Endocrinology 3b & 4a – Hyperadrenal Disorders and Pharmacology
advertisement
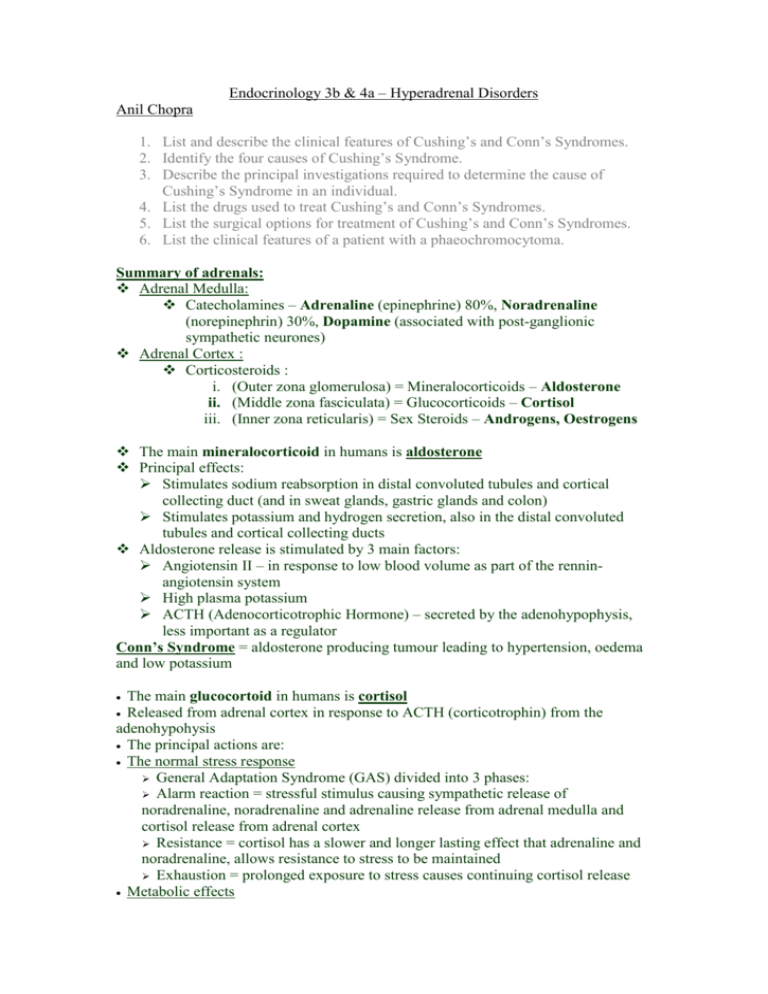
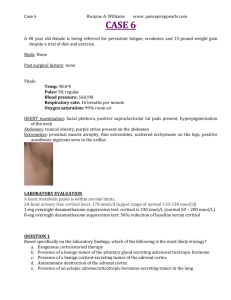
Endocrinology 3b & 4a – Hyperadrenal Disorders Anil Chopra 1. List and describe the clinical features of Cushing’s and Conn’s Syndromes. 2. Identify the four causes of Cushing’s Syndrome. 3. Describe the principal investigations required to determine the cause of Cushing’s Syndrome in an individual. 4. List the drugs used to treat Cushing’s and Conn’s Syndromes. 5. List the surgical options for treatment of Cushing’s and Conn’s Syndromes. 6. List the clinical features of a patient with a phaeochromocytoma. Summary of adrenals: Adrenal Medulla: Catecholamines – Adrenaline (epinephrine) 80%, Noradrenaline (norepinephrin) 30%, Dopamine (associated with post-ganglionic sympathetic neurones) Adrenal Cortex : Corticosteroids : i. (Outer zona glomerulosa) = Mineralocorticoids – Aldosterone ii. (Middle zona fasciculata) = Glucocorticoids – Cortisol iii. (Inner zona reticularis) = Sex Steroids – Androgens, Oestrogens The main mineralocorticoid in humans is aldosterone Principal effects: Stimulates sodium reabsorption in distal convoluted tubules and cortical collecting duct (and in sweat glands, gastric glands and colon) Stimulates potassium and hydrogen secretion, also in the distal convoluted tubules and cortical collecting ducts Aldosterone release is stimulated by 3 main factors: Angiotensin II – in response to low blood volume as part of the renninangiotensin system High plasma potassium ACTH (Adenocorticotrophic Hormone) – secreted by the adenohypophysis, less important as a regulator Conn’s Syndrome = aldosterone producing tumour leading to hypertension, oedema and low potassium The main glucocortoid in humans is cortisol Released from adrenal cortex in response to ACTH (corticotrophin) from the adenohypohysis The principal actions are: The normal stress response General Adaptation Syndrome (GAS) divided into 3 phases: Alarm reaction = stressful stimulus causing sympathetic release of noradrenaline, noradrenaline and adrenaline release from adrenal medulla and cortisol release from adrenal cortex Resistance = cortisol has a slower and longer lasting effect that adrenaline and noradrenaline, allows resistance to stress to be maintained Exhaustion = prolonged exposure to stress causes continuing cortisol release Metabolic effects Peripheral protein catabolism Hepatic gluconeogenesis Increased blood glucose Fat metabolism (lipolysis in adipose tissue) Enhanced effect of glucagon and catecholamines Some mineralocorticoid effects Renal and cardiovascular effects Excretion of water load Increased vascular permeability Other effects e.g. on bone, CNS, growth etc Effects of large amounts of cortisol: Anti-inflammatory action Immunosuppressive action Anti-allergic action All are associated with decreased production of molecules such as prostaglandins, leukotrienes, histamines etc as well as on the movement and function of leukocyte and the production of interleukins Normal cortisol release follows a circadian rhythm with the main production overnight Cushing’s Syndrome – excessive cortisol production (or other glucocortoid) Possible causes = taking steroids by mouth (most common), Cushing’s disease, Ectopic ACTH production such as in lung carcinoma, adrenal adenoma or carcinoma Cushing’s Disease – ACTH