Heparin Resistance
advertisement

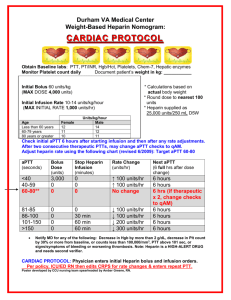
Heparin Resistance “Heparin resistance is a term used to describe the situation when patients require unusually high doses of heparin to achieve a therapeutic APTT” “True resistance” refers to a situation where the low APTT is reflective of a true absence of anticoagulation “Psuedoresistance” refers to a situation where the patient is adequately anticoagulated despite a low APTT Has been arbitrarily defined as the requirement for >35,000 units/24 hours ~25% of patients with VTE fulfill this requirement Chest 2001;119:64S-94S Heparin: Background MOA •Catalyzes antithrombin’s irreversible binding to clotting factors Xa and IIa (thrombin) • Prevents further coagulation but is not a thrombolytic PK Elimination 1. Rapid, saturable clearance through binding to endothelial cells/proteins 2. Renal elimination T1/2 – dose dependant, but typically between 1-2 hours Heparin: Mechanism ATIII forms irreversible covalent bonds with thrombin or Xa Only heparin molecules with at least 18 saccharides (~6000 daltons)can bind both antithrombin and thrombin Only activated coagulation factors are targeted Unique Pentasaccharide sequence that interacts with antithrombin AT III Heparin: Monitoring APTT Evaluates the activity of the intrinsic pathway (factors I,II, V, VIII, IX, XI, XII,). APTT Not affected by inhibition of Xa. (target 1.5 to 2.5 times normal) Antifactor Xa Evaluates the amount of factor Xa that the heparin in the blood is able to neutralize (target 0.35 to 0.7 units/ml ref: http://www.ncbi.nlm.nih.gov/pubmed/8267489) http://www.fritsmafactor.com/newfritsmafactor/?p=2489 Heparin Resistance: Mechanisms Heparin Resistance: Mechanism Mechanisms Effects clearance due to binding to acute Phase reactants (true resistance) •Levels of certain acute phase reactants and other plasma proteins that bind to and clear heparin are increased in inflammatory states. • A study found septic patients have more heparin bound to plasma proteins (Young Arteriosclerosis Thrombosis and vascular biology 1997;17:1568)). •Another study found acute-MI patients(an inflammatory condition) have more heparin bound to proteins and associated lower aPTT (Rich J Thromb Thrombolysis 2007;23:93) •Another study found acute-PE patients have lower free heparin levels than acute-DVT patients (Hirsh. Circulation 1976;53:691) ATIII Deficiency (true resistance) production Cirrhosis Loss Nephrotic Syndrome Enhanced consumption Sepsis with DIC Burn injuries Hepatic veno-occlusive disease CABG Large hemotomas Genetic: Autosomal dominant, fatal if homozygotic with prevalence rate between 1:500-1:5000 Heparin Resistance: Mechanism Mechanisms Effect Factor VIII (?psuedo resistance) •Mean factorVIII level in heparin resistant patients of 2.39 U/ml vs 1.60 U/ml in non resistant patients. APTT lower in patients with high factor VIII. Anti-Xa assay may be more accurate reflective of degree of anticoagulation (Levine. Ach Intern Med 1994;154:49) but some authors disagree (British J Haematology;2010:613) •Some observational studies have found that with progressively increasing Factor VIII levels there is an increasing risk of venous thrombosis. (Kamphuisen. Arterioscler Thromb Vasc Biol 2001;21:721) •Factor VIII levels are increased in association with obesity, diabetes, fibrinogen, triglycerides, increased age and is an acute phase reactant (malignancy, chronic disease, infection) (Kamphuisen. Arterioscler ThrombVasc Biol 2001;21:721) LMWH in patients with heparin resistance? Mechanisms Effects Increased clearance due to binding to acute Phase reactants •LMWH have reduced binding to plasma proteins and as a result have much more consistent anti-Xa and antiIIa activity. (Cosmi. Circulation 1997;95:118) (Hirsh. Blood 1992;79:1) ATIII Deficiency Factor VIII Dependant on ATIII for their activity. Unclear effect Fondaparinux in patients with heparin resistance? Mechanisms Effect Increased clearance due to binding to acute Phase reactants ATIII Deficiency Factor VIII •At therapeutic concentrations fondaparinux is highly (94%) and specifically bound to antithrombin III. Would indicate that increased clearance via protein binding is unlikely (Clin Pharmacokinetics 2002;41 Suppl 2:11) Dependant on ATIII for activity Unclear effect Rivaroxaban in patients with heparin resistance? Mechanisms Effect Increased clearance due to binding to acute Phase reactants ATIII Deficiency Factor VIII •Mainly eliminated through metabolism (3A4, 3A5, 2J2) with remainder removed via kidneys. No indication that pharmacokinetics are altered in sepsis Independent of ATIII Unclear effect Dabigatran in patients with heparin resistance? Mechanisms Effect Increased clearance due to binding to acute Phase reactants ATIII Deficiency Factor VIII •Not highly bound to plasma proteins. Mainly eliminated via urine/fecal routes. Independent of ATIII Unclear effect Heparin Resistance Summary Should be evaluated for when patients are receiving >35,000 units/24 hour period Patients with heparin resistance may be over or under anticoagulated depending on the etiology of their resistance If possible consider switching to alternative agent (LMWH, fondaparinux or oral anticoagulant) If not possible consider testing anti-factor Xa levels (target 0.35 to 0.7 u/ml). If therapeutic with low aPTT then likely psuedoresistance