Acute apical periodontitis
advertisement

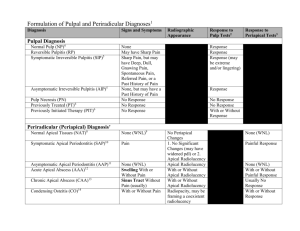
Acute apical periodontitis (parodontitis apicalis acuta) (etiology, calssification, clinical features, dg., diff. Dg. ) Definition of Periapical Disease Periapical diseases are ´´an inflammatory conditions occuring around the apex of a tooth caused by a necrotic pulp´´ Inflammation around a root end is known as ´´apical periodontitis´´ Structures around the apical foramen constitute the ´´periapical region´´ Structures surrounding the apex of tooth roots are known collectively as the ´´periapical tissues´´, they consist of the periodontal ligament and the alveolar bone. Lesions produced by periapical infection are in close proximity to the apices of the teeth. Periapical lesions are recognized by their radiographic appearance and the symptoms they produce. Etiology of Periapical Disease Most periapical diseases are caused by dead pulps. Most, but not all, pulpal disease is caused by bacterial invasion from dental caries or, less commonly, cracked teeth. The remainder are caused by non-bacterial pulpal deaths caused, for example trauma. The products of bacterial invasion and pulp necrosis initiate most periapical diseases. Clinical Features of Periapical Disease The signs and symptoms of periapical disease are related to inflammation Being inflammatory in origin, periapical diseases manifest with the signs and symptoms of acute or chronic inflammation. However, there is no consistent relationship between patient´s symptoms and histologic findings. Radiographic Features of Periapical Disease Most periapical lesions manifest as sharply-defined radiolucencies. Most, but not all, periapical lesions destroy bone around the tooth apex resulting in radiolucent defects on radiographic examination of the area. Because it takes several days for enough bone destruction to produce a radiolucent lesion, the earliest periapical lesions may not be detected in a radiograph. The more long-lived ones will cause enough bone destruction to produce a radiolucency that can be easily detected in a radiograph. As will be seen, most periapical lesion are small and well- circumscribed. It is uncommon for these lesions to become large, to spread, or to break through the surrounding cortical bony plates Acute Apical Periodontitis Acute Inflammatory Periapical Diseases A common condition accompanied by excruciating pain, a necrotic pulp, and radiographic thickening of the apical periodontal ligament space, treatment requires pulp extirpation or tooth extraction. Acute inflammation may extend into the periapical tissues Excruciating is associated with acute pulpitis, it is also associated with extension of the acute inflammatory process into the periapical tissues creating acute apical periodontitis While bacterial infection and necrotic pulp are responsible for the onset of most cases of AAP, it may also be a complication of initial endodontic therapy. In these cases, machanical cleansing of the root cannals forces irritating debris into the periapical tissues initiating an acute inflammatory response there . Pain is the presenting symptom, it may be provoked by percussion. The patient may also sense that the affected tooth is higher than nearby ones. Often the pain is so diffuse that the patient cannot localize it. The dentist can usually locate the offending tooth by the crude but effective technique of tapping (percussion) on one tooth after another until the patient experiances pain. Extension of the acute inflammatory response into the periodontal ligament explains both tooth elevation and tappinginduced pain Usually there are very few radiographic features accompanying acute apical periodontitis AAP arises so quickly, probably within an hour or two, that bone destruction and its resulting radiographic changes may not be evident. Sometimes, however, widened periodontal ligament around the apex may produce a radiolucent thickening there. Microscopic features include a localized acute inflammatory exudate with dilated capillaries, and neutrophils The pulp will die making extirpation or extraction necessary Since the source of AAP is a necrotic pulp, it follows that pulp extirpation or extraction is the appropriate therapy for it. If the lesion resulted from endodontic therapy, the endodontist will usually reopen the canal to allow drainage or, if the canal filling has been completed, enter the periapical area surgically to debride the region APICAL PERIODNTITIS Inflammation of periapical region Causes: 1, Trauma-direct blow to the tooth 2, Chemicals- Passage of chemical irritants through the apical foramen during the use of drugs in treatment of deep cavities, and pulp lesions 3, Bacterial toxins, bacterial infections-in dental caries, pulp lesions. The response to apical irritans can be acute or chronic1. Most commonly balance between body resistance and noxious agent–granuloma formation. 2. noxious stimuli or ↓ body resistance– suppurative apical periodontitis 3. chronic lesion may develop apical cyst. Acute Apical Periodontitis Aetiology: Pulp disease (deep caries), bacterial toxins, bacterial irritations-passage of instruments beyond the canal which may push some irritants as necrotic, pulp tissue, bacteria, or dentine fragments into periodontal ligament. Stages 1. Periodontal stage hyperemia of blood vessels and oedema in periodontium 2. Endosseus stage the bone is envolved first by hyperemia of vessels then by leukocytic infiltration and finally by pus formation 3. Subperiostal stage pus beneath the periosteum-subperiostal abscess 4. Submucous stage pus in soft tissuesubmucous abscess Clinical features Generally- Rapid onset, acute pain, tooth sensitive to touch, massive swelling. Periodontal stage- the tooth is painful to touch by eating, bite slightfeeling of elevated tooth in the socket Endosseous stage- intensive pain, constant, throbbing, pressing pain. Patient wants to extract the