High-Alert Medications: Safeguarding Against Errors Part 2
advertisement

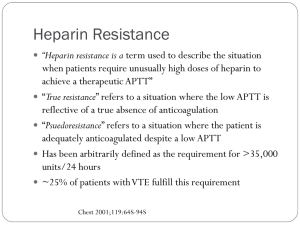
High-Alert Medications: Safeguarding Against Errors (Part 2) Learning Objectives • Describe examples of specific safety improvements to prevent errors with highalert medications • Outline a framework to examine high-alert drugs in your institution This presentation describes the steps for specific safety improvements for the use of just two separate high-alert medications. The Medication Errors textbook has similar suggestions for approximately 30 more high-alert drugs and classes of drugs. Instructors may assign students to prepare similar strategies for safeguarding the use of high-alert medications in their respective institutions. Step #1 • Identify potential or actual problems that have occurred with use of the high-alert drugs in your institution or system-wide within your organization – – – – Review adverse drug reaction (ADR) reports Review literature Refer to examples in the textbook, chapter 14 Confer with a multidisciplinary group within your organization Step #1 (continued) • Problems or errors may occur because of: – – – – – Dosing errors Calculation errors Concentration errors IV admixture errors Duplicate or concurrent therapy Step #1 (continued) • Problems or errors may occur because of: – – – – – – Improper manufacturer labeling Look-alike drug names and packages ADRs Injection of drug with preservatives Contamination Incompatibilities Step #2 • Make the key improvements described in the first part of the high-alert medications section of this program, including the use of: – – – – – Fail-safes Constraints Externalize error-prone processes Improve access to information Standardize Step #2 (continued) • Make the key improvements including the use of: – – – – – – Simplification Differentiation Reminders Redundancies Patient monitoring Failure mode and effects analysis Unfractionated Intravenous Heparin • Known dosing errors include: – Temporary increase in the pump rate to deliver a bolus dose has caused errors because staff have forgotten to reset the pump after delivery of the bolus – Abbreviating heparin units as “U” has led to 10-fold overdoses – Pump setting errors involving either concentration or rate of infusion have resulted in dosing errors Unfractionated Intravenous Heparin • Known calculation errors include: – Math errors in determining the volume of heparin to administer for a bolus dose, or the rate of infusion of a maintenance heparin solution – Practitioners, particularly pharmacy staff, have miscalculated the volume of heparin to be added to TPN or other electrolyte solutions Unfractionated Intravenous Heparin • Known concentration errors include: – Various concentrations of IV heparin bags and heparin vials have been mixed up, in part because of look-alike vials and bags – Mix-ups have occurred between heparin 1,000 units/500 mL bags used for maintenance of adult arterial lines and 25,000 units/500 mL bags for IV use Unfractionated Intravenous Heparin • Known IV admixture errors include: – In settings where a standard concentration of commercially available heparin is not in use, nurses and pharmacists have made errors when mixing heparin solutions Unfractionated Intravenous Heparin • Known duplicate or concurrent therapy errors include: – Patients already receiving low-molecular weight heparin who are inadvertently also placed on continuous IV heparin Unfractionated Intravenous Heparin • Known errors involving improper manufacturer labeling include: – Labeling of small-volume injectable products may display the concentrations (e.g., 10,000 units/mL) but not the total volume (10 mL), which can lead practitioners to believe the container holds 10,000 units, not 100,000 units Unfractionated Intravenous Heparin • Known errors involving look-alike drug names and packages include: – Look-alike vials of heparin (flush solutions) and insulin (both dosed in “units”) are often found together on top of medication carts or counters, resulting in occasional mix-ups – Prefilled syringes or cartridges may resemble other drugs Unfractionated Intravenous Heparin • Known errors involving adverse drug reactions include: – Poor monitoring of potential thrombocytopenia • Known errors involving injection of drug with preservatives include: – In newborns, administration of IV heparin that is not preservative-free has caused benzyl alcohol toxicity Unfractionated Intravenous Heparin • Known errors with incompatibilities include: – Reteplase and heparin, which are incompatible, have been used in combined administration through the same IV line, causing a precipitating mass that stopped an infusion Suggested Key Improvements for the Use of IV Unfractionated Heparin • Fail-safes – Use only free-flow protected pumps to administer heparin infusions • Constraints – Do not store heparin vials (flush solution) on top of medication carts and counters – Do not store heparin solutions for arterial lines near other injectable solutions Suggested Key Improvements for the Use of IV Unfractionated Heparin • Externalize error-prone processes – Use commercially premixed solutions • Improve access to information – Have the pharmacy place a label on both sides of the bag, taking care not to obscure the manufacturer’s label – Affix dosing charts (printed on labels) to heparin infusion bags – Use the patient’s actual weight in kilograms (kg) as the basis for determining heparin doses Suggested Key Improvements for the Use of IV Unfractionated Heparin • Simplify – Use weight-based heparin infusion charts or nomograms to determine bolus doses and infusion rates – Do not deliver a bolus by temporarily modifying the rate of a maintenance infusion; administer the bolus directly from a syringe connected to an IV access port Suggested Key Improvements for the Use of IV Unfractionated Heparin • Differentiate – Use unit-dose syringes for heparin flushes to differentiate them from other injectable products that are