Concept Map Level 4 - Student Nurse Journey
advertisement
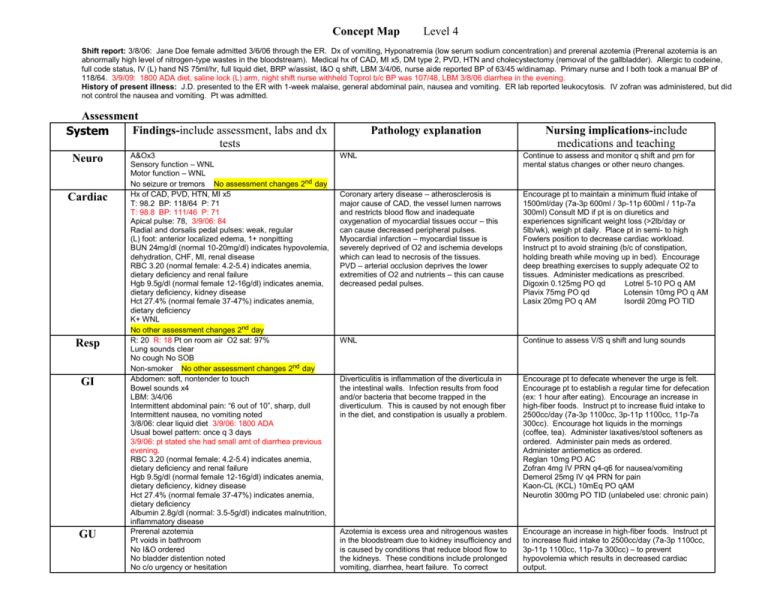
Concept Map Level 4 Shift report: 3/8/06: Jane Doe female admitted 3/6/06 through the ER. Dx of vomiting, Hyponatremia (low serum sodium concentration) and prerenal azotemia (Prerenal azotemia is an abnormally high level of nitrogen-type wastes in the bloodstream). Medical hx of CAD, MI x5, DM type 2, PVD, HTN and cholecystectomy (removal of the gallbladder). Allergic to codeine, full code status, IV (L) hand NS 75ml/hr, full liquid diet, BRP w/assist, I&O q shift, LBM 3/4/06, nurse aide reported BP of 63/45 w/dinamap. Primary nurse and I both took a manual BP of 118/64. 3/9/09: 1800 ADA diet, saline lock (L) arm, night shift nurse withheld Toprol b/c BP was 107/48, LBM 3/8/06 diarrhea in the evening. History of present illness: J.D. presented to the ER with 1-week malaise, general abdominal pain, nausea and vomiting. ER lab reported leukocytosis. IV zofran was administered, but did not control the nausea and vomiting. Pt was admitted. Assessment Findings-include assessment, labs and dx System tests A&Ox3 Neuro Sensory function – WNL Cardiac Resp GI GU Motor function – WNL No seizure or tremors No assessment changes 2nd day Hx of CAD, PVD, HTN, MI x5 T: 98.2 BP: 118/64 P: 71 T: 98.8 BP: 111/46 P: 71 Apical pulse: 78, 3/9/06: 84 Radial and dorsalis pedal pulses: weak, regular (L) foot: anterior localized edema, 1+ nonpitting BUN 24mg/dl (normal 10-20mg/dl) indicates hypovolemia, dehydration, CHF, MI, renal disease RBC 3.20 (normal female: 4.2-5.4) indicates anemia, dietary deficiency and renal failure Hgb 9.5g/dl (normal female 12-16g/dl) indicates anemia, dietary deficiency, kidney disease Hct 27.4% (normal female 37-47%) indicates anemia, dietary deficiency K+ WNL No other assessment changes 2nd day R: 20 R: 18 Pt on room air O2 sat: 97% Lung sounds clear No cough No SOB Non-smoker No other assessment changes 2nd day Abdomen: soft, nontender to touch Bowel sounds x4 LBM: 3/4/06 Intermittent abdominal pain: “6 out of 10”, sharp, dull Intermittent nausea, no vomiting noted 3/8/06: clear liquid diet 3/9/06: 1800 ADA Usual bowel pattern: once q 3 days 3/9/06: pt stated she had small amt of diarrhea previous evening. RBC 3.20 (normal female: 4.2-5.4) indicates anemia, dietary deficiency and renal failure Hgb 9.5g/dl (normal female 12-16g/dl) indicates anemia, dietary deficiency, kidney disease Hct 27.4% (normal female 37-47%) indicates anemia, dietary deficiency Albumin 2.8g/dl (normal: 3.5-5g/dl) indicates malnutrition, inflammatory disease Prerenal azotemia Pt voids in bathroom No I&O ordered No bladder distention noted No c/o urgency or hesitation Pathology explanation Nursing implications-include medications and teaching WNL Continue to assess and monitor q shift and prn for mental status changes or other neuro changes. Coronary artery disease – atherosclerosis is major cause of CAD, the vessel lumen narrows and restricts blood flow and inadequate oxygenation of myocardial tissues occur – this can cause decreased peripheral pulses. Myocardial infarction – myocardial tissue is severely deprived of O2 and ischemia develops which can lead to necrosis of the tissues. PVD – arterial occlusion deprives the lower extremities of O2 and nutrients – this can cause decreased pedal pulses. Encourage pt to maintain a minimum fluid intake of 1500ml/day (7a-3p 600ml / 3p-11p 600ml / 11p-7a 300ml) Consult MD if pt is on diuretics and experiences significant weight loss (>2lb/day or 5lb/wk), weigh