Pathology 21 p972-982 [5-6
advertisement

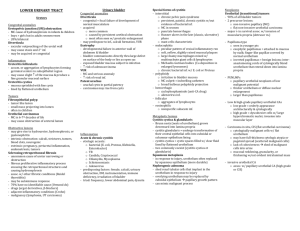
Pathology 21 p972-982: The Lower Urinary Tract - - - Renal pelves, ureters, bladder and urethra lined by urothelium, surface layer “umbrella cells” (trilaminar membrane and uroplakins) with BM and lamina propria under o Lamina propria forms discontinuous muscularis mucosae Ureters retroperitoneal, pass anterior to common iliac or external iliac artery, close to uterine arteries o 3 narrowings: ureteropelvic junction, bladder entry, crossing iliac vessels o Oblique course allows for sphincteric valve to block reflux Uterine prolapse pulls floor of bladder creating cystocele in vagina Seminal vesicle and prostate posterior an inferior to neck of bladder o Prostatic hypertrophy may obstruct ureters Ureters - - - - Congenital Anomalies = o Double and bifid ureters -> either double renal pelves or 1 large kidney, unilateral o Ureteropelvic junction (UPJ) obstruction -> results in hydronephrosis (most common cause), boys, bilateral in 20%, agenesis of opposite kidney o Diverticula -> asymptomatic, pockets of stasis and 2° infection, hydroureter (dilation), elongation and tortuosity of ureter Inflammation = ureteritis, not associate with infection o Morphology: Accumulation of lymphocytes w/ elevation -> ureteritis follicularis Fine cysts in mucosa -> ureteritis cystica Tumors and Tumor-Like Lesions = benign tumors generally mesenchymal, fibroepithelial polyp projects in lumen (children), malignant tumors (from renal pelvis, calyx or bladder) majority urothelial carcinomas Obstructive lesions = may lead to hydroureter, hydronephrosis, pyelonephritis, unilateral from proximal cause, bilateral from distal cause (nodular prostatic hyperplasia) o Sclerosing Retroperitoneal Fibrosis = fibrous proliferative inflammatory process encasing the retroperitoneal structures and causing hydronephrosis; idiopathic (Ormand disease; 70%) autoimmune reaction Treatment = ureterolysis Urinary Bladder - - Diverticula = evagination of bladder wall, predispose to infection (stasis) o Congenital form -> failure of normal musculature o Acquired diverticular -> w/ prostatic enlargement, increased pressure causes outpouching Exstrophy = anterior abdominal wall opening, mucosa subject to infection, ↑ risk of adenocarcinoma - - - - - Vesicoureteral reflux = most common and serious anomaly, infections and scarring Congenital vesicouterine fistulas = connection b/w bladder and vagina, rectum, or uterus Urachus = patency, fistulous urinary tract, may be urachal cysts (carcinomas may arise) Acute and Chronic Cystitis = common from Escherichia coli, Proeus, Klebsiella, and Enterobacter, women>men o tuberculous cystitis sequal to renal tuberculosis o candida albicans cause in immunosuppression and Schistosoma haematobium common in Middle East (Egypt). Viruses, Chlamydia and Mycoplasma may also cause o Predisposing factors -> calculi, obstruction, DM, instrumentation, immune deficiency, irradiation (radiation cystitis) o Morphology: Hyperemia of mucosa Cytotoxic antitumor drugs and adenovirus infection develop hemorrhagic cystitis Follicular cystitis -> lymphocytic aggregation Eosinophilic cystitis _. Infiltration with submucosal eosinophils o Clinical: Triad of symptoms: 1) frequency, 2) lower ab pain, 3) dysuria (pain or burning) Interstitial cystitis (Chronic Pelvic Pain Syndrome) = persistent, painful form of chronic cystitis occurring most frequently in women o pain, frequency, urgency, hematuria and dysuria without infection o fissures and punctate hemorrhages (glomerulations) in mucosa o chronic mucosal ulcers (Hunner ulcers) = late (classic, ulcerative) phase o Biopsy rules out carcinoma Malacoplakia = peculiar pattern of vesical inflamm reaction, soft, yellow, mucosal plaques 34cm, infiltration with large, foamy macrophages mixed with multinucleate giant cells and interspersed lymphocytes o Michaelis-Gutmann bodies within macrophages o Chronic bacterial infection (E. coli or Proteus species) and immunosuppressed transplant recipients Polypoid Cystitis = inflammatory condition from irritation to bladder mucosa (catheters most commonly), confused with papillary urothelial carcinomas Cystitis Glandularis and Cystitis cystica = nests of urothelium (Brunn nests) grow into lamina propria -> transform into cuboidal/columnar lining (cystitis glandularis) or cystic space (cystitis cystica) o Goblet cells and intestinal mucosa appearance = intestinal or colonic metaplasia o Squamous metaplasia -> response to