packaged in vials (e.g., insulin, normal saline) and to avoid potential contamination of vials – Separate the storage of heparin syringes from look-alike syringes of other medications Suggested Key Improvements for the Use of IV Unfractionated Heparin • Differentiate (continued) – Separate heparin and insulin, which are both measured in units and may have a similar 100 unit/mL concentration, adding to potential for confusion – Use TALL-man letters on auxiliary labels and order entry screens to differentiate HeSpan and hEParin Suggested Key Improvements for the Use of IV Unfractionated Heparin • Reminders – Affix to infusion bags a reminder to perform an independent double check before starting the infusion – Build alerts into order entry systems to remind pharmacists to dispense preservative-free heparin to neonates Suggested Key Improvements for the Use of IV Unfractionated Heparin • Redundancies – Require an independent double check of the drug, concentration, dose calculation, rate of infusion, pump settings, line attachment, and patient identity before the start of a heparin infusion and with each change of the bag or rate of infusion – Have infusion pump settings independently checked by two persons Suggested Key Improvements for the Use of IV Unfractionated Heparin • Redundancies (continued) – Have line placement on dual-channel pumps independently checked by two persons – Require an independent check of all admixtures involving heparin in the pharmacy (including the addition of heparin to TPN or other electrolyte solutions) Suggested Key Improvements for the Use of IV Unfractionated Heparin • Patient monitoring – Develop and follow a standard format for communicating to the pharmacy dose adjustments based on laboratory values – Develop and follow a standard process for obtaining aPTT values at required intervals and communicating the results to prescribers Suggested Key Improvements for the Use of IV Unfractionated Heparin • Patient monitoring (continued) – Establish and follow a protocol for detecting heparin-induced thrombocytopenia, treating patients who develop signs of this ADR, and communicating this information Suggested Key Improvements for the Use of IV Unfractionated Heparin • Failure mode and effects analysis – Have an interdisciplinary team perform FMEA for all forms of heparin therapy (including flushes), and remedy risks that could harm patients – Evaluate the packaging and labels on all heparin products to identify potential for confusion and remedy problems by repackaging or switching manufacturers to improve distinction and clarity of labeling and packaging Opioids • Known dosing errors include: – Misprogramming of infusion pumps leading to serious opioid overdoses – Fentanyl patches have not been removed prior to application of a new patch, leading to overdoses; the clear backing of some patches makes them difficult to see once applied to the skin Opioids • More known dosing errors include: – Fentanyl has sometimes been improperly prescribed for episodes of acute pain, such as postoperative pain or pain from dental surgery – Poor patient education has led to multiple patches being applied to the site of pain, leading to serious overdoses and fatalities Opioids • More known dosing errors include: – Physicians have prescribed fentanyl patches in doses that were too high for opioid-naïve patients, leading to overdoses and fatalities – Opium tincture has been dispensed and administered instead of paregoric (camphorated tincture of opium), leading to overdoses and fatalities Opioids • Redundancies bypassed – Narcotic accidents are among the most frequent of all serious incidents reported. One reason for errors with these drugs is that injectable narcotics are usually kept in nursing areas as floor stock items. Doses are identified, prepared, and administered by the same nurse; no redundant safety checks are performed. Opioids • Look-alike drug names – Mix-ups between hydromorphone and morphine are common; most often they are related to the look-alike product names and some practitioners’ misconception that hydromorphone is the generic name for morphine. Hydromorphone is approximately five times more potent than morphine. Opioids • Look-alike drug names (continued) – Opioids are often stored side by side in secured cabinets or drawers. This has contributed to selection of the wrong medication, as have the look-alike syringes, vials, and minibags of various opioids. Opioids • Miscommunication of drugs – The abbreviations MSO4 (for morphine sulfate) and MgSO4 (for magnesium sulfate) have been confused, leading to administration of morphine when magnesium was intended – DTO (as an abbreviation for deodorized tincture of opium) has been used to mean diluted opium tincture (1:25) or paregoric, leading to confusion about the actual dose and to serious dosing errors Opioids • Concentration errors – Concentrated forms of oral liquid morphine (20 mg/mL) have often been confused with the standard solution (2 mg/mL), leading to serious errors and fatalities – Pharmacists and nurses have selected the 5 mg/mL morphine concentration instead of the 1 mg/mL concentration for patientcontrolled analgesia (PCA) use Opioids • Concentration errors (continued) – Overdoses of oral liquid morphine have resulted when physicians prescribe the drug by volume rather than by metric weight and nurses use the more concentrated form to prepare the dose – Extended-release and immediate-release morphine products have been confused Opioids • Errors caused by “PCA by proxy” – Delivery of opioid doses via PCA devices by nurses or family members has led to serious and fatal dosing errors – Improper patient selection for PCA has led to unsafe use in unresponsive adults, young children, and neonates, who cannot activate the pump themselves Opioids • Errors caused by accidental epidural administration – PCA and epidural lines are sometimes confused, leading to errors in route of administration Opioids • Errors with PCA infusion pump