pt daily. Place pt in semi- to high Fowlers position to decrease cardiac workload. Instruct pt to avoid straining (b/c of constipation, holding breath while moving up in bed). Encourage deep breathing exercises to supply adequate O2 to tissues. Administer medications as prescribed. Digoxin 0.125mg PO qd Lotrel 5-10 PO q AM Plavix 75mg PO qd Lotensin 10mg PO q AM Lasix 20mg PO q AM Isordil 20mg PO TID WNL Continue to assess V/S q shift and lung sounds Diverticulitis is inflammation of the diverticula in the intestinal walls. Infection results from food and/or bacteria that become trapped in the diverticulum. This is caused by not enough fiber in the diet, and constipation is usually a problem. Encourage pt to defecate whenever the urge is felt. Encourage pt to establish a regular time for defecation (ex: 1 hour after eating). Encourage an increase in high-fiber foods. Instruct pt to increase fluid intake to 2500cc/day (7a-3p 1100cc, 3p-11p 1100cc, 11p-7a 300cc). Encourage hot liquids in the mornings (coffee, tea). Administer laxatives/stool softeners as ordered. Administer pain meds as ordered. Administer antiemetics as ordered. Reglan 10mg PO AC Zofran 4mg IV PRN q4-q6 for nausea/vomiting Demerol 25mg IV q4 PRN for pain Kaon-CL (KCL) 10mEq PO qAM Neurotin 300mg PO TID (unlabeled use: chronic pain) Azotemia is excess urea and nitrogenous wastes in the bloodstream due to kidney insufficiency and is caused by conditions that reduce blood flow to the kidneys. These conditions include prolonged vomiting, diarrhea, heart failure. To correct Encourage an increase in high-fiber foods. Instruct pt to increase fluid intake to 2500cc/day (7a-3p 1100cc, 3p-11p 1100cc, 11p-7a 300cc) – to prevent hypovolemia which results in decreased cardiac output. Musc-skel Integ Endocrine Psychosocial RBC 3.20 (normal female: 4.2-5.4) indicates anemia, dietary deficiency and renal failure Hgb 9.5g/dl (normal female 12-16g/dl) indicates anemia, dietary deficiency, kidney disease BUN 24mg/dl (normal 10-20mg/dl) indicates hypovolemia, dehydration, CHF, MI, renal disease/failure Crea: WNL K+ WNL No assessment changes 2nd day Limb movements x4 WNL No c/o pain/stiffness Pt sits, walks, stands and turns independently Posture/gait: WNL No assessment changes 2nd day Skin warm and dry Skin intact (L) foot: anterior localized edema, 1+ nonpitting No assessment changes 2nd day Glucose: 3/7/06: 223 3/8/06: 150 3/9/06: 119 azotemia, you need to correct the source of the problem, which is reduced blood flow. Place pt in semi- high Fowlers position to reduce cardiac workload, instruct pt to avoid straining. Promote physical and emotional rest. Encourage deep breathing for adequate tissue oxygenation. Kaon-CL (KCL) 10meq PO qAM WNL Continue to monitor for any problems with walking or pain q shift/prn. Edema due to cardiovascular problems as stated above. Continue to assess and monitor edema and skin for any changes q shift and prn. DM type 2 is due to insulin resistance of the cells response, or the pancreas doesn’t produce enough insulin and this affects protein, carbohydrate and fat metabolism. Pt has family/friends that visit. She lives alone. She does not drink alcohol. She is knowledgeable about her medical hx conditions, though she seems to lack knowledge regarding nutrition. She suffers from insomnia sometimes. Nutrition problems in the elderly can be common, could be due to financial resources or knowledge deficit on nutrition facts. Assess for s/sx of hyperglycemia q shift and prn. (frequent urination, excess