Discussion Presented by:
Jay Hall PA-S II
Ali Rahimi MD
Osteoarthritis is a prevalent and rising
chronic joint disorder.
We will discuss epidemiology, pathology,
clinical signs and symptoms, as well as
current a upcoming treatment options.
Prevalence varies with the definition of the
disease.
Rotterdam study:
Population based cohort of 3906 people
Showed that among people 55 years or older 67% of
women and 55% of men had radiographic OA of the
hand.
Most commonly affected sites
Hand – 100 per 100,000 person years
Hip – 88 per 100,000 person years
Knee – 240 per 100,000 person years
Since cartilage is avascular, the supply of nutrients and
oxygen to damaged areas and chondrocytes is
restricted.
This leads to a cluster of chondrocytes and an
increased synthesis of tissue-descructive proteinases.
Inadequete repair of the matrix leads to inability to
withstand mechanical stress, and a cycle is created.
Loops of soluble factors released by the chondrocytes
trigger the inflammatory process that accelerates
breakdown.
Due to the aneural component of cartilage, this
destruction is not symptomatic until adjacent
innervated tissue and structures are involved.
Synovial involvement leads to swelling and pain,
thought to be secondary to cartilage debris
entering the synovial cavity.
Synovial macrophages further promote
inflammation and creates a vicious cycle.
Occurrence
Knee
Hip
Hand
Age, sex,
physical activity,
BMI, quad
strength, bone
density,
smoking,
genetics
Age, physical
activity,
previous injury,
intense sports,
genetics
Age, grip
strength,
occupation,
genetics
Age,
symptomatic
activity, sex,
intense sports
Unknown
HRT (protective)
Progression
Age, BMI,
vitamin D,
chronic joint
effusion,
misalignment,
synovitis
HRT (protective)
Pain and restricted joint ROM are typical
presenting symptoms.
Pain Weight bearing related
AM stiffness <30 minutes (vs. RA)
“Classic” symptoms
◦ Heberden and Bouchard nodes
Several pitfalls:
◦ Differential must include: rheumatoid, psoriatic,
gonoccocal (younger pt with knee pain)
◦ Identify the proper site of pain!
Hip pain can be referred to knee and anserine bursa!
Lumbar spine stenosis can cause hip, knee and ankle
pain!
A biomarker is a molecule or molecular
fragment that is released into a biologic fluid
(serum, urine, synovial fluid)
Seem to associate with structural changes but
not clinical progression.
Research has failed to produce validity due to
markers flucuating status depending on stage
of disesase
IE a marker may elevate early but decrease with severity
Markers of cartilage degradation have been
studied the most and show moderate to good
relation with osteoarthritis
CTXII – in urine + in 74% of population with OA
Recently focused on in a pilot study that showed CTXII
decreased after administration of calcitonin (which inhibits
osteoclast activity)
COMP – in serum + in 54% of population with OA
Studying markers of bone metabolism have been
less effective
Presumably due to high turn-over rate of bone molecules
Synovial metabolism markers are least
studied but produce positive results.
HA in the serum has been the most reliable
biomarker so far
The conclusion is that none of the available
biomarkers are sufficiently effective to aid
in diagnosis, nor are any consistent enough
to function as an outcome in clinical trials.
Treatment should focus on improving pain
and stiffness as well as preventing further
joint damage.
Three main modalities
◦ Non-pharmacological
◦ Pharmacological
◦ Surgical
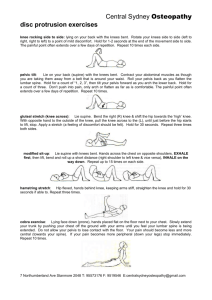
Non-pharmacologic
◦ Joint conservation efforts: weight reduction
load of 4:1 at hip and 8:1 at knee
Improved physical function, decreased pain
Positive changes in cartilage and bone biomarkers
◦ Exercise that strengthens muscles and improves CV are most
effective for OA of hip/knee.
◦ Effect size of 0.20-0.50
◦ RCTs show weight reduction will decrease pain
◦ Heat/Ice are easy to use and effective in reducing symptoms
despite scarce data
◦ Scarce evidence with varying effect size
◦ Information regarding osteoarthritis can reduce symptoms
◦ Effect size <0.20
Pharmacological
APAP is first line analgesic for OA because of safety and
effectiveness
NSAIDs non-selective or cyclo-oxygenase 2 selective
drugs can be used for:
OA of hip/knee/hand -- preferably the lowest effective dose for
shortest time
Patients with high GI risk should use COX-2
inhibitor or NSAID/PPI
Recent study of celecoxib vs. diclofenac + omeprazole in pts
with osteo and RA:
showed equal treatment for upper GI problems but celecoxib
showed reduced GI events (anemia of GI origin).
Pharmacologic
◦ Opioid treatment has been increasing but
improvement in patients who fail to receive
beneifit from NSAIDs is only seen with strong
opiods (oxycodone, fentanyl) which is generally
reserved for exceptional circumstances.
◦ Weaker opioids (tramadol, codeine) have not been
assessed in long term trials, and absence of
evidence for safety and concerns about
dependence should be considered.
Weaker opioids (tramadol, codeine) have not been
assessed in long term trials, and absence of evidence
for safety and concerns about dependence should be
considered.
APAP/codeine combos show a small (5%) but
statistically significant (P<0.05) benefit over
APAP alone but are associated with more
adverse events.
◦ Diacerein (interleukin 1 inhibitor) has a slow acting but persistant relief
◦
Effect size 0.24 95%CI (0.08-0.39)
◦ Glucosamine sulphate has been studied thoroughly in the United States
but no beneficial effect has been reported.
◦
◦
Effect size varies from 0.30 to 0.87 depending on study
No effect of structure modification
◦ Hyaluronic acid has varying effectivness depending on injection regiment.
◦
Effect size of 0.39
◦ Inta-articular injection of steroids is effective for “flares” but diminishes
after 1 week.
◦
Effect size for pain relief 0.58
◦ Cochrane review of surgical lavage and debridement shows no benefit
short or long term vs. placebo.
Focused on displaying that osteoarthritis is
not a single disease, different forms present
with different clinical and structural
characteristics.
New developments in pathophysiology of OA
prompt the division of disease into
distinguishable phenotypes (such as: pain,
trauma, structure and age)
This will allow for specific, phenotype
delineated treatment. However consensus for
definition of phenotypes will take time to be
reached.
PostTraumatic
Metabolic
Agerelated
Genetic
Pain
Age
Young
(<45y)
Middle age
(45-65y)
Old (>65y)
Variable
Variable
Causative
Feature
Mechanical
stress
Mechanical
stress,
adipokines*,
hormone
imbalance,
hyperglycem
ia
AGE,
Gene
chondrocyt related
e
senescence
Main Site
Knee,
thumb,
ankle,
shoulder
Knee,
Hip, knee,
hand,
hand
generalized
Hand, hip,
spine
Hip, knee,
hand
Interventio
n
Joint
protection,
joint
stabilization,
prevent falls,
surgical
Weight
loss,
glycemic
control,
lipid
control,
HRT
No specific
interventio
n, gene
therapy
Pain
medication,
antiinflammato
ry drugs
No specific
interventio
n
Inflammato
ry, bony
changes,
altered
pain
perception
Growing knowledge of pathogenic
mechanisms of osteoarthritis will lead to new
drugs to target treatment.
Recent pilot studies with calcitonin (inhibits
osteoclast) and nitric oxide inhibition show
promising possibilites.