Diseases of the
exocrine pancreas
Exocrine Pancreatic Insufficiency
Exocrine Pancreas Insufficiency (EPI)
• Inability to process nutrients efficiently due
to lack of production of enzymes from
pancreas.
– Pancreatic acinar atrophy
• Found most commonly in German
Shepherds and Rough Collies through a
recessive gene.
– In cats, EPI is primarily the result of chronic
pancreatitis
Diagnosis of EPI
• Not usually evident until 85-90% of pancreas
is unable to secrete enzymes.
– Weight loss although no change in diet or appetite
(appetite often increases)
– Persistent tarry diarrhea.
– Flatulence
– Poor haircoat
Testing and treatment for EPI
• TLI (trypsin-like immunoreactivity)
– Detects trypsin and trypsinogen
– Usually want below 2.5 in dogs to be diagnostic
• Canine 5.7-45.2
• Feline 12-82
• Treatment includes enzymatic supplement
– Viokase powder
– Raw ox or pig pancreas
Client considerations
•
•
•
•
Usually life long treatment.
Can be very expensive.
Can be well controlled.
Should not breed animal that has EPI.
DISEASES OF THE ADRENAL GLANDS
CUSHING’S DISEASE
(Hyperadrenocorticism)
ADDISON’S DISEASE
(Hypoadrenocorticism)
Adrenal Glands
ADRENAL GLANDS
mineralocorticoids
Glucocorticoids
Androgens
epinephrine
Physiology
• Hypothalamus – Corticotropin realeasing factor
(CRF) >>> Anterior Pituitary Gland –
Adrenocorticotropic hormone (ACTH)
– >>> ADRENAL CORTEX
• Glucocorticoid hormone
• Mineralocorticoid hormone
• Sex hormones (Androgens)
• SNS >>> ADRENAL MEDULLA >>> Epinehrine and
norepinephrine
– Increase HR, Inc. BP, Dilated air passages – lungs, dec.
GI function, vasoconstriction
Hormone Functions
Mineralocorticoids – Aldosterone
•
•
•
•
Regulates electrolyte and H2O balance
Hypoadrenocorticism/ Addison’s
Primarily Dogs
Life threatening
Glucocorticoids
•
•
•
•
•
Promote gluconeogenesis
Suppress inflammation
Suppress immune system
Inhibit cartilage growth and development
Hyperadrenocorticism / Cushing’s
Hyperadrenocorticism (Cushing’s Disease)
• Definition: Disorder caused by deleterious effects
of high circulating cortisol concentrations on
multiple organ systems
• Systems affected:
–
–
–
–
–
–
–
–
Renal
Skin
Cardiovascular
Respiratory
Endocrine/metabolic
Musculoskeletal
Nervous
Reproductive
Cushing’s Disease
Effects of excess glucocorticoids:
1.
2.
3.
suppress inflammation
suppress immune system
inhibit cartilage growth, development,
and repair
Causes:
1.
2.
3.
Anterior pituitary lesion (pituitary-dependent disease) – 85% of
cases
Adrenal tumor (excess cortisol secretion independent of pituitary
control) – 15-20% of cases
Overmedication with glucocorticoids - Iatrogenic
Cushing’s Disease
Cushing’s Disease
Bilaterally symmetrical alopecia, pot-belly, pyoderma
Cushing’s Disease
Pot bellied
PU/PD
Muscle wasting
Thin coat
Cushing’s Disease
signs are slow to develop and usually go unnoticed by owner
Clinical Signs:
1. Some are similar to hypothyroidism
2. Dog >6 yr old (most are female)
3. PU/PD/PP
4. Pot bellied; obese
5. Muscle atrophy and weakness, lethargy, excess
panting
6. Bilateral symmetric alopecia; pruritis; pyoderma (↓
immune response)
7. Calcinosis cutis (firm plaques of Ca++ under skin)
8. Abnormal gonadal function (lack of estrus; soft,
small testicles)
Cushing’s Disease: Calcinosis cutis
Commonly seen on the dorsal midline, ventral abdomen and inguinal region.
Skin is usually thin and atrophic
Cushing’s Disease: Dx
Chemistry Panel
1.
2.
3.
4.
↑ ALP, ALT, cholesterol, blood glucose
↓ BUN
Lipemia
Low USG < 1.015, proteinuria, hematuria, pyuria, bactiuria
Urine cortisol/creatinine ratios (sample collected at home)
1.
2.
Normal ratio=no Cushing’s
Elevated ratio=may be Cushing’s
ACTH Stimulation test
1.
2.
3.
Normal patients show an increase of plasma cortisol
Pituitary dependent disease (excess ACTH release) and Adrenal tumors: 60-85%
show EXAGGERATED cortisol response
Does not differentiate between Pit disease and Adrenal tumor
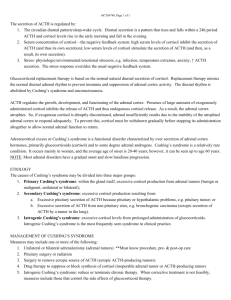
ACTH Stimulation for Hyperadrenocorticism
• Take a pre blood sample.
• Inject ACTH stimulation gel or liquid
– Verify amounts with lab as there is
difference between amount to be injected
with gel and liquid.
• Wait two hours and take a post sample
Cushing’s Disease: Dx
Low-Dose Dexamethasone Suppression Test
1.
