Amenorrhea UNC School of Medicine Obstetrics and Gynecology Clerkship Case Based Seminar Series
advertisement

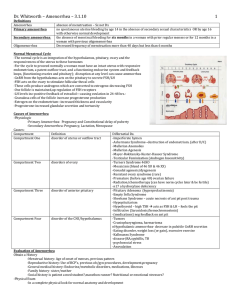
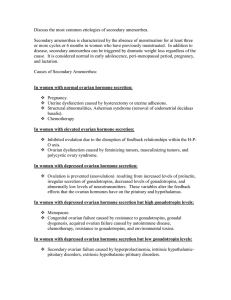
Amenorrhea UNC School of Medicine Obstetrics and Gynecology Clerkship Case Based Seminar Series Objectives for Amenorrhea Define amenorrhea and oligomenorrhea Explain the pathophysiology and identify the etiologies of amenorrhea and oligomenorrhea Describe the symptoms and physical examination findings of amenorrhea and oligomenorrhea Discuss the steps in the evaluation and management of amenorrhea and oligomenorrhea Describe the consequences of untreated amenorrhea and oligomenorrhea Definition Amenorrhea – absence of menses Primary amenorrhea – absence of menarche Absence of menarche by age 14 without secondary sexual characteristics Absence of menarche by age 16 with secondary sexual characteristics Secondary amenorrhea – absence of menses in a previously menstruating woman Absence of menses for > 6 months or duration of 3 menstrual cycles Oligomenorrhea – reduction in frequency of menses Cycle lengths > 35 days, but < 6 months Primary Amenorrhea: Etiology Pregnancy Thyroid disease Hyperprolactinemia Prolactinoma Hypergonadotropic hypogonadism Gonadal dysgenesis (i.e. Turner syndrome) Premature ovarian failure Hypogonadotropic hypogonadism Constitutional delay of puberty Congenital GnRH deficiency (Kallman syndrome) Functional hypothalamic amenorrhea (i.e. Anorexia or Bulimia nervosa) CNS tumor (i.e. Craniopharyngioma) Normogonadotropic Congenital (i.e. Mullerian agenesis, Androgen Insensitivity syndrome) Outflow tract obstruction (i.e. Imperforate hymen, Transverse vaginal septum) Hyperandrogenic anovulation (i.e. PCOS, Cushing’s disease) Primary Amenorrhea: Etiology Most common etiologies: Chromosomal abnormalities causing gonadal dysgenesis – 50% Hypothalamic hypogonadism – 20% Absence of the uterus, cervix, or vagina – 15% Transverse vaginal septum or imperforate hymen – 5% Pituitary disease – 5% Primary Amenorrhea: History Findings Association Completion of stages of puberty? Development of axillary and pubic hair? Breast development? Ovarian or pituitary failure Chromosomal abnormality Family history of delayed or absent puberty? Familial disorder Constitutional delay of puberty Height relative to family members? Turner’s syndrome Symptoms of virilization? PCOS Ovarian or adrenal tumor Presence of Y chromosome Recent stress? Change in weight, diet, or exercise? Functional hypothalamic amenorrhea Medications (i.e. antidepressants, antipsychotics)? Hyperprolactinemia Galactorrhea? Hyperprolactinemia Headaches, visual field defects, fatigue, polyuria or polydipsia? Hypothalamic-pituitary disease Primary Amenorrhea: Physical Exam Evaluation of pubertal development (height, weight) and growth chart Breast development (Tanner staging) Evaluation for features of Turner’s syndrome Webbed neck, low hair line, shield chest, widely spaced nipples Examine skin for hirsutism, acne, striae, increased pigmentation, and vitiligo Pelvic exam Clitoral size Intactness of hymen Depth of vagina Presence of vaginal septum Presence of cervix, uterus, and ovaries Tanner Stages Stage 1: Prepubertal, no palpable breast tissue or pubic hair. Stage 2: Development of breast bud; sparse, straight pubic hair. Stage 3: Enlargement of breast; pubic hair darker, coarser, and curlier. Stage 4: Areola and papilla project above the breast; pubic hair adult-like in appearance. Stage 5: Recession of areola to match contour of breast; pubic hair extends to thigh. Figure from: Roede, MJ, van Wieringen, JC. Growth diagrams 1980: Netherlands third nation-wide survey. Tijdschr