4 weeks
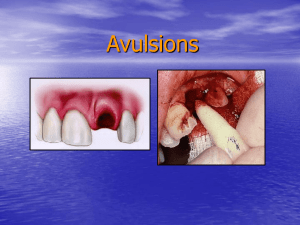
advertisement

Traumatic Injuries, Cracked Teeth and vertical root fractures (VRF) Fact Most dental trauma occurs in 7_12 age range And most trauma occurs in the anterior region of the mouth, maxilla>mandible 1. Crown FX without Pulp exposure NO PROBLEM, RELAX AND RESTORE Complicated Crown FX with Pulp Exposure @80% IF w/in 24hrs Pulp Cap? Partial Pulpotomy@95% Full pulpotomy @75% OR: EXTIRPATION if root is fully formed 2. Crown-Root Fracture sometimes fractures at an angle Angular Fracture: Is this restorable? Remember, In all trauma, the primary purpose of our treatment is to keep the pulp vital, if at all possible, ESPECIALLY if apex is open WHY? Pulpotomy – Immature Apex If Vital = “Apexogenesis”* Apexogenesis vs Apexification Dealing with the immature root Apexogenesis (Vital Pulp) best to treat w pulpotomy. The idea is to allow the vital pulp to remain vital and complete the development of the root apex as well as thickening of the RC walls RCT maybe needed later BUT not if tooth remains asymptomatic AND vital Apexification (Necrotic Pulp) Hoping to get closure of the apex (& there is NO wall thickening) to be able to later do a proper RC seal via obturation. CaOH + time is proper tx over 3-18mo RCT ALWAYS NEEDED HERE* and is less predictable due to thinner walls Object of either treatment is to allow for roofing over of apex and allow RCT to be done at a later date. And now, Regeneration? Revascularization of immature permanent teeth utilizing a mixture of antibiotics(3 weeks), creating a blood clot w/in the RCS which produces development of the tooth structure 3.Horizontal Root Fracture Root FX (Horizontal) What do you do here? Try to reposition and splint 2-4 wks, check for vitality q 30 days 4. Luxation Injuries (MOST COMMON OF ALL DENTAL INJURIES) 30-44% Concussion Subluxation Extrusion Lateral Intrusion AVULSION WORST CASE SEQUELAE? PULP NECROSIS EXTERNAL/INTERNAL ROOT RESORPTION Possible tooth loss Concussion Luxation Injury Least severe of Luxation injuries No displacement of tooth nor excessive mobility Tooth tender to touch “Bruised PDL” No radiographic abnormalities Assess vitality in 4 wks Subluxation Luxation Injury Tooth tender to touch & slightly mobile (1+) but not displaced Possible hemorrhage from gingival crevice No radiographic abnormalities Damage to supporting structures? Assess vitality in 4 weeks Extrusion Luxation Injury Elongated mobile tooth Cl. II mobility or greater Radiographs show increased apical periodontal space Manually reposition Reposition tooth + Flexible splint (2 weeks) Assess vitality in 4 weeks What is a flexible splint? -Allows physiologic movement of the teeth in order to minimize ankylosis -In the past, .028 gauge ortho wire bonded to tooth for 7-10 days unless alveolar FX had occurred. Then 4-8 wks OR: 4-6# fishing line bonded to teeth -Currently, titanium trauma splint (TTS) is recommended Semi-rigid or flexible splinting Experimental studies in non-human primates have demonstrated that rigid splinting ,especially for prolonged periods, leads to ankylosis &/or external resorption. Maintaining a slight degree of tooth mobility appears to be beneficial to PDL healing Titanium Trauma Splint Medaris AG, Basel Switzerland TTS splint Insert picture of same Splinting of traumatized teeth with a new device:TTS (Titanium Trauma Splint) Medartis AG, Basel, Switzerland Von arx T, etal Dent Traumatol, ’01;17:180-84 Lateral Luxation Injury Displaced laterally & often locked in bone Not tender to touch, not mobile Alveolus fractured Percussion test: high metallic sound (ankylosis) Increased PDL space best seen on eccentric or occlusal radiographs Anesthetize & reposition + Flexible splint (4 weeks) Assess vitality in 4 weeks Intrusion Luxation Injury External root resorption likely Most severe of luxations*** Tooth appears shorter: displaced into alveolar bone PDL destruction/alveolar crushing) Beware of ankylosis/resorption/ pulp necrosis is all but certain in mature teeth*** Not tender to touch, not mobile Percussion test: high metallic sound Radiographs not always conclusive Slightly luxate with forceps or band and move orthodontically. Splinting is not usually necessary (>4 weeks) Tooth with open apex may spontaneously re-erupt. Treatment of intrusion luxation Closed apex needs ortho. or surgical repositioning and probable RCT in 1-3 weeks In all LUXATION and especially INTRUSION injuries, the apical neurovascular bundle and attachment apparatus will be affected to some degree>>>loss of vitality & internal/external resorption 5. Avulsion Tooth is knocked completely out of mouth Viability of the PDL must be preserved for success Extra-oral dry time is CRITICAL 3060”*** Must be replaced in socket ASAP (15-20”) in order to.. Prevent ankylosis Prevent external root resorption To replant or not? should be “decent tooth”: No point in replanting THIS one Replant? TX is aimed at minimizing the inflammation from the two main consequences of avulsion, namely; attachment damage and pulpal infection that inevitably results The SINGLE most VIP factor in achieving a favorable outcome is the SPEED at which a clean tooth is properly replanted Keeping the attached PDL moist is VIP!!