design flaws – Several manufacturers’ PCA pumps have unsafe default settings; for example, one pump defaults to a 0.1 mg/mL setting, which has been misread as 1 mg/mL during programming for a morphine infusion Opioids • Adverse drug reactions – Allergic reactions to opioids are common – Gastrointestinal complaints are common – Meperidine use, especially in the elderly, has led to toxic levels of its metabolite, normeperidine, which, in turn, may induce irritability and nervousness, agitation, tremors, and even seizures Opioids • Inadequate pain control – Some patients have not received adequate pain control because they do not know how to use the PCA device • Patient monitoring problems – Insufficient monitoring of patients receiving opioids has resulted in respiratory arrest Opioids • Errors caused by unintended use – Fentanyl patches prescribed for adults have been applied by young children because of unsecured storage or disposal (used patches still contain significant amounts of the active drug) Suggested Key Improvements for the Use of Opioids • Constraints – Limit oral liquid narcotics in floor stock to conventional concentrations; avoid stocking concentrated morphine solutions in patient care areas – Dispense concentrated oral morphine solutions only when ordered for a specific patient (not as unit stock) Suggested Key Improvements for the Use of Opioids • Constraints (continued) – Separate morphine and hydromorphone in all drug storage areas – Avoid the use of meperidine for pain control, especially in the elderly – Consider deleting paregoric and opium tincture from all formularies Suggested Key Improvements for the Use of Opioids • Constraints (continued) – Return unused supplies of concentrated liquid morphine to the pharmacy immediately after patient discharge – Instruct patients who use fentanyl patches to store and dispose of the patches in a secure manner to avoid unintended access by children, pets, or drug-seeking adults Suggested Key Improvements for the Use of Opioids • Improve access to information – Educate staff about the possibility of mix-ups between hydromorphone and concentrated morphine – Post equianalgesic charts for opioid-to-opioid conversions on all patient care areas for reference by prescribers and nurses Suggested Key Improvements for the Use of Opioids • Improve access to information (continued) – Include the brand name “Dilaudid” along with the generic name hydromorphone when prescribing, transcribing, and dispensing (on labels) this drug – Educate patients and caregivers about the proper use of PCA Suggested Key Improvements for the Use of Opioids • Improve access to information (continued) – Before applying a fentanyl patch to a newly admitted patient, ask about patches that may have been applied at home; if the patient is unable to respond, thoroughly inspect the skin before applying the patch – Establish dose ranges for opioids by weight, and build alerts into the order entry system for exceeding maximum doses Suggested Key Improvements for the Use of Opioids • Standardize – Establish one standard concentration for each opioid in use – Use only generic names, except for hydromorphone, which can be more easily distinguished by using the brand name, Dilaudid, followed by the generic name – Reduce the variety of available opioids through the use of protocols and standard order sets Suggested Key Improvements for the Use of Opioids • Standardize (continued) – Establish protocols and preprinted orders for PCA – In establishing patient selection criteria for PCA, consider this safety feature: a sedated patient will not press the PCA button – Standardize to a single drug, morphine, as the opioid of choice for PCA Suggested Key Improvements for the Use of Opioids • Differentiate – Stock morphine and hydromorphone in different strengths or forms (e.g., 1 mL prefilled syringes of hydromorphone 1 mg/mL; 2 mL prefilled syringes of morphine 2 mg/mL – Use TALL-man lettering, HYDROmorphone, on pharmacy labels, auxiliary labels, medication administration records, and drug listings in the computer Suggested Key Improvements for the Use of Opioids • Differentiate (continued) – Affix an auxiliary label to concentrated solutions to avoid confusion with standard concentrations – Apply auxiliary labels to prefilled syringes of opioids that look similar to help people differentiate them Suggested Key Improvements for the Use of Opioids • Reminders – Label the distal ends of all access lines to distinguish IV from epidural lines – Apply auxiliary labels to concentrated forms of morphine or other opioids, noting that the drugs are highly concentrated Suggested Key Improvements for the Use of Opioids • Reminders (continued) – If concentrated morphine is available on patient units, affix an auxiliary label to the bottle and segregate the concentrated solution from the other strengths – Build alerts into the computer system to warn staff about the differences between paregoric and opium tincture Suggested Key Improvements for the Use of Opioids • Redundancies – Implement protocols for the use of PCA and other opioids that ensure independent double checks of the appropriateness of the drug, dose, pump setting, and line placement – Question all patients about allergies and sensitivities to opioids before administration Suggested Key Improvements for the Use of Opioids • Patient monitoring – Ensure that oxygen and naloxone are available in areas where narcotics are administered – Establish guidelines for appropriate monitoring of patients receiving opioids – Do not rely on just pulse oximetry readings to detect opioid toxicity Suggested Key Improvements for the Use of Opioids • Failure mode and effects analysis – Conduct FMEA for PCA to uncover risks and take action to reduce the chance of harmful errors Reference Cohen MR, Smetzer JL, Tuohy NR, Kilo CM. High-alert medications: safeguarding against errors. In: Cohen MR, ed. Medication Errors. 2nd ed. Washington, DC: American Pharmacists Association; 2007.