thirst/hunger, dry mouth, fatigue, weight loss). Administer insulin as ordered. Novolog sliding scale SC AC HS Novolin 70/30 SC BID AC 35units Assess reasons for nutrition deficit. If financial, refer pt to sources (ex: Lone Star program), if knowledge deficit, pt needs teaching on her nutrition. Encourage family involvement. Ambien 10mg PO HS PRN for insomnia Discharge planning: indicate likely patient needs or ongoing problems on discharge. Nursing actions to provide for those needs. Need: Pt needs teaching regarding how to prevent constipation. Action: Help pt to understand and know that certain medications can have a constipating side effect. Send home with her a cup with measurement on it just like she used in the hospital. MD contact – if physician needed to be called, state what you would say: Dr. was not called. Sample phone call: I would have the MAR, labs, chart available before placing this call. Hi, this is Community City hospital calling about your patient Jane Doe. in room 22A. She has developed increased abdominal pain “10 out of 10” and is doubled over. The location of the pain is in the LLQ with distention. She is doubled over in pain and crying. The Demerol was given 20 mins ago and has not helped. There is no bladder distention. Would you like me to prep her for an MRI, CT scan or ultrasound? Also would you like to increase the Demerol or administer another pain medication? I would write down any orders as he/she speaks, and then read them back to him for confirmation. I would document that I made the phone call and what time it was made, as well as any new orders he gave. Prioritize: list your patients in order of priority; least stable to most stable: explain why 1. 2. 3. 4. 5. J.J. 62yr old Caucasian female admitted 3/8/06, dx new onset seizure and UTI. Pt is A&Ox2, stays confused and cannot recall why she is in Hospital. Husband w/Parkinson’s at bedside, and she believes he was the one admitted. She called a friend to come get her and take her home. Friend arrived and was able to give some history on both of them. Pt is alcoholic, but denied alcohol use on admission. Other circumstances Alerted nurse to call adult protective services. S.M. is a 64yr old Caucasian female admitted 3/8/06, dx of pneumonia w/hx of a stroke. Bilateral lung sounds rales/ronchi. V/S WNL. Bilateral upper Extremities experienced ongoing uncontrolled movements. C.G. 67yr old Caucasian female admitted 3/6/06, dx vomiting, Hyponatremia and prerenal azotemia. Hx of CAD, MI x5, PVD, DM type 2, HTN, cholecystectomy. V/S WNL J.S. 55yr old Hispanic male admitted 3/5/06, dx acute cholecystitis, cholecystectomy on 3/6/06, V/S WNL, pt ambulates independently, d/c home 3/8/06. R.H. 19yr old Caucasian male admitted 3/5/06, dx of (R) ankle infection, V/S WNL, pt ambulates independently, no wound, skin intact, d/c home 3/8/06. Teaching: GI – teaching regarding nutrition to prevent constipation Encourage pt to drink something warm in the mornings (cup of coffee) and something warm in the evenings (cup of tea). This will promote bowel activity. Encourage pt to eat small frequent meals/snacks. Encourage pt to eat supplement bars high in fiber for snacks. Encourage pt to increase and to measure her liquids. Advise a minimum of 2000cc – 2500cc/day. (ex: 7a-3p drink 150cc/hr to intake 1200cc/8hr). Provide pt with small cup with measurement lines. Instruct pt how to include more fiber in her diet (ex: avocado, blackberries, baked beans, raisin bran) and increase her fluid intake (ex: 2500cc/day) Author Unknown