NSOI - University of Louisville Department of Ophthalmology and
advertisement

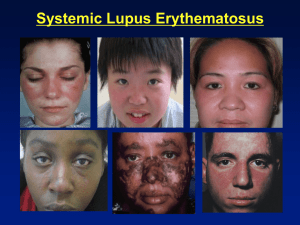
Grand Rounds Shivani V. Reddy, M.D. University of Louisville Department of Ophthalmology and Visual Sciences Patient Presentation CC: Left Eye Pain HPI: 31 y/o WF presents to the ER with 5 days of pain/pressure OS . She describes the pain as 8/10, deep and stabbing in quality with gradual worsening over the 5 day period. Denies blurry vision, photophobia or foreign body sensation. History POHx: episode of OD pain 7 months prior - CT orbits with OD superior rectus, lateral rectus and lacrimal gland enlargement - resolved with Prednisone 60 mg PO Q.day x 2 weeks myopia PMHx: migraines, anxiety FAMHx: no known thyroid or autoimmune diseases ROS: URI which she recovered from 3 weeks prior MEDS: benadryl, protonix, flexaril, depakote ALLERGIES: lortab, toradol, sulfa antibiotics Exam 8 20/20 VA TP 20/20-2 12 4→3 P 4→3 no RAPD EOM: -1 restriction in all gazes with pain OS no diplopia MRD 1: 4mm OU no lid lag no proptosis OS Exam OD OS LIDS/LASHES WNL WNL CONJ WNL WNL CORNEA WNL, no staining WNL, no staining IRIS WNL WNL LENS WNL WNL FUNDUS EXAM: c/d: 0.3 with sharp rim OU MVP wnl OU PHYSICAL EXAM: no cervical/submandibular LAD CT SCAN Enlargement of superior oblique muscle OS, no lacrimal gland involvement Summary 32 y/o WF presents with 5 days of OS pain worsened on EOM with minor movement restriction in all gazes. Ant segment and fundus exam WNL. CT scan shows swelling of superior oblique muscle. She had a similar episode OD previously that resolved upon treatment with corticosteroids DDx: Thyroid Eye Disease Autoimmune Disease Orbital malignancy Infectious (orbital cellulitis) NSOI Laboratory Workup - ESR - CRP - CBC WNL WNL WNL ANA negative ACE WNL Thyroid Function Tests - Free T4 WNL - T3 WNL - TSH WNL - TSI negative - T-Perox negative Summary 32 y/o WF presents with 5 days of OS pain worsened on EOM with minor movement restriction in all gazes. Ant segment and fundus exam WNL. CT scan shows swelling of superior oblique muscle. She had a similar episode OD previously that resolved upon treatment with corticosteroids. Negative Workup DDx: Thyroid Eye Disease Autoimmune Disease Orbital malignancy Infectious (orbital cellulitis) NSOI Treatment Started on oral Prednisone 1mg/kg with ranitidine 3 day follow-up Pain and EOM restriction resolved Started on slow taper No recurrences as of 2 weeks ago per telephone follow-up Nonspecific Orbital Inflammation (NSOI) Also known as: Inflammatory orbital pseudotumor Idiopathic orbital inflammatory syndrome Benign process characterized by polymorphous lymphoid infiltrate +/- fibrosis of varying degrees No known local or systemic cause Diagnosis of exclusion Controversial pathogenesis, likely cell mediated NSOI typically unilateral in adults, but upto 1/3 bilateral in children 5 main locations in order of frequency: Lacrimal gland (darcryoadenitis) Extraocular muscles (myositis) 50% with tendon involvement Anterior orbit +/- tenons involvement (ring sign) Orbital apex Diffuse Sclerosing subtype with marked orbital fibrosis NSOI Variable presentation depending on location Most typical feature is deep-rooted boring retro-orbital pain Other common features EOM restriction +/- pain Proptosis Conjunctival Inflammation Chemosis Upper eyelid erythema Children commonly present with uvietis, disc edema and eosinophilia NSOI Lab findings: Elevated ESR CBC with eosinophilia + ANA levels Mild CSF