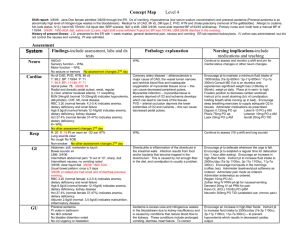
Grand Rounds Best Disease Mark Sherman MD University of Louisville Department of Ophthalmology and Visual Sciences 04/04/2014 Subjective CC: Distorted vision x several months HPI: 45 year old white male presented to general clinic with complaint of worsening distortion of vision in both eyes for several months. Patient stated he had noticed a deterioration in his vision in his early 30s but the distortion was new over the past several months. Patient denied any other ocular complaints. POH: None PMH: COPD Meds: Inhalers, Prednisone FH: Uncle: Best Dz, Grandfather: AMD Exam BCVA: OD 20/25 OS 20/25 Pupils: 53 53 No APD IOP: EOM: 14 14 Full OU Anterior Segment SLE: L/L Conjunctiva K AC I/L OD OS WNL WNL WNL WNL WNL WNL WNL WNL WNL WNL DFE Bilateral round, yellow lesions involving the fovea OCT OD OS Bilateral subretinal lesions with preservation of the retinal architecture Assessment/Differential Diagnosis Assessment: 45 year old white male with bilateral “yolk-like” subretinal lesions DDx: 1) Adult Vitelliform Dystrophy 2) Best Disease Adult Vitelliform Pattern Dystrophy Caused by mutations in the RDS/peripherin gene Characterized by: Yellow subfoveal lesions that are bilateral Round or oval shape Typically one-third disc diameter in size Often contain a central pigmented spot Adult Vitelliform Pattern Dystrophy Usually appears in the fourth to sixth decade of life Presenting symptoms include: mild blurring of vision and metamorphospia Over time the lesions fade and leave an area of RPE atrophy Visual prognosis is guarded and is directly related to the size of the lesion and its location within the macula Best Disease Autosomal dominant maculopathy Caused by mutations in the Best1 (VMD2) gene on chromosome 11 which codes for the protein bestrophin Bestrophin: functions as a transmembrane chloride channel in the basolateral plasma membrane on the RPE The dysfunctional ion transport leads to accumulation of lipofuscin Best Disease Affected individuals present with a yellow, yolk-like (vitelliform) macular lesion in childhood or early adulthood The lesion eventually breaks down, leaving a mottled geographic atrophic appearance Best Disease Diagnosis: Primarily a clinical diagnosis EOG: Always abnormal ERG: Typically normal Prognosis: Visual prognosis is usually good with most patients maintaining 20/30 acuity Choroidal neovascularization does occur in approximately 20% of cases Best Disease vs Adult Vitelliform Dystrophy Lesion size: Usually larger in Best disease, typically 1/3 disc diameters in adult vitelliform dystrophy Age of presentation: Childhood to early adulthood in Best disease and typically between the fourth and sixth decade in adult vitelliform dystrophy Electro-oculogram (EOG): Abnormal in best disease and normal in adult vitelliform dystrophy Intravitreal bevacizumab for choroidal neovascularization associated with Best’s Disease Case report of a 27 year old woman who presented with 20/200 vision in her right eye; was found to have intraretinal hemorrhage in the macula with a neurosensory detachment The left eye showed a vitelliform lesion in the macula Best disease was confirmed with EOG Patient was given a single dose of intravitreal Avastin Four weeks after treatment the vision had improved to 20/25 and remained stable for 12 months of follow up References BCSC: Retina and Vitreous. Vitelliform Degenerations. Pgs: 236-237 Boon CJ, Levering BJ, Leroy BP, Hoyng CB, et al. The spectrum of ocular phenotypes caused by mutations in BEST1 gene. Prog Retin Eye Res. 2009;28(3):187-205 Fishman GA, Baca W, Alexander KR, et al. Visual acuity in patients with Best vitelliform macular dystrophy. OphthalmologyI. 1993;100(11):1665-1670 Petrukhin K, Koisti MJ, et al. Identification of the gene responsible for Best macular dystrophy. Nat Genet. 1998;19(3)241-247. Velazquez-Villoria D, Macia C, et al. Intravitreal bevacizumab for choroidal neovascularization associated with Best’s Disease. Arch Soc Esp Opht. 2014.