injury (more durable) o Nephrogenic Adenoma -> from shed tuular cells implanting at sites of injured urothelium, replaced by cuboidal epithelium (papillary growth pattern) Neoplasms = 95% of epithelial origin, urothelial or transitional tumors o o Urothelial Tumors = 90% of all bladder tumors, precursor lesions -> non-invasive papillary tumors and flat non-invasive urothelial carcinoma (in situ, CIS; changes of malignancy but confined to epithelium) Decrease in survival with invasion of muscularis propria (detrusor muscle) Classification -> benign urothelial papilloma, urothelial neoplasm of low malignant potential, papiallry urothelial carcinoma grade 1-3 Morphology: Papillary (excrescences), nodular or flat gross patterns Papillomas -> younger, exophitic, covered by epitheliam that is histologically identical to normal urothelium Inverted papillomas -> benign, excised Papillary urothelial neoplasma of low malignant potential (PUNLMPs) > thicker urothelium or diffuse nuclear enlargement Low-grade papillary urothelial carcinomas -> evenly spaced (maintain polarity) and cohesive, infrequent mitotic figures, rare threat High-grade papillary urothelial cancers -> dyscohesive, large hyperchromatic nuclei, frequent mitotic figures, loss of polarity (80% invasive) o may invade surrounding organs or produce fistulas or metastasize to lymph nodes Carcinoma in situ (CIS or flat urothelial carcinoma) -> malignant, pagetoid spread, lack of cohesiveness, shedding of cells Invasive urothelial cancer -> high grade urothelial cancer or CIs, staging is most important factor for outlook Variants of urothelial carcinoma -> nested variant, lymphoepitheliomalike carcinoma, and micropapillary carcinoma Other epithelial tumors Squamous cell carcinomas -> where shcistosomiasis is endemic, more frequent, chronic bladder irritation and infection Mixed urothelial carcinomas with areas of squamous carcinoma -> invasive, fungating, infiltrative, ulcerative Adenocarcinomas -> some from urachal remnants or with intestinal metaplasia Small-cell carcinomas Pathogenesis: Men > women, developed > undeveloped nations, urban > rural Cigarette smoking increase risk Industrial exposure to arylamines Schistosoma haematobium infections (Egypt, Sudan), 70% squamous Long-term analgesics use and exposure to cyclophosphamide (hemorrhagic cystitis) Bladder irradiation - Chromosome 9 monosomy or deletions are the only genetic changes present frequently in superficial papillary tumors and occasionally in noninvasive flat tumors Invasive urothelial carcinomas deletions of 17p (p53 gene) Initiated by deletions of tumor suppressor genes on 9p and 9q -> superficial papillary tumors Initiated by p53 mutations -> CIS and invasion (w/ chrom9) Clinical: Painless hematuria (dominant manifestation) Frequency, urgency, dysuria Urothelial tumors tendency to recur (higher grade each time) Low-grade, papillomas, low malignant tumors -> 98% 10-year survival Clinical challenge is early detection and adequate follow-up -> cytologic exams and biopsy o Cystectomy for invasion of muscularis propria, CIS or highgrade, and CIS extending into prostatic urethra o Mesenchymal tumors Benign Tumors = most common is leiomyoma, isolated, intramural, encapsulated Sarcomas = large masses protrude into vesicle, fleshy, grey-white, most common in infancy is embryonal rhabdomyosarcoma (grapelike mass sarcoma botryoides), in adults is leiomyosarcoma o Secondary Tumors = from nearby organs or lymphomas Obstruction = bladder neck, from prostatic nodular hyperplasia, strictures, fibrosis, tumors, foreign bodies/calculi, and denervation o Morphology: Thickening of bladder wall (trabeculation) Crypts form -> become diverticula If dilated, wall is thinned, no trabeculation Urethra - - Inflammation = accompanied by cystitis in women and prostatitis in men, pain, itching and frequency o Gonococcal urethritis = early manifestation of infection o Nongonococcal urethritis = bacteria (E. coli), Chlamydia (25-60% in men, 20% women), Mycoplasma (Ureaplasma urealyticum) o component of Reiter syndrome (arthritis, conjunctivitis, urethritis) Tumor and Tumor-like lesions = o Urethral caruncle = inflammatory lesion, painful, in external urethral meatus o Benign epithelial tumors -> squamous, urothelial papillomas, inverted urothelial papillomas, conylomas o o Peyronie disease = fibrous bands, corpus cavernosum of penis, penile curvature and pain Carcinoma of the urethra -> if proximal urothelial differentiation, if distal squamous; fungating growth