Heparin
advertisement

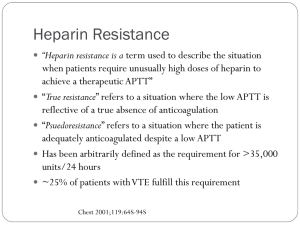
Heparin Benedict R. Lucchesi, M.D., Ph.D. Department of Pharmacology University of Michigan Medical School Heparin Chemistry –Low molecular weight fractions of heparin have a high affinity for ACTIVATED FACTOR X (Xa), but have less of an effect on thrombin. Antithrombin-Binding Structure of Heparin I II OSO-3 COO- O O OH IV *OSO O COOOH CH2OSO3 O O O III O OH NH R’’ D-Glucosamine D-Glucuronic Unit Acid R’= H or -SO3R’’= COCH3 or -SO3- 3 O V H2CO R’ O O OH O HNSO3OSO3HNSO3D-Glucosamine L-Iduronic D-Glucosamine Acid * Antithrombin binding region Groups essential for high affinity binding of antithrombin ATIII Thrombin Lysine Sites 5 13 or more saccharide units Heparin ATIII Factor Xa Lysine Sites 5 <13 Low Molecular Weight Heparin Inhibition of thrombin and Factor Xa by the Heparin/AT III complex through a unique pentasaccharide unit. Binding to thrombin requires a minimum of 13 saccharide units. Low molecular weight heparin acts to inhibit Factor Xa and requires that the latter only bind to AT III. Anticoagulant Therapy Heparin –Actions of Heparin »Inactive by itself as an anticoagulant »Requires the presence of a plasma cofactor- ANTITHROMBIN III (AT III) »Heparin potentiates the action of AT III »Heparin-AT III-complex neutralizes the actions of: Factors II, IX, X, XI, XII and XIII »Binds to lysine sites on AT III, leads to conformational change at the arginine reactive center INTRINSIC PATHWAY EXTRINSIC PATHWAY IXa VIIa / Tissue Factor TFPI VIIIa aPC = sites of Heparin/ATIII Inhibition FACTOR Xa Prothrombin aPC Protein S Platelet Aggregation Va Thrombin PC / Thrombomodulin aPC Inactivation Va & VIIIa Fibrinogen XIIIa Fibrin Actions of Heparin 1. Low concentrations of heparin increase the activity of AT III considerably, especially against Factor Xa and THROMBIN - these are the most sensitive components of the coagulation cascade 2. Rationale for the clinical use of “mini-dose” heparin 3. Inhibition of THROMBIN requires that both the AT III complex and the ENZYME bind to heparin 4. Inhibition of FACTOR Xa requires that heparin only bind to AT III Actions of Heparin (continued) 5. Binds strongly to AT III - leads to conformational change of AT III 6. Active site of AT III is exposed 7. The active AT III inhibits the proteases involved in coagulation Factors II, IX, X, XI, XII and XIII 8. Heparin is NOT consumed, but is released from the AT III complex and is available to react to AT III. Heparin Pharmacokinetics • Heparin binds to saturable sites on the endothelial cells • It is internalized and depolymerized • It displaces platelet factor 4 from the endothelial cells - a protein that neutralizes heparin Heparin-Anticoagulant action is modified by: Fibrin - –Clot bound fibrin binds thrombin and protects it from inactivation by heparin-AT III. Platelets –Bind factor Xa and protect it from heparin-AT III complex inhibition and by secreting platelet factor 4 »Not the case with HIRUDIN (AT III independent). »Subendothelial thrombin is protected from heparinAT III as well. Heparin-Contraindications –Patients who are hypersensitive –Presence of active bleeding or hemophilia –Thrombocytopenia –Purpura –Severe hypertension –Intracranial hemorrhage –Bacterial endocarditis –Active tuberculosis –Ulcerative lesions of GI tract Heparin-Contraindications –Threatened abortion –Visceral carcinoma –During or after surgery on the brain, spinal cord or eye –Patients undergoing lumbar puncture or regional anesthesia block –History of heparin-induced thrombocytopenia Heparin-Adverse Effects Side Effects Dose Related Major Bleeding Yes Thrombocytopenia Yes with thrombosis Yes Osteoporosis Yes Anaphylaxis No Skin necrosis ? Local urticaria ? Hypoaldosteronism ? Frequency 5% 5 - 15% 0.4% Rare Rare Rare Rare Rare Heparin-Induced Thrombocytopenia vs Heparin-Induced Thrombocytopenia and Thrombosis Heparin-Adverse Effects (continued) Heparin-Induced Thrombocytopenia TWO FORMS: –Mild reduction in platelet count, 2-15 days after initiation of full-dose heparin therapy –Platelet count usually remains above 100,000/µl. Bleeding risk is minimal Heparin-Adverse Effects (continued) Heparin-Induced Thrombocytopenia-and Thrombosis –Severe reduction in