secreting tumour in the adenohypophysis Addison’s Disease – deficiency of cortisol and aldosterone (primary adrenal failure). Can be caused by autoimmune disease where adrenal is wiped out (most common in UK), or the commonest cause worldwide where tuberculosis destroys it Cushing’s Syndrome It is a condition caused by the production of too much cortisol. It causes protein to be converted to fat. Causes of Cushing’s Syndrome - Taking too many steroids - Pituitary dependent Cushing’s disease o Pituitary tumour that secretes ACTH - Ectopic ACTH e.g. from lung cancer. - Adrenal adenoma secreting cortisol. Symptoms of Cushing’s - Muscle weakness (proximal myopathy) - Hypertension & Hypokalaemia - Red straie, thin skin and easy bruising due to lack of protein synthesis - Poor wound healing - Moon face. - Proximal myopathy - Osteoporosis - Moon face Centripetal obesity Type II Diabetes Hirsutism Buffallo hump Thin hair and balding Increased pigmentation if Cushing’s Disease Oedema Depression confusion, insomnia Investigations - 24h urine collection. Check cortisol levels in urine. - Blood diurnal cortisol levels (throughout the day) o Cortisols usually highest around 9 am and lowest around midnight. o In Cushings, it is high all the time - Low dose dexamethasone (artificial steroid) suppression test. o 0.5mg every 6 hours for 48 hours o Dexamethasone = artificial steroid that stops the production of ACTH o Pituitary will switch off if normal. o Any cause of Cushing’s will fail to suppress. - High does dexamethasone o Used to distinguish pituitary Cushing’s from other types o Only pituitary Cushing’s will suppress to 50% o Basal cortisol 500nM o End of LDDST: 480nM o End of HDDST: 325nM o Ectopic and adrenal tumours will see no suppression Treatment - Removal of tumour by pituitary surgery (transsphenoidal hypophysectomy) - Bi-lateral adrenalectomy - Unilateral adrenalectomy Pharmacology The main drugs used in the treatment of Cushing’s syndrome are enzyme inhibitors. They inhibit different enzymes in the biosynthesis of cortisol: Name – Metyrapone Usage – Cushing’s Disease diagnosis. If given and ACTH and 11-deoxycortisol go up, then diagnosis of Cushing’s disease is confirmed (pituitary adenoma). If ACTH and 11-deoxycortisol don’t change then the tumour is ectopic (somewhere else) but still secreting lots of ACTH. It is also used as long term treatment when surgery is not possible. Mode of action – blocks the action of 11β hydroxylase and hence decreases the synthesis of cortisol very quickly. Side Effects - Nausea, vomiting, dizziness, sedation, hypoadrenalism, impaired performance in skilled tasks e.g. driving, operating machinery. Can also lead to hypertension in long term use. Administered orally. Name – Trilostane Usage – Cushing’s syndrome, primary hyperaldosteronism and reduction in sex steroid production (e.g. post-menopausal breast cancer). Mode of action – blocks the action of 3β -hydroxysteroid dehydrogenase and hence decreases the synthesis of all steroids. Side Effects - Nausea, vomiting, diarrhea, flushing. Name – Ketoconazole Usage – mainly used as anti-fungal. Also used to inhibit steroidogeneisis. Mode of action – blocks the action cytochrome P450 enzymes. Side Effects - nausea, vomiting, abdominal pain, alopecia, (hair loss) gynaecomastia (males developing breasts) oligospermia (low sperm count), ventricular tachycardias, liver damage, reduced