slides 2
advertisement

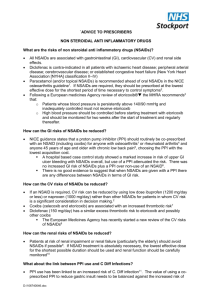
First MTP Osteoarthritis Hallux valgus with bunion OA is a Problem with the Cartilage! Osteoarthritis: Risk Factors • Secondary Osteoarthritis: The degeneration is secondary to an injury to the cartilage • Primary Osteoarthritis: No obvious cartilage injury • Erosive (hand) OA: runs in families, autosomal dominant but more penetration in women • Often starts 5-10 years pre to post menopause, adds more joints (DIPs, PIPs), can mimic psoriatic arthritis, burns out with bony changes Risks for OA • • • • • • Advanced Age Female Genetics Obesity Occupation (overuse) Trauma Osteoarthritis: Laboratory • All laboratory investigations should be normal in osteoarthritis • Labs and Xrays are not necessary to make the diagnosis Osteoarthritis: Management • Non-Pharmacologic – Exercises – Strengthening – Splinting • Pharmacologic – Oral Medications Surgery – Topical Medications – Injectable Medications – Alternative/Complimentary Choices Goals of Treatment 1. Pain Reduction 2. Improved Function 3. Changes the Disease Outcome 4. Low Cost 5. Low Side Effects Proper Footwear Strength Training Assistive Devices Physical & Occupational Therapy Education Exercise & Weight Loss Topical Medications 1. Capsaicin 2. Topical Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) Pennsaid, Diclofenac Topical NSAIDs Limited Use for Osteoarthritis • Small effects in clinical trials • Apply 4 times per day • Expensive • Messy Benefits • Little systemic absorption Intra-Articular Corticosteroids Pros • Cheap • Relatively Safe: 1 in 15-20,000 risk of infection • Safe to do 4 injections in a single joint per year Cons • Short term benefit at 4 to 8 weeks but negative at 12 and 24 weeks • Predictors of response are unclear Viscosupplementation • Joints typically contain a small amount of lubricating fluid called synovial fluid. • Hyaluronic acid is a component of this synovial fluid • Synovial fluid Hyaluronic acid is decreased in patients with osteoarthritis • Viscosupplements are synthetically or biologically derived Hyaluronic Acid Viscosupplementation • Given by a series of 1 to 3 injections once a week depending on the product • Only approved for osteoarthritis of the knee • The effects are variable lasting months in some people and not working at all in others Viscosupplementation Pros • If it works, may have a significant benefit Cons • Expensive ~ $300 per course • The effects are variable lasting months in some people and not working at all in others • Post-injection pain, swelling • Not very good clinical trial data Oral Medications 1. Simple Analgesics 2. Non-Steroidal Anti-Inflammatory Medications (NSAIDs) 3. Narcotic Analgesics and non-narcotic (tramadol) 4. Complimentary Therapy (Glucosamine) Acetaminophen • Acetaminophen (Tylenol ) • Useful in mild to moderate osteoarthritis Pros • Cheap • Safe • Proven Benefit Cons • Small effect • Often need 3g/day Non-Steroidal AntiInflammatory Drugs (NSAIDs) • Traditional NSAIDs • COX-2 Selective NSAIDs (COXIBs) Prostaglandin Synthesis Cell Membrane Phospholipids Arachidonic Acid NSAIDs COX-1 Prostaglandins COX-1 Continuously Expressed GI Tract Platelets Endothelium Kidney NSAIDs COX-2 Prostaglandins COX-2 Upregulated Synovial Lining Macrophages Chondrocytes Endothelium Macula Densa Non-Steroidal AntiInflammatory Drugs (NSAIDs) Traditional NSAIDs • Block the Actions of COX-1 and COX-2 • Available Over the Counter (Ibuprofen) • Several (Ibuprofen, Diclofenac, Naproxen, etc) COX-2 Selective NSAIDs (COXIBs) • Only Block the Action of COX-2 • Only 1 available – Celecoxib (Celebrex) NSAIDs & COXIBs: What Works • NSAIDs consistently outperform acetaminophen in OA treatment NSAIDs & COXIBs: What to look out for • • • • • • GI Risk – gastric and duodenal ulcer Renal Risk – raise creatinine and HTN Cardiovascular Risk - ?increased MIs Hepatoxicity Edema Allergic reactions Clinical Risk Factors for NSAID Gastropathy 1. History of Ulcer Related Complications • 2. 