- The 1st Kuwait
advertisement

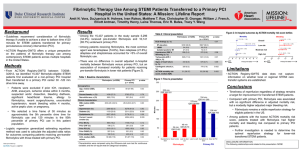
Updates in Acute Coronary Syndromes Management Mohammad Zubaid, MB, ChB, FRCPC, FACC Professor of Medicine, Kuwait University Head, Division of Cardiology Mubarak Alkabeer Hospital Kuwait The 1st Kuwait-North American update in Internal Medicine 4th Medical Scientific Conference – Mubarak Alkabeer Hospital February 7, 2014 – Jumeirah hotel, Kuwait From plaque formation to progression to clinical manifestations Plaque formation Risk factor Clinical manifestations Slow progression Atherosclerosis Accelerated Progression Atherothrombosis STABLE No symptoms Silent ischemia Stable angina UNSTABLE Unstable angina NSTEMI STEMI Sudden cardiac death Distribution of ACS type in Kuwait Discharge diagnosis 2534 patients Gulf COAST 2012 Kuwait population Age (Mean ±SD) Female Hypertension Diabetes Smoking Prior MI Prior PCI Prior CABG Prior TIA Prior stroke STEMI (288) n (%) 56.7±13.3 61 (21) 145 (50) 152 (53) 164 (57) 41 (14) 25 (9) 7 (2) 7 (2) 19 (7) Pooled analysis of the short-term results from 23 randomized trials comparing primary PCI and fibrinolytic therapy in 7739 patients Stone G. Circulation 2008;118:538-551 Primary PCI Recommendations Class Level Indications for primary PCI Primary PCI is the recommended reperfusion therapy over fibrinolysis if performed by an experienced team within 120 min of FMC Primary PCI is indicated for patients with severe acute heart failure or cardiogenic shock, unless the expected PCI related delay is excessive and the patient presents early after symptom onset. I A I B Steg et al, EHJ 2012;33:2569-2619 Periprocedural antithrombotic medications in primary PCI Recommendations Class Level Aspirin oral or i.v. (if unable to swallow) is recommended I B An ADP- receptor blocker is recommended in addition to aspirin. Option are: I A • Prasugrel in clopidogrel-naive patients, if no history of prior stroke/TIA, age <75 years. I B • Ticagrelor I B • Clopidogrel, preferably when prasugrel or ticagrelor are either not available or contraindicated I C Antiplatelet therapy Steg et al, EHJ 2012;33:2569-2619 Fibrinolytic therapy Recommendations Class Level I A In patient presenting early (<2 h after symptom onset ) with large infarct and low bleeding risk, fibrinolysis should be considered if time from FMC to balloon inflation is >90 min IIa B If possible, fibrinolysis should start in the Prehospital setting IIa A A fibrin – specific agent (tenecteplase, alteplase, reteplase) is recommended ( over non – fibrin specific agents) I B Oral or i.v. aspirin must be administered I B Clopidogrel is indicated in addition to aspirin I A Fibrinolytic therapy is recommended within 12 h of symptom onset in patients without contraindications if primary PCI cannot be performed by an experienced team within 120 min of FMC Steg et al, EHJ 2012;33:2569-2619 PCI post lysis Recommendations Class Level I A Rescue PCI is indicated immediately when fibrinolysis has failed (< 50% ST- segment resolution at 60 min). I A Emergency PCI is indicated in the case of recurrent ischemia or evidence of reocclusion after initial successful fibrinolysis. I B Transfer to a PCI capable center following fibrinolysis Is indicated in all patients after fibrinolysis Interventions following fibrinolysis Steg et al, EHJ 2012;33:2569-2619 Prehospital and in-hospital management Reperfusion stratergies within 24 h of FMC STEMI diagnosis Primary PCI capable center EMS or non primary-PCI capable center Preferably < 60 min PCI possible <120 min? Immediate transfer to PCI center Primary - PCI Rescue PCI Immediately Yes Preferably ≤ 90 min (≤ 60 min in early presenters) Immediate transfer to PCI center No Preferably ≤ 30 min No Yes Successful fibrinolysis Immediate fibrinolysis Preferably 3-24 h Coronary angiography Steg et al, EHJ 2012;33:2569-2619 Important treatment goals in the management of STEMI Stages Target Preferred for FMC to ECG and diagnosis ≤ 10 min Preferred for FMC to fibrinolysis (FMC to needle) ≤ 30 min Preferred for FMC to primary PCI (door to balloon) in primary PCI hospitals ≤ 60 min Preferred for FMC to primary PCI in hospitals without cath facility ≤ 90 min (≤ 60 min if early presenter with large area at risk) if this target cannot be met, consider fibrinolysis Acceptable for primary PCI rather than fibrinolysis ≤ 120 min (≤ 90 min if early presenter with large area at risk) if this target cannot be met, consider fibrinolysis Preferred for successful fibrinolysis to angiography 3-24 hours Steg et al, EHJ 2012;33:2569-2619 Components of delay in STEMI Symptom onset FMC Reperfusion therapy System delay Time to reperfusion therapy Wire passage in culprit artery (primary PCI) Steg et al, EHJ 2012;33:2569-2619 ………..