pleocytosis Histological Findings Pleomorphic cellular infiltrate with lymphocytes, plasma cells and eosinophils, later stages with fibrotic changes Sclerosing subtype shows very little inflammation NSOI Dacryoadenitis with marked inflammation and expansion along the lateral orbital wall. Diffuse gland enlargement with blurring of margins NSOI Extraocular muscle inflammation with tubular enlargement 2/2 tendon involvement medial rectus > superior muscle complex > lateral rectus > inferior rectus NSOI Diffuse orbital involvement showing fat enhancement (asterix’s) Diagnosis Based on a combination of clinical symptoms, labs and imaging Biopsy if - diagnosis uncertain, atypical presentation, poor response to initial medical treatment Treatment Mild cases Observation NSAIDS + PPI Moderate - Severe Cases Corticosteroids are mainstay of therapy at 1mg/kg dosing Slow taper to ensure complete suppression of inflammation Refractory Cases & Sclerosing Variant Immunomodulator therapy Cyclosporine, cyclophosphamide, methotrexate Low dose radiation Response/Prognosis 78% with +ve initial response BUT only 37% cured , 52% disease recurrence Patients with optic neuropathy 2/2 compression showed 95% response rate Sclerosing subtype tends to show less of a treatment response Per 2007 review of 56 published biopsy proven NSOI cases 34% have complete resolution 43% with partial resolution 23% refractory Ophthal Plast Reconstr Surg 2013;29:286–289) • Prospective, noncomparitive interventional case series • 47 patients with acute idiopathic orbital inflammation • Dacryoadenitis – 31 • Myositis – 12 • Diffuse – 4 cases • Patients injected with 2-4 ml betamethasone suspension through a 22 gauge needle into the inflamed gland, around the inflamed muscle and periocularly in diffuse cases • After injection, NSAIDS + topical steroid treatment for 2 weeks •F/U was weekly x 1 month, every 3 months x 1 year, then yearly • Dacryoadenitis – 31 cases (4 recurrent) • 25 cases 2ml suspension, 6 cases 4ml suspension • Mean age 26.4 years , F>M (24:7) • Complete response - 1-2 weeks • No recurrences/complications • Myositis - 12 cases (1 recurrent) • 2ml suspension • Mean age 27.4 years , M>F (9:3) • Complete response - 1-2 weeks • 1 recurrence 14 months post with LR inflammation- resolved after inj#2 • No other recurrences/complications • Diffuse Inflammation – 4 cases (2 recurrent) • 4 ml suspension • Mean age 29.2 years, all men • Complete response - 1-4 weeks • 1 recurrence 9 months post , resolved after inj #2 • No other recurrences/complications THANK YOU References BCSC Section 4. Ophhtalmic Pathology and Intraocular tumors BCSC Section 8. Orbit, Eyelids and Lacrimal System Ding ZX, Lip G, Chong V. Idiopathic orbital pseudotumor. Clinical Radiology 2011;66:886-892 Kapur R, Sepahdari AR, Mafee MF, et al. MR imaging of orbital inflammatory syndrome, orbital cellulitis, and orbital lymphoid lesions: the role of diffusionweighted imaging. AJNR Am J Neuroradiol 2009;30:64-70 Mombaerts I, Schingmann RO, Goldschmeding R, et al. Are systemic corticosteroids useful in the management of orbital pseudotumors? Ophthalmol. 1996;103:521-528 Ahn Yuen SJ, Rubin PAD. Idiopathic Orbital Inflammation Distribution, Clinical Features, and Treatment Outcome. Arch Ophthalmol. 2003;121:491-499 Swamy BN, McCluskey P, Nemet A, Crouch R, Martin P, Benger R, Ghabriel R, Wakefield D. Idiopathic orbital inflammatory syndrome: Clinical features and treatment outcomes. Br J Ophthalmol 2007;91:1667-1670