3. 4. 5. 6. 7. 8. 13.5% Previous ulcer, bleeding Multiple NSAIDs High-dose NSAIDs Concomitant Anticoagulation Age > 69 Age > 59 Concomitant Steroids History of CV disease 9.0 % 7.0 % 6.4% 5.6% 3.1% 2.2% 1.8% More Patients are Without Appropriate Gastroprotection Patients >65 years not receiving gastroprotective approaches with their NSAIDs (%) 100 No gastroprotection 80 60 40 20 0 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004 2005 Year Singh G, et al. Gastroenterology 2006; 130(Suppl. 2): A-82 (Abstract 564). NSAIDs & COXIBS: Cardiovascular • All NSAIDs may increase the risk of MI (possibly) and some more than others • Use the lowest possible dose for the shortest duration of time Narcotics • Benefits – Codeine does have some evidence for efficacy, however, it also has a high incidence of side-effects. – Oxycodone, morphine, and hydromorphone may be better choices • Side Effects – Increaed in the elderly – Sedation, confusion, constipation • Risk for Falls and other Accidents Addiction • It is EXCEEDINGLY rare for patients with OA to show addictive behaviour. In fact, a study of over 800 patients with OA treated with opioids for 3 years found only 4 (0.02%) to have addictions. (Ytterberg S, Mahowald M, Woods S. Codeine and oxycodone use in patients with chronic rheumatic disease pain. Arthritis Rheum 1998;41:1603-12.) • OA patients stop opioids after surgery. (Visuri T, Koskenvuo M, Honkanen R. The influence of total hip replacement on hip pain and the use of analgesics. Pain 1985;23:19-26.) Glucosamine: The Theory • Glucosamine is a component of cartilage • Glucosamine is reduced in osteoarthritic cartilage • Replacing glucosamine may have beneficial effects Glucosamine: The Evidence • You are a believer or not – Both positive and negative trials • Withdrawal trial and NIH trial were both essentially negative • DONA (RottaPharm) – Only brand of glucosamine to show positive benefit in trials – All trials sponsored by pharmaceutical company Glucosamine: Practicality • Dose: 500 mg three times daily • If no effect after 3 months stop ? Take with chondroitin Seems very safe Surgery for Osteoarthritis Surgery: Who is appropriate • Most people with arthritis, including older individuals, should be referred for surgical treatment when other treatment is ineffective and function is impaired. • Surgery should not be used as a last resort • There is no “magic age” for surgery Surgery: Why Consider Consider surgery before: • Advanced muscle weakness • Joint deformities • Significant loss of function with further deconditioning Treatment Conclusions • Non-Pharmacologic Therapy – Education – Physical Therapy • • • • • – – – – Assessment Education Strengthening Range of Motion Joint Protection & Energy Conservation Weight Loss & Nutrition Cardiovascular Exercise Shoes & Insoles Assistive Devices Treatment Conclusions • NSAIDs – Work very well in select patients – Try a few NSAIDs before find the right one for you. – 3 week trials of at least 3 different NSAIDs. • Injectable Corticosteroids – Work well in some patients • Viscosupplementation – Can work well in some patients (milder disease) • Opioids – Can provide considerable benefit Treatment Conclusions Lack of Scientific Evidence for • Acupuncture • Magnet Therapy OA Guidelines Other • Exercise • Brace, Taping • Weight Loss • Joint replacement Medications • Acetaminophen • NSAIDs/Coxibs • Topical agents • Injectable agents Questions