Corneal Dystrophy - University of Louisville Ophthalmology
advertisement

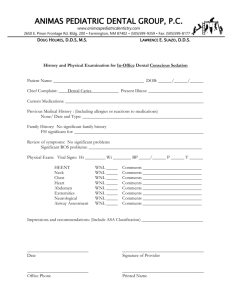
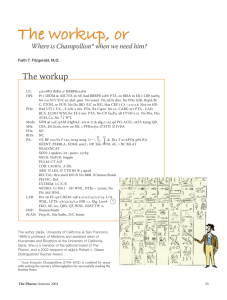
Grand Rounds Amir R. Hajrasouliha, M.D. University of Louisville Department of Ophthalmology and Visual Sciences Friday, June 20th, 2014 Case Presentation CC: Gradual blurred vision OU HPI: 26 y/o otherwise healthy caucasian male present with progressive decrease of vision OU (OD>OS) in past year. The patient reported that he had bilateral laser vision correction (LASIK) 4 years ago. Case presentation: History POHx: LASIK 4 years ago PMHx: None Eye med: None Meds: None FH: Mother with unknown corneal dystrophy 20/40-2 -1.00 sphere VA 20/20-1 sc T 12 P 11 wnl wnl EOM and CVF Full Right Left External WNL WNL Lids WNL WNL Conjunctiva White and quiet White and quiet Cornea s/p LASIK with multiple round/disc-shaped intrastromal corneal opacities with intervening clear stroma sparing the peripheral corneal s/p LASIK with few intrastromal corneal opacities Anterior Chamber Deep and quiet Deep and quiet Iris WNL WNL Lens WNL WNL DFE WNL WNL OD OS OCT OD OCT OD OCT OD OCT OD OCT OD OCT OS OCT OS Assessment & Plan 26 y/o male with corneal deposits at interface post LASIK OU ; OD>>OS • Granular corneal dystrophy OU Management Observation Laser refractive surgery (LRS) is contraindicated in • Unstable refractive error • Keratoconus • Herpetic keratitis • Significant cataract • Uncontrolled glaucoma • Uncotrolled diabetes • Uncontrolled collagen vascular disease • Pregnancy • Pt on amiodarone and isotretinoin LASIK is contraindicated in Epithelial basement membrane dystrophy (EBMD) Fuchs PRK is treatment of choice for EMBD and its safety in Fuchs is not established Granular corneal dystrophy type I Inheritance: Autosomal dominant Pathology: Hyaline material, stain bright red with Masson trichrome stain. Hyper-reflective opacities are seen on confocal microscopy. Mutation: TGFBI gene on chromosome 5q31 Clinical finding Onset early in life around teens Lesions do not extend to limbus but can extend anterioly through focal breaks in Bowman layer. Slowly progressive with vision only rarely dropping to 20/200 after age 40. Recurrent erosions occur and vision decreases as the opacities become more confluent. Treatment Early in disease, no treatment is needed. Recurrent erosions may be treated with contact lens, superficial keratectomy, or PTK When visual acuity is affected, DALK or PK has a good prognosis. Recurrence in the graft (anterior and peripherally) may occur after many years as fine sub-epithelial opacities varying from the original presentation. PTK treatment for GCD1 Clinical & Experimental Ophthalmology, 34, no. 8 (2006): 808-810 In 2002 and 2003 there were some reports from Japan that demonstrated corneal electrolysis for granular lesions at the interface after LASIK surgery, resulted in clearing of the cornea ; however, the technique did not become popular as the recurrence rate was high. Deposits of Transforming Growth Factor-[beta]-Induced Protein in Granular Corneal Dystrophy Type II After LASIK. Kim, Tae-im; Roh, Mi; Grossniklaus, Hans; E MD, MBA; Kang, Shin; Jeong MD, PhD; Hamilton, Stephen; Schorderet, Daniel; Lee, W; Kim, Eung; Kweon MD, PhD Cornea. 27(1):28-32, January 2008. DOI: 10.1097/ICO.0b013e318156d36d © 2008 Lippincott Williams & Wilkins, Inc. Published by Lippincott Williams & Wilkins, Inc. 2 Secondary wound healing process induce TGF-β secretion which stimulates mutated TGFβI protein product synthesis (keratoepithelin or TGFβIp). The misfolded protein then accumulates as the insoluble protein aggregates and results in clinical defect. Munier FL, et al. Kerato-epithelin mutations in four 5q31-linked corneal dystrophies. Nature Genetics. 1997; 15: 247-251. Thank You