HG UC
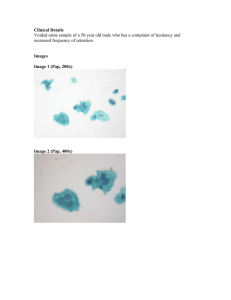
advertisement

بسم هللا الرحمن الرحيم Interpretation of urine cytology Nashwa Emara M.D.,phd ASS. Prof. Pathology Function • Majority of UT malignancies are urothelial CA. • The main function of urine cytology is diagnosis of UC. Indications Diagnosis of symptomatic patients (hematuria). Screen high risk patients (industrial chemicals, metals, etc.) Follow-up patients with UT neoplasia. Complementary to cystoscopy and biopsy: detect small and hidden lesions (diverticuli, ureters, renal pelvis).. Urine cytology is the most reliable method for detecting urothelial CIS (>biopsies). Types of Specimens Voided urine (avoid 1st morning specimens) Catheterized urine (in Females) Washings/Brushings Superior to voided urine but localized, may not sample upper urinary tract and urethra Ileal conduit urine Deep Vs Superficial Cells Columnar and Squamous Cells Normal Urine Cytology Washing, Instrumentation, Lithiasis Diagnostic Accuracy Number of Specimens: -Voided urine on 3 consecutive days. + 50% accuracy (1 specimen) + 75-90% accuracy (3 specimens) Patient Population: High risk and history of CA Tumor Grade: • HG UC: 78 - 98% • LG UC: 0 - 70% Grading Systems for Papillary UC 1973 WHO 1998 WHO/ISUP Urinary Cytology Papilloma Papilloma Low-grade Papillary Urothelial Lesion* Grade I PUNLMP Low-grade Papillary Urothelial Lesion Grade II Low-Grade Low-grade Urothelial Carcinoma Grade III High-Grade High-grade Urothelial Carcinoma WHO Grading of Papillary Urothelial Malignancies Features PUNLMP Low-grade UC High-grade UC Polarity Normal Minimal loss Disordered Superficial cells Usually present May be present Absent Papillary architecture Delicate Fused+ Delicate Fused Nuclear size Increased Increased Greatly increased Pleomorphism Slight Moderate Marked Nuclear polarization Slight abnormal Abnormal Absent Hyperchromasia Slight Moderate Marked Mitoses None or Rare Present Prominent Nuclear grooves Present Present Absent Chromatin Fine, uniform Mild variation Marked variation PUNLMP Low-grade Urothelial Carcinoma Cytologic diagnosis of LG PUC is problematic Minimal shedding of neoplastic cells Subtle cytologic alterations Difficult to distinguish from reactive changes, i.e. stones, instrumentation Cytologic overlap between PUNLMP and LG UC, some cases indistinguishable Low-grade Urothelial Carcinoma vs Reactive Low-grade Urothelial Carcinoma Diff. Diag. of LGUC Reactive/reparative changes Instrumentation effect Lithiasis Upper urinary tract sampling Low-grade UC Vs Benign LGUC Vs Instrumentation Instrumentation Effect Catheterized urine & bl. wash specimens. Large pseudopapillary groups and 3D clusters. Nuclear overlap and crowding. Low N/C ratio. Finely granular chromatin with even distribution. Well defined cytoplasmic borders. Nuclear palisading at periphery of clusters with abundant cytoplasm. Lithiasis Cytology of Upper Urinary Tract specimens Direct sampling of upper UT is effective in detecting HG UC, but poor for low grade lesions Normal upper UT epithelium shows more atypia than lower UT and occasionally more than LG UC High N/C ratio, enlarged nuclei, nuclear membrane irregularities Often present in papillary clusters Almost impossible to distinguish low grade UC from upper tract benign changes Renal Pelvis & Ureter Brushings High-grade Urothelial Carcinoma Often invasive, 70 mortality. Can not reliably separate CIS from invasive high-grade UC. High diagnostic accuracy of cytology: - Sensitivity 80 %. - Specificity > 95%. HGUC Diff. Diag. of HGUC Viral infection Therapy effect Degenerative and reactive changes Upper urinary tract specimens Stones Polyoma Virus (Decoy Cells) Therapy Effect Degenerative Changes Diagnostic categories Negative Atypical, rule out LGUC /PUNLMP Suspicious for HG UC/ malignancy HG UC/ other malignancies(Murphy) Summary Urothelial neoplasms can be separated into 2 main categories: –Low grade neoplasia (PUNLMP and LG UC). –High grade UC. Urine cytology best applied to HG UC. Cytology less helpful for detecting and monitoring LG neoplasms. –Not major limitation. –LG neoplasms rarely aggressive and can be readily detected by cystoscopy. N.B.: Ancillary techniques are highly sensitive GOOD LUCK…..