………………................. ≤ 10 min ………..………………... ………..……………….... ………..………………......... Patient delay Diagnosis Start of lysis Reperfusion in eligible patients Per country Kuwait Oman UAE Bahrain (n=259) (n= 315) (n= 129) (n= 119) 40 29 49 58 11 13 PPCI (%) 6 0.3 Lysis (%) 86 92 Shortfall (%) 8 7.7 Reperfusion in eligible patients Kuwait Adan Hospital Rest of Hospital (n=56) (n= 203) PPCI (%) 27 0 Lysis (%) 64 93 Shortfall (%) 9 7 Was reperfusion administered in time? Reperfusion Timeline Thrombolysis in Kuwait Thrombolysis Adan Hospital Rest of Hospital (n=37) (n= 188) Median D2NT (min) 34 41 D2NT ≤30 min (%) 43 36 Primary PCI experience Adan Hospital November 13 – December 30, 2013 Distribution of timeline Primary PCI experience Adan Hospital November 13 – December 30, 2013 Distribution of timeline during and after normal working hours During working hours 14 patients After working hours 45 patients Door to ECG 5 7 ECG to cardiology notification 11 6 Cardiology response time 4 3 Door to balloon time 51 62 Door to balloon ≤60 minutes 71% 53% Door to balloon ≤90 minutes 93% 89% Primary PCI experience Mubarak Alkabeer Hospital November 13 – December 30, 2013 Held off for two weeks in the middle Distribution of timeline Primary PCI experience MKH vs. Adan Hospital November 13 – December 30, 2013 Distribution of timeline (values in mean) Adan (33 patients) MKH (24 patients) 205 124 Door to ECG 7 18 ECG to cardiology notification 9 20 Cardiology response time 4 3 Door to balloon time 64 111 Door to balloon ≤60 minutes 48% 0 Door to balloon ≤90 minutes 85% 15% Door to balloon ≤120 minutes 97% 65% Symptom onset to ER arrival Components of delay in STEMI Symptom onset FMC Reperfusion therapy System delay Time to reperfusion therapy Wire passage in culprit artery (primary PCI) Steg et al, EHJ 2012;33:2569-2619 ………..………………................. ≤ 10 min ………..………………... ………..……………….... ………..………………......... Patient delay Diagnosis Start of lysis Door to balloon in hospitals with and without cath labs in Kuwait Adan Hospital ECG to Cardiology Door to ECG Cardiology response time 9 7 Door to balloon 64 4 Mubarak AlKabeer Hospital Door to ECG 18 ECG to Cardiology 20 Cardiology response time 3 Door to balloon 5 Ambulance notification 13 Ambulance response 30 Ambulance trip time 111 In-hospital cardiac catheterization Prehospital and in-hospital management Reperfusion stratergies within 24 h of FMC STEMI diagnosis Primary- PCI capable center EMS or non primary-PCI capable center Preferably < 60 min PCI possible <120 min? Immediate transfer to PCI center Primary - PCI Rescue PCI Immediately Yes Preferably ≤ 90 min (≤ 60 min in early presenters) Immediate transfer to PCI center No Preferably ≤ 30 min No Yes Successful fibrinolysis Immediate fibrinolysis Preferably 3-24 h Coronary angiography Steg et al, EHJ 2012;33:2569-2619 PCI post lysis Recommendations Class Level I A Rescue PCI is indicated immediately when fibrinolysis has failed (< 50% ST- segment resolution at 60 min). I A Emergency PCI is indicated in the case of recurrent ischemia or evidence of reocclusion after initial successful fibrinolysis. I B Transfer to a PCI capable center following fibrinolysis Is indicated in all patient after fibrinolysis Interventions following fibrinolysis Steg et al, EHJ 2012;33:2569-2619 Kuwait Gulf COAST population Rates of inhospital cath for STEMI patients Cath during hospital stay STEMI (288) n (%) 120 (42) Adan Hospital 61 (87) The rest of hospitals 59 (27) Hospital arrival to PCI at Adan, Mean±SD, Median (days) Hospital arrival to PCI excluding Adan, Mean±SD, Median (days) 0.86±1.2, 0.00 4.4±3.5, 3 Management of hyperglycemia in the acute phase of STEMI Recommendations Class Level Measurement of glycaemia is indicated at initial evaluation in all patients, and should be repeated in patients with know diabetes or hyperglycemia I C Plans for optimal outpatient glucose control and secondary prevention must be determined in patients with diabetes before discharge I C The goals of glucose control in the acute phase should be to maintain glucose concentrations ≤11.0 mmol/L (200mg/dL) while avoiding fall of glycaemia<5 mmol/L (<90mg/dL). In some patients, this may require a dose-adjusted insulin infusion with monitoring of glucose, as long as hypoglycemia is avoided IIa B A measurement of fasting glucose and HbA1c and , in some cases, a post- discharge oral glucose tolerance test should be considered in patients with hyperglycemia but without a history of diabetes IIa B Routine glucose-insulin-potassium infusion is not indicated III A Steg et al, EHJ 2012;33:2569-2619 Routine therapies in the acute, subacute