platelet count, 7-14 days after initiation of therapy with full-dose or lowdose heparin –May be associated with thrombotic complications, including arterial thrombosis with platelet-fibrin clots that may cause MI or stroke –Presence of antiplatelet IgG in patients with severe form ? –May be less common with heparin from pork. Heparin - Laboratory Monitoring aPTT / TCT –Therapy is routinely monitored by means of the aPTT (at UofM it is the TCT) –A clotting time of 1.5 to 2.0 times the normal mean aPTT value (50 - 70 seconds) is therapeutic –Initially the aPTT should be measured and the infusion rate adjusted every 4 hours. –Once a steady state is achieved, daily monitoring is sufficient. Resistance to Heparin • Some patients may not show a prolongation of the aPTT unless very high doses of heparin are used • Presence of an increased concentration of FACTOR VIII will give rise to a very short control aPTT - they may not be truly resistant to heparin Heparin-Resistance to Heparin (continued) • Accelerated clearance of heparin may exist - as in the case of massive pulmonary embolism • Inherited AT III deficiency have 40 - 60 % of the normal plasma concentration of AT III. They respond normally to heparin • Acquired AT III deficiency as with hepatic cirrhosis, nephrotic syndrome or disseminated intravascular coagulation; large doses of heparin may not prolong the aPTT Heparin - Managing OverAnticoagulation • Anticoagulant effect of heparin disappears within hours after discontinuation of the drug. • Mild bleeding due to heparin can be controlled without administration of an antagonist. • Antagonists are used if bleeding is lifethreatening. Heparin - Managing of OverAnticoagulation Management depends on: –Degree of over-anticoagulation –Presence or absence of bleeding –A specific, immediate heparin antagonist –Protamine Sulfate –Use 25 - 50 mg intravenously –Side-effects largely allergic in nature Heparin: Managing Overanticoagulation (cont’d) • Protamine binds to the acidic (negatively charged) heparin molecule - neutralizes heparin. • Protamine also interacts with platelets, fibrinogen, and other plasma proteins. • Use smallest dose, give by slow IV infusion - do not exceed 50 mg over 10 min. - Causes, flushing, bradycardia, dyspnea, hypotension, anaphylaxis. • Use 1 mg of protamine for every 100 units of heparin remaining in the patient. • Protamine sulfate is a low molecular weight, basic (positively charged) protein. Heparin - Clinical Uses –Effective for the prevention and treatment of: • venous thrombosis and pulmonary embolism • mural thrombosis after acute MI • managing unstable angina • prevention of coronary artery rethrombosis • used to prevent blood clotting in extracorporeal • • circulation - e.g. surgery, hemodialysis treat selected cases of disseminated intravas-cular coagulation (DIC) treat fetal growth retardation in pregnant women Heparin - Recommendations for Clinical Use Pregnancy - heparin is the anticoagulant of choice –does not cross the placenta –no untoward effects in the fetus or newborn –given in therapeutic doses - 15,000 U sc q 12 hrs to women with prosthetic heart valves or venous thromboembolism –doses in excess of 20,000 U per 24 hrs for more than 5 months is questionable -due to risk of OSTEOPOROSIS Low Molecular-Weight Heparins Enoxaparin (Lovenox™) Dalteparin (Fragmin™) –contain a lower proportion of the critical pentasaccharide sequence than the parent compound. –they increase the action of ATIII on factor Xa, but not its action on thrombin. Low Molecular-Weight Heparins • The LMWHs are not inactivated by platelet factor 4, therefore activity extends to factor Xa bound to platelet membranes. • In clinical doses, no affect on platelet reactivity, PT or aPTT. • Currently approved for prevention of deep vein thrombosis: • After hip or knee surgery or abdominal surgery. • Unstable angina (NQWMI). Low Molecular Weight Heparins • Do not require routine monitoring of INR, PT, or aPTT. • One fixed dose administered subcutaneously. – 30 mg every 12 hours. • Must not be administered IM and is not intended for IV administration. • Use with caution in patients with a history of heparin-induced thrombocytopenia. • Reversed by protamine, 1 mg for each mg of LMWH.