Soc Gezondheids 1985; 63:1. Reproduced with permission from the author. Primary Amenorrhea: Evaluation Secondary sexual characteristics present? No Yes Measure FSH Perform ultrasound of uterus Uterus absent or abnormal FSH < 5 FSH > 20 Hypogonadotropic hypogonadism Hypergonadotropic hypogonadism Hypothalamic amenorrhea Constitutional delay Karyotype of puberty Kallman syndrome CNS tumor 46,XX Premature ovarian failure Uterus present or normal Karyotype analysis Outflow obstruction analysis 46,XY 46,XX No Yes Androgen insensitivity syndrome Müllerian agenesis Evaluate for 2° amenorrhea Imperforate hymen Transverse vaginal septum 45,XO Turner’s syndrome PCOS Cushing’s Secondary Amenorrhea/Oligomenorrhea: Etiology Pregnancy Thyroid disease Hyperprolactinemia Prolactinoma Breastfeeding, Breast stimulation Medication (i.e. Antipsychotics, Antidepressants) Hypergonadotropic hypogonadism Postmenopausal ovarian failure Premature ovarian failure Hypogonadotropic hypogonadism Functional hypothalamic amenorrhea (i.e. Anorexia or Bulimia nervosa) CNS tumor (i.e. Craniopharyngioma) Sheehan’s syndrome Chronic illness Normogonadotropic Outflow tract obstruction (i.e. Asherman’s syndrome, Cervical stenosis) Hyperandrogenic anovulation (i.e. PCOS, Cushing’s disease, CAH) Secondary Amenorrhea/Oligomenorrhea: Etiology Most common etiologies: Ovarian disease – 40% Hypothalamic dysfunction – 35% Pituitary disease – 19% Uterine disease – 5% Other – 1% Secondary Amenorrhea/Oligomenorrhea: History Findings Association Recent stress? Change in weight, diet, or exercise? Functional hypothalamic amenorrhea Development of acne, hirsutism, striae, central obesity, PCOS increased skin pigmentation or deepening voice? Cushing’s disease Ovarian or adrenal tumor Medications (i.e. antidepressants, antipsychotics)? Hyperprolactinemia Chronic illness? Functional hypothalamic amenorrhea Headaches, visual field defects, fatigue, polyuria or polydipsia? Hypothalamic-pituitary disease Symptoms of estrogen deficiency (hot flashes, vaginal dryness, decreased libido, or poor sleep)? Premature ovarian failure Postmenopausal ovarian failure Galactorrhea? Hyperprolactinemia History of obstetrical catastrophe, severe bleeding, D&C, endometritis, or other infection? Sheehan’s syndrome Asherman’s syndrome Secondary Amenorrhea/Oligomenorrhea: Physical Exam General Evaluation of height, weight, and BMI Examine skin for hirsutism, acne, striae, acanthosis nigricans, thickness or thinness, and easy bruisability Thyroid exam Breast exam Express for galactorrhea Pelvic exam Atrophy Vaginal dryness Secondary Amenorrhea/Oligomenorrhea: Evaluation Negative urine pregnancy test Check TSH and prolactin Normal prolactin, Abnormal TSH Both normal Progestin challenge test Thyroid disease Withdrawal bleed No withdrawal bleed Normogonadotropic hypogonadism Estrogen/progestin Challenge test Hyperandrogenic anovulation No withdrawal bleed PCOS Cushing’s Outflow obstruction Asherman’s Cervical stenosis Normal TSH, Abnormal prolactin Prolactin < 100 ng/mL Prolactin > 100 ng/mL • Medication MRI to evaluate for prolactinoma Negative MRI Consider other causes Withdrawal bleed Check FSH Medication FSH > 20 IU/L Hypergonadotrpoic hypogonadism Ovarian failure FSH < 5IU/L MRI to evaluate for pituitary tumor Normal MRI Hypothalamic Hypogonadotropic amenorrhea hypogonadism Chronic illness Secondary Amenorrhea/Oligomenorrhea: Evaluation Progestin challenge test Medroxyprogesterone acetate 10 mg daily for 10 days IF withdrawal bleed occurs – Not outflow tract obstruction IF no withdrawal bleed occurs – Estrogen/Progestin challenge test Estrogen/Progestin challenge test Oral conjugated estrogen 0.625 – 2.5 mg daily for 35 days Medroxyprogesterone acetate 10 mg daily for 26-35 days IF no withdrawal bleed occurs – Endometrial scarring Hysterosalpingogram or Hysteroscopy to evaluate endometrial cavity Secondary Amenorrhea/Oligomenorrhea: Evaluation Evaluation of hyperandrogenism Symptoms: hirsutism, acne, alopecia, masculinization, and virilization Differential diagnosis: Adrenal disorders: Atypical congenital adrenal hyperplasia (CAH), Cushing’s syndrome, Adrenal neoplasm Ovarian disorders: PCOS, Ovarian neoplasms Lab: Testosterone, DHEA-S, 17α-hydroxyprogesterone Hormone Level Indication Testosterone < 200 ng/dL PCOS > 200 ng/dL Evaluate for adrenal or ovarian tumor < 700 ng/dL PCOS > 700 ng/dL Evaluate for adrenal or ovarian tumor DHEA-S 17α-hydroxyprogesterone > 4 ng/mL Consider ACTH stimulation test to diagnose CAH Amenorrhea/Oligomenorrhea: Management Treatment should be directed at… Correcting the underlying pathology Helping woman to achieve fertility (IF desired) Preventing the complications of disease process Consequences of untreated amenorrhea/oligomenorrhea: Hypoestrogenism – Osteoporosis, Infertility Hyperestrogenism – Heart disease, Stroke, Diabetes Mellitus, Breast cancer (controversial), Endometrial hyperplasia and Endometrial cancer Amenorrhea/Oligomenorrhea: Management Diagnosis Management Ovarian insufficiency Premature ovarian failure Postmenopausal ovarian failure Hormone replacement therapy (HRT) *Congenital anatomic lesions Surgical correction *Presence of Y chromosome (i.e. AIS) Gonadectomy *Gonadal dysgenesis (i.e. Turner syndrome) Estrogen + progestin, growth hormone IVF (IF pregnancy desired) Hyperprolactinemia Dopamine agonist (Bromocriptine, Cabergoline) Functional hypothalamic amenorrhea Increase caloric intake > energy expenditure Hypothalamic or pituitary dysfunction (non-reversible) OCP’s, pulsatile GnRH or exogenous gonadotropins CNS tumor Craniopharyngioma Prolactinoma Surgical resection Microadenoma (< 10mm) – Dopamine agonist Macroadenoma (>10mm) – Trans-sphenoidal resection PCOS OCP’s, weight loss, and metformin Asherman’s syndrome Hysteroscopic lysis of adhesions *Causes of primary amenorrhea only Bottom Line Concepts A thorough history and physical examination as well as laboratory testing can help narrow the diagnosis of amenorrhea. In patients with primary amenorrhea, the presence or absence of sexual development should direct evaluation. Constitutional delay of puberty is a diagnosis of exclusion. The definitive method to identify hypothalamic-pituitary dysfunction is to measure FSH and prolactin levels. If the patient has abnormal uterine development, a karyotype analysis should be performed to diagnose müllerian agenesis versus chromosomal abnormalities. In a patient with secondary amenorrhea, pregnancy should be ruled out prior to further workup. Treatment goals of amennorrhea and oligomenorrhea include prevention of complications such as osteoporosis, endometrial hyperplasia and heart disease; preservation of fertility; and in primary amenorrhea, progression of normal pubertal development. References and Resources APGO Medical Student Educational Objectives, 9th edition, (2009), Educational Topic 43 (p92-93). Beckman & Ling: Obstetrics and Gynecology, 6th edition, (2010), Charles RB Beckmann, Frank W Ling, Barabara M Barzansky, William NP Herbert, Douglas W Laube, Roger P Smith. Chapter 35 (p315-319). Hacker & Moore: Hacker and Moore's Essentials of Obstetrics and Gynecology, 5th edition (2009), Neville F Hacker, Joseph C Gambone, Calvin J Hobel. Chapter 32 (p355-363). Master-Hunter T, Helman DL. Amenorrhea: evaluation and treatment. Am Fam Physician. 2006 Apr 15; 73(8): 1374-82.