and long term phase of STEMI Recommendations Class Level IIa B Oral treatment with betablockers is indicated in patients with heart failure or LV dysfunction I A A fasting lipid profile must be obtained in all STEMI patients, as soon as possible after presentation I C I A IIa C Oral treatment with betablockers should be considered during hospital stay and continued thereafter in all STEMI patients without contraindications It is recommended to initiate or continue high dose statins early after admission in all STEMI patients without contraindication or history of intolerance, regardless of initial cholesterol values Reassessment of LDL should be considered after 4-6 weeks to ensure that a target value of ≤1.8 mmol/L (70 mg/dL) has been reached Steg et al, EHJ 2012;33:2569-2619 Routine therapies in the acute, subacute and long term phase of STEMI Recommendations ACE Inhibitors are indicated starting within the first 24 h of STEMI in patients with evidence of heart failure, LV systolic dysfunction, diabetes or an anterior infarct An ARB, preferably valsartan, is an alternative to ACE inhibitors in patient with heart failure or LV systolic dysfunction, particularly those who are intolerant to ACE inhibitors ACE inhibitor should be considered in all patients in the absence of contraindications Aldosterone antagonists are indicated in patients with an ejection fraction ≤40% and heart failure or diabetes, provided no renal failure or hyperkalaemia Class Level I A I B IIa A I B Steg et al, EHJ 2012;33:2569-2619 Adherence to medical therapy Gulf COAST STEMI/NSTEMI Gulf COAST 2012 Gulf RACE 2007¹ EHS-ACS-II 2004² NRMI-5 2004-2006³ Aspirin at arrival (%) 99 98 97 90 Aspirin prescribed at discharge (%) 97 97 90 91 Beta- blocker at discharge (%) 85 78 71 89 Statin at discharge (%) 97 84 80 82 Clopidogrel at discharge for medically treated AMI patients (%) 67 57 63 - From plaque formation to progression to clinical manifestations Plaque formation Risk factor Clinical manifestations Slow progression Atherosclerosis Accelerated Progression Atherothrombosis STABLE No symptoms Silent ischemia Stable angina UNSTABLE Unstable angina NSTEMI STEMI Sudden cardiac death Work up of ischemic chest pain Chest Pain Admission Working diagnosis ECG Acute Coronary Syndrome Persistent ST-elevation troponin rise/fall Bio-chemistry Diagnosis Hamm et al, EHJ 2011;32:2999-3054 ST/T– abnormalities STEMI NSTEMI normal or undetermined ECG troponin normal Unstable Angina Criteria for high risk with indication for invasive management Primary • Relevant rise or fall in troponin • Dynamic ST- or T- wave changes (symptomatic or silent) Secondary • • • • • • • Diabetes mellitus Renal insufficiency (eGFR < 60 mL/min/1.73m2) Reduced LV function (ejection fraction < 40 %) Early post infarction angina Recent PCI Prior CABG Intermediate to high GRACE risk score Hamm et al, EHJ 2011;32:2999-3054 Gulf COAST Kuwait population Age (Mean ±SD) Female Hypertension Diabetes Smoking Prior MI Prior PCI Prior CABG Prior TIA Prior stroke NSTEMI (574) n (%) 61.7±12.3 221 (39) 403 (70) 391 (68) 177 (31) 208 (36) 120 (21) 45 (8) 28 (5) 57 (10) Decision – making algorithm in ACS 1.Clinical Evaluation 2. Diagnosis/Risk Assessment STEMI reperfusion urgent < 120 min Evaluation • • • • 3. Coronary angiography Validation • Quality of chest pain. Symptom - orientated physical examination. Short history for the likelihood of CAD. Electrocardiogram (ST elevation?) ACS possible • • • • • • Response to antianginal treatment. Biochemistry/troponin. ECG Echocardiogram. Calculated risk score (GRACE) Risk Criteria. Optional: CT, MRI, scintigraphy. early <24h <72h No CAD no/elective Hamm et al, EHJ 2011;32:2999-3054 Antithrombotic treatment in NSTE ACS Targets for antithrombics Anticoagulation Tissue Factor Collagen Antiplatelet Aspirin Plasma clotting cascade Fondaparinux ADP Thromboxane A2 Prothrombin LMWH Heparin AT Factor Xa Conformational activation of GPIIb/IIIa AT GPIIb/IIIa inhibitors Thrombin Platelet aggregation Bivalirudin Fibrinogen Fibrin Thrombus Hamm et al, EHJ 2011;32:2999-3054 Clopidogrel Prasugrel Ticagrelor Conclusions Management of ACS has evolved rapidly over the past few years. Early risk stratification and cardiac catheterization is a cornerstone in ACS management. If we want to benefit our patients, it is important that we examine what we do. Our ACS patients receive good medical therapy at discharge from hospital. However, we rely heavily on lytic therapy for reperfusion in STEMI and it is not administered in efficient timing to get the most benefit from it. In both STEMI and NSTE ACS, our use of cardiac catheterization falls short of guidelines recommendations.