* Replantation guidelines HOW FAST IS FAST? 5”, 30” 60”, TAKE YOUR PICK, it depends on whose book you read! If tooth is out of the mouth less than 15-20”, replant according to guidelines If tooth was out and placed in cold milk or other physiological solution w/in 15-20” & available for replantation w/in 30”, replant and follow guidelines If tooth is out > 60” and not stored, there is usually one outcome: resorption and probable loss If the pt is pre adolescent, the tooth may become infraoccluded (ankylosed) as he/she grows older To replant or not If the root of the avulsed tooth is not completely formed, the prognosis for survival and revascularization is possible if not left out>60” If root is incompletely formed and replantation is rapid, vitality may be maintained but is not predictable First Aid Instructions Handle by crown only Pick off debris with tweezers Replant tooth if possible _________________________________ If not, transport in appropriate medium: “HBSS (Hank’s Balanced Salt solution) OR “Via Span” (if available) OR milk if above not available OR place in vestibule (saliva) & Report to dental office ASAP Once in Dental office: Take films to make sure there is no alveolar FX & that adjacent teeth are OK “Save-a-tooth” (Hank’s Balanced Salt solution) OR “Via Span”, milk, saline Gently clean socket Replant and check occlusion Splint (7-10 days) RX antibiotics Avulsion Injury What NOT to do! Do Not Handle by root Scrub root Allow tooth to dry Submerge the tooth in water (tap water is hypotonic> and will cause cell rupture) AAE has a Flow Chart Outlining Current Treatment Management Protocols of both Luxation and Avulsion cases ..www. aae.org. If over 60” “dry time” Remove remnants ofPDL by soaking in acid for 1” Soak in Stannous Fl for 5” No harm done to go ahead and complete endo ASAP Splint Immature Tooth: Open Apex, revascularization is possible if out less than 30-60” Replant as above EXCEPT different Soak tooth in Doxycycline (1mg/20cc saline)<replantation for 5” Monitor pulp vitality closely (q 30 d or until root development is confirmed) Vital Open apex will NOT necessarily require RCT UNLESS pulp becomes necrotic. What if it does? Do we do apexogenesis then? Ankylosis A problem following trauma and long term rigid splinting Tooth is solidly fixed and has a high metallic ring when percussing. Does not erupt with other teeth May lead to massive external resorption & loss of tooth Internal= appearance of “aneurysm” w/in canal. Complications with Replanted avulsed teeth & Possibly with Rigid Long-Term Splinting Ankylosis (Replacement Resorption) Vertical Root Fracture Look for ‘J’-Shaped apical lesion Look for Drop-off Pocket if . . . . VRF difficult to confirm radiographically –UNLESS separation of segments occurs Transillumination Restoration Removal + Staining Other methods of discovering VERTICAL ROOT FRACTURE A surgical exploration is usually the only other way to confirm presence of VRF* Flare-ups Flare-ups A flare-up is an acute exacerbation of an asymptomatic pulp/or periapical pathosis after the initiation or continuation of root canal treatment. Patient Presentation Pain Pain and swelling Factors Mechanical chemical Emotional state Gender Microbial • Immunological • Psychological • state Regulation of periapical inflammation Incidence 1.4 to 19% 20 to 40% Age of Patient? There is a lack of agreement concerning the influence of age on the incidence of flare-up. 40_59 year(most) Under the age of 20(least) Gender and Flare-ups Women(most) Systemic conditions Host resistance Allergy Anatomic Location Mandibular teeth premolars Anxiety Preoperative History of the Tooth Number of Treatment Visits Causes of Inter-Appointment Pain Mechanical Chemical Microbial injury Re-Treatment Cases 13.6% flare-up Strategies to Prevent Flare-ups Anxiety Reduction Behavioral Intervention Occlusal Reduction Pharmacologic Strategies for Flare-up Antibiotic NSAIDs and Acetaminophen Long-acting Local Anesthetics Patient Instructions By the Clock NOT PRN Indications for Antibiotic Therapy Systemic involvement Compromised host resistance Fascial space involvement Treatment of Endodontic Flareups Diagnosis and Definitive Treatment Drainage Through the Coronal Access Opening I&D Instrumentation Trephination( For severe pain without visible swelling)