Dr Adam Harris, Consultant Gastroenterologist
advertisement

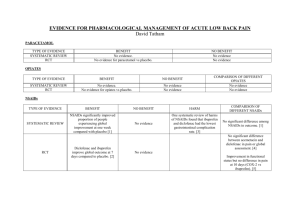
Case Studies in Luminal Gastroenterology Adam Harris Consultant Gastroenterologist The Spire Tunbridge Wells Hospital Luminal Gastroenterology Learning objectives: 1. Avoiding foregut complications of NSAIDs 2. Understanding new dietary option in IBS 3. Understanding latest drug treatments in constipation Case Study 1 87 yr old woman with OA, nocturnal joint pains, angina & bleeding DU 1999 Needs pain relief – what do you recommend? NSAIDs & Bleeding ulcers • PMH of ulcer bleeding who use NSAIDs are at highest risk (20%) of re-bleeding • Use NSAID plus standard dose PPI • Despite this 4-8% will re-bleed in 6 months Chan et al. New Engl J Med 2002; 347:2104-10. NSAIDs High Risk of Complications • PMH PUD or bleed • >65 yrs • Longterm use; high dose • More than one NSAID • Co-prescribed steroids, clopidogrel or warfarin • Serious co-morbidities Risk of gastro-duodenal ulcer Placebo + Aspirin Naproxen + Aspirin Celecoxib + Aspirin 8% 27% 19% NSAIDs & PPIs 4 points to remember: 1. PPIs decrease risk of NSAID-associated GU & DU cf placebo 2. PPIs equally effective whether non-selective NSAIDs or COX-2 inhibitors 3. PPI co-therapy is effective in healing & preventing recurrent ulcers with long term NSAIDs 4. PPIs decrease risk of NSAID-associated bleeding Aspirin 4 points to remember: 1. Aspirin increases risk of UGIB 4 fold 2. Aspirin + other NSAID increases risk 8 fold 3. No difference in RR with EC or “junior” 4. Eradication of H pylori decreases risk of ulcer Lai et al. New Engl J Med 2002; 346: 2033-38 McQuaid KR, Laine L. Am J Med 2006; 119: 624-38 Arora G et al. Clin Gastro Hepatol 2009; 7: 725-35 Case Study 2 24 yr old female with 1-2 year of recurrent low abdominal pain, bloating & intermittent watery diarrhoea Unemployed & lives alone Normal examination Blood tests, urine & stool culture normal Faecal calprotectin <50 Low FODMAP diet • Fermentable, Oligo-, Di-, Mono-saccharides and Polyols • Comprise fructose, lactose, fructans, galactans & polyols • Low FODMAP diet developed at Monash University in Melbourne, Australia FODMAPs in diet • • • • • Fructose eg fruits, honey, corn syrup Lactose eg diary Fructans eg wheat, onion, garlic Galactans eg beans, lentils, legumes Polyols eg sorbitol, avocado, apricots, plums Low FODMAP • FODMAP CHO trigger changes in fluid content & bacterial fermentation in bowel leading to symptoms in susceptible individuals • Follow low FODMAP diet to eliminate fermentable carbohydrates; trained dietician required. • Eliminate from diet for trial period then re-introduce each FODMAP carbohydrate gradually & record symptoms • Reported (by enthusiasts) that up to 70% of patients report improvement in symptoms Case Study 3 28 yr old woman with 5 yr history of constipation (BO 2 x/wk) with straining & passage of hard stool; bloating & low abdo discomfort No incontinence. No neurological illness. Examination & blood tests normal. Tried fibre, lactulose, Movicol, Senna, bisacodyl with limited or no benefit. Differential Diagnosis? Differential Diagnosis? • IBS-C • Idiopathic Slow Transit Constipation • Functional Outlet Obstruction Investigation? Colonic Transit Marker Study IBS-C ISTC Functional Outlet Obstruction Treatment Options • IBS-C linaclotide (Constella) • ISTC prucalopride (Resolor) • Functional Outlet Obstruction Further assessment; surgery; biofeedback Prucalopride • 5-HT4 receptor agonist with entero-colonic kinetic activity; not a laxative • Women only • Works within 2-3 hours • ↑ spontaneous bowel movements: 67% vs 39% placebo (p<0.001) • Improves symptoms of pain, bloating, straining & tenesmus Prucalopride • • • • 2mg od for 28 days If no response: do not continue 1mg od: women>65 yr; liver/renal failure AE: nausea; headache; abdo pain; diarrhoea • Cost: 28 x 2mg ≈ £60 Linaclotide • Guanylate cyclase-C agonist • Reduces visceral hypersensitivity, increases intestinal secretion & accelerates transit • Treatment of moderate-severe IBS-C in adults • One capsule (290 mcg) od 30 mins before meal • Interaction: OCP, thyroxine • Adverse effect: diarrhoea (<20%) • Cost: £37.56 for 28 days Linaclotide • 47% decrease in abdo pain over 26 weeks (p<0.001 vs placebo)1 • 40% improvement in bloating over 26 weeks (p<0.0001 vs placebo)1 • Increase in spontaneous bowel movements from 1.7 to 5.7 weekly over 12 weeks (p<0.0001 vs placebo)2 • Improvement in QoL (p<0.01 vs placebo) 1. Quigley EM et al. Aliment Pharmacol Ther 2013; 37:49-61 2. Chey WD et al. Am J Gastroenterolo 2012; 107: 1702-12 Luminal Gastroenterology Learning objectives: 1. Avoiding foregut complications of NSAIDs 2. Understanding new dietary option in IBS 3. Understanding latest therapies in constipation