androgen production. Name – Aminoglutethamide Usage – malignant adrenocortical & prostate cancer Mode of action – blocks conversion of cholesterol to pregnenolone. Side Effects – corticosteroids need to be replaced. Administered orally. Conn’s Syndrome Cause by a benign adrenal tumour (zona glomerulosa). Aldosterone is secreted in excess and results in hypertension and hypokalaemia. Diagnosis - Primary hyperaldosteronism - Renin – angiotensin system should be suppressed (exclude secondary hyperaldosteronism). Treatment - Removal of tumour - Aldosterone receptor antagonist: spironolactone - If both adrenal glands are responsible then patient should stay on spironolactone. Pharmacology The treatment of Conn’s syndrome involves the use of aldosterone receptor antagonists. Name – spironolactone Usage – treating primary hyperaldosteronism, oedema, congestive heart failure, nephrotic syndrome and cirrhosis of the liver. Mode of Action – it is a prodrug that is converted to carenone. This competitively antagonises the mineralocorticoid receptor. It also therefore decreases Na+ reabsorption and K+ excretion. Side effects - Menstrual irregularities, gynaecomastia (androgen receptor binding), GI tract irritation, blood dyscrasias. Should not be used in renal or hepatic disease. Phaeochromocytomas These are tumours of the adrenal medulla that secrete catecholamines (adrenaline and noradrenaline). Symptoms of Phaeochromocytoma • Hypertension in young people. • Episodic severe hypertension (after abdominal palpation). • Can lead to myocardial infarction and stroke. • The high adrenaline can cause ventricular fibrillation. • • • Treatment for Phaeochromocytoma Surgery to remove tumour. Anaesthetic should be cautioned as it could have hypertensive effects. Should be immediately given α and β blockers. Extra Facts 10 % of tumours are extra-adrenal (sympathetic chain). 10 % of tumours are malignant. 10 % of tumours are bilateral. (both glands). Pharmacology In patients with phaeochromocytoma β blockers are given. Name – Propanolol Usage – anti-hypertensive, glaucoma, angina, anxiety, cardiac arrhythmias. Mode of action – blocks β1 and β2 adrenoceptors and hence causes decrease in heart rate, peripheral resistance, blood pressure, stoke volume, reduces renin release, and central sympathetic outflow. Side effects – bronchoconstriction (not used in asthmatics), cold extremities, heart failure, heart block, also care when used in diabetics as it blocks glycolysis, increase in GI tract motility. Can cause nightmares. Name – Phentolamine Usage – phaeochromocytoma, “cheese reaction” to tyramine. Mode of Action – blocks α adrenoceptors causing fall in arterial blood pressure and reduced peripheral resistance. Side effects – reflex tachycardia, postural hypotension, flushing (increase flow through cutaneous splanchnic vascular beds, nasal congestion, failure to ejaculate, pupillary constriction (block of adrenergic tone to radial muscle of iris). Name: Phenoxybenzamine Usage: used in conjunction with β-adrenoceptor antagonists (propranolol, atenolol) to treat hypertensive episodes in phaeochromocytoma and to prepare patients for surgery. Mode of Action: binds to α adrenoceptors, reduces blood pressure by blocking α1 receptors. It is a non-selective antagonist of acetylcholine, histamine and 5-HT. Side effects: postural hypotension, reflex tachycardia and increased cardiac output.