2.
Inject low dose of steroid (should suppress ant. pit [ACTH])
Measure plasma cortisol at 0, 4, 8 h
Interpretation:
1.
2.
Normal dogs will show decrease in plasma cortisol
Pituitary tumor and adrenal tumor will not show any effect at 8
h (cortisol will still be high)
Cushing’s Disease: Dx
High-Dose Dexamethasone Suppression Test (used to
differentiate between Pit Dis and Adrenal tumor)
1.
2.
Dosing: 0.1 mg/kg IV
Collect plasma cortisol at 0, 4, and 8 h
Interpretation:
1.
2.
Pituitary dependent disease—70-75% will show decrease at 4
or 8 h
Adrenal tumor—no change in plasma cortisol level (tumor is
autonomous)
Cushing’s Disease: Rx
Surgical removal—
1.
2.
FAT - Specialized surgery; most vets would refer surgery
Pituitary tumors are not surgically removed
Medical treatment
1.
Lysodren (o,p,DDD)—necrosis of z fasiculata (middle), z reticularis
(deep)
-repeat ACTH stimulation q 7-10 d until cortisol normal
-like chemotherapy
-excess dose affects z glomerulus (Addison’s Dis)
Cushing’s Disease: Rx
2. trilostane (Vetoryl®)—less side-effects
than o,p,DDD
-interfers with cortisol production
(doesn’t kill cells)
-FDA approved
Cushing’s Disease: Client info
•
•
•
•
Serious disease; life-long treatment
Periodic monitoring required
Addison’s disease may result
Prognosis: average life expectancy is
20-30 mo on therapy with frequent
recurrence of clinical symptoms –
varies with cause (pit vs adrenal,
tumors)
• Hyperadrenocortism
Addison’s Disease (Hypoadrenocorticism)
• Definition: Disorder caused by deficient
production of glucocorticoids (cortisol) or
mineralocorticoids (aldosterone) or both
• Secondary disease caused by chronic
administration of corticosteroids
Addison’s Disease (Hypoadrenocorticism)
•
•
•
Not as common as Cushing’s Disease; rarely seen in cats
Deficiency of Glucocorticoids and Mineralocordicoids
Clinical signs due to Mineralocorticoid (Aldosterone) deficiency
Clinical Signs:
1.
2.
3.
4.
lethargy, weakness, anorexia, wt loss
Vomiting/Diarrhea
PU/PD, dehydration
Bradycardia
Addison’s Disease
• Pathophysiology
– Decreased aldosterone => Increased K and
decreased Na
– => decreased volume => azotemia,
hypotension, dehydration, weakness,
depression
– Hyper K => heart (bradycardia)
– Glucocorticoid deficiency => vomiting,
diarrhea, melena, lethargy, wt loss,
hypoglycemia (less common than expected)
Addison’s Disease: Dx
Chem Panel
Na:K ratio <25:1 !!!(normal=27:1 to 40:1)
↑ BUN, Creatinine, Ca++
↓ blood glucose, albumin (less common
ACTH Stimulation test (definitive test)
normal dog= ↑ cortisol
hypoadrenocorticism dog= low, unchanged cortisol level
Endogenous ACTH will be increased (1º hypoadrenocorticism; lack of neg
feedback)
What is your Dx?
Chem Panel
(What is not normal?)
Parameter
Value
BUN
81 mg/dl
Creatinine
2.1 mg/dl
Sodium 131 meq/L
Potassium
6.5 meq/L
Na:K ratio
20
Normal value
7-27 mg/dl
0.4-1.8 mg/dl
141-156 meq/L
4.0-5.6 meq/L
27-40
What is your Dx?
ACTH Stimulation Test Results
Value
Plasma Cortisol
Pre-ACTH
Post-ACTH
Normal
0.2
0.3
2-6
6-18
Addison’s Disease: Rx
Acute Crisis (may be life-threatening situation)
1.
2.
Normal saline IV (low Na+ is hallmark finding of Addison’s)
Glucorticoid replacement(cortisol will also be low)
a.
3.
Dexamethasone or Prednisone (IV or IM)
Mineralocorcorticoid replacement
a.
b.
Florinef® (fludrocortisone acetate)—po
Percortin-V (desoxycorticosterone pivalate) injection
Chronic Management
1.
Glucocorticoid replacement
a.
b.
2.
Mineralocorcorticoid replacement
a.
b.
3.
Prednisone
Prenisolone
Florinef® (fludrocortisone acetate)—po daily (not cheap; 50¢/tab)
Percortin-V (desoxycorticosterone pivalate)—inj ~monthly (expensive)
Monitor electrolytes, BUN/Creatinine, clinical signs
Addison’s disease: Client info
1.
2.
3.
4.
5.
6.
Mineralocorticoid deficiency is life-threatening
Animal requires periodic blood tests
Glucocorticoids needed in times of stress
Always remind attending vet of pet’s condition
Hormone replacement therapy continued for life of
pet
Prognosis: Good to excellent after stabilization and
treatment
• Hypoadrenocorticism
• Addison’s in crisis
References
• Alleice Summers, Common Diseases of
Companion Animals
• http://www.aahanet.org/PublicDocuments/A
AHADiabetesGuidelines.pdf
• http://www.vetmed.wsu.edu/cliented/diabete
s.aspx
• http://www.sciencedirect.com/science/article
/pii/S0378427408001732