tooth, strong feeling of elevated tooth Subperiosteal stage- throbbing pain increasing in intensity, the tooth is extremly sensitive to touch, swelling area is sensitive Submucous stage- decrease of painful symptoms Diagnosis: History (painful symptoms) sensitivity to touch, tooth in supraocclusion, face asymetry due to swelling, lymph node involvement, tenderness to percussion, pyrexia X-ray: vary from widen periodontal space to a large alveolar radiolucency. Differential diagnosis Acute serous and purulent pulpitis, abscess Apical Abscess Acute pulpal-periapical inflammation may enlarge into an abscess Pain associated with AAP is sufficient to require the patient to seek dental care. It is also usually the case that the patients defenses are capable of localizing the infection to the periapical region The acute inflammatory reaction may enlarge forming an abscess (apical abscess, dento-alveolar abscess) Abscesses are caused by virulent organisms and decreased immunologic rsponses Apical abscesses are caused by necrotic pulps. Abscess formation suggests that the microorganism responsible is virulent or the patients immunologic defenses are impaired Apical abscesses are painful Fever, leukocytosis, and neutrophilia are commonly present. As the lesion enlarges, it may penetrate the buccal or lingual cortical plates and expand into the surrounding soft tissues. Such extension may include the floor of the mouth, the palate, the face, and the neck. Soft tissue extension will show the usual features of acute inflammation: redness, swelling and warmth Unless a dentist intervenes, the abscess will drain spontaneously exuding a purulent exudate. A tooth abscess is normally not seeable, except as a lump - sometimes - as the tooth abscess exists under the skin and can only be seen, as such, by X-rays. Sometimes you may see a picture of a face with part of it swollen, again you are seeing the swelling under the skin, not actually seeing the tooth abscess as such - some of the swellings can be through the lymph glands trying to take the infection caused by the tooth abscess. On X-ray, the tooth abscess can be seen by a trained eye. Most pictures of a tooth abscess simply show a drawing of a tooth, a cavity leading into the soft pulp, and a colored area denoting the infection Acute tooth abscess: Characterized by rapid, painful onset. Sleep and overall function may be disturbed due to symptoms involved. Swelling of gum tissue and surrounding areas my be present. It can be very difficult to find relief during the painful peak of a tooth abscess. Daily activities are often interrupted during this time Any abscessed tooth has the potential to become a life threatening situation. Infection of a tooth in the lower jaw can cause swelling of the check and under the jaw bone. If the swelling under the jaw becomes too advanced, swallowing and breathing can become critically impaired (Ludwig's Angina). An infection of a top tooth may produce swelling in the check, side of the temple or under the eye. The gradual closing of the eye due to swelling and infection represents a dire situation (Cavernous Sinus Thrombosis). Abscesses may not be detected with radiographs, they are composed of acute inflammation An apical abscess, like AAP, arises suddenly so there is little radiographic change. If the lesion has been present long enough, however, a faint, diffuse radiolucency may be evident. Abscesses are composed of an intense acute inflammatory reaction. In addition to the usual features of acute inflammation, immature neutrophils (band cells) are likely to be seen, dead and dying neutrophils and necrotic debris (suppuration) are also prominent. Establishing drainage and proper antimicrobial therapy will cure most abscesses In the absence of significant radiographic changes, the dentist must rely on clinical features to arrive at a proper diagnosis (pain, systemic features, suppuration) Once the presence of an apical abscess is suspected , vigorous treatment must be pursued. First, the source of the acute inflammatory response must be identified and eliminated. Second, a bacterial culture of exudate must be obtained and submitted to a laboratory for the purpose of identifying the offending microorganism and determine the antibiotic most effective in killing it (culture and sensitivity test) Finnaly, the dentist should prescribe an ATB. If the abscess has spread into the surrounding soft tissues, an incision and hrainage should be performed. This procedure provides a source of exudate for culture and sensitivity testing, and, allows for the removal of suppuration so that repair will follow. Acute Osteomyelitis The main reason for treating apical abscesses with vigor is to prevent spread along the bone marrow spaces causing a condition known as osteomyelitis. Ost. Is a very serious condition that can cause destruction of large sections of jaw and be difficult to cure. Ost. May be the inevitable result of untreated pulpal or periapical infection. Almost always, bacterial infection is involved. Ost. More commonly affects the mandible than the maxilla. Probably the maxillas excellent blood supply is the difference. There is usually malaise (discomfort), pain, fever, and leukocytosis. There may be swelling of the mandible and suppurative drainage into the oral cavity Because the Ost. Takes longer to develop than other acute inflammatory lesions, usually there are significant and specific radiographic changes. These include involvement of bone away from the periapical region, indistinct outline (diffuse growth pattern) and combination of radiolucencies and radiopacities (mottled radiographic apperarance) Microscopically shows bone destruction (osteoclasts) and bone deposition (osteoblasts) proceeding side by side. So, it is in bone: Inflammation induced bone resorption and bone repair may proceed simultaneously. It is this reaction that produces the mottled radiographic features of Ost.