Endocrine – Adrenal Gland

Endocrine – Adrenal Gland
Part 1
Adrenal Gland
• Description
– AKA
• Suprarenal gland
– Location
• On top of each kidney
– Composed of:
• Adrenal cortex
• Adrenal Medulla
Hormone & Function
• Adrenal Cortex
– Mineralocortioids
• Aldosterone
– Function
• Regulates electrolyte
& fluid homeostasis
Hormone & Function
• Adrenal Cortex
– Glucocorticoids
• Cortisol
• Hydrocortisone
– Function
• Stim. gluconeogenesis
& h blood glucose
• Anti-inflammatory
• Anti-immunity
• Anti- allergy
Hormone & Function
• Adrenal Cortex
– Androgen
• Sex hormones
– Function
• Female
– Stim. Sex drive
• Men
– Negligible
Hormone & Function
• Adrenal Medulla
– Epinephrine
• Adrenaline
– Function
• Prolong & h SNS
(sympathetic nervous system) response to stress
Hormone & Function
• Adrenal Medulla
– Norepinephrine
– Function
• Prolong & h SNS
(sympathetic nervous system) response to stress
Effects of Epinephrine & Norepinephrine a.
h cardiac output b.
h metabolic rate c. Vasoconstriction d.
h respiratory rate
Adrenal Cortex
• The cortex synthesizes & secretes 30+ different steroids.
– Glucocorticoids
– Mineralocorticoids
– Androgens
Learning Tip
SALT, SUGAR & SEX
• Aldosterone = promotes salt retention
• Cortisol= sugar
• Androgens = sex hormones
Negative feedback loop
• Stress
• Hypothalamus
• Stimulates Anterior Pituitary
• Secretes ACTH target cell
• Adrenal cortex
• Secretes Cortisol specific action
• h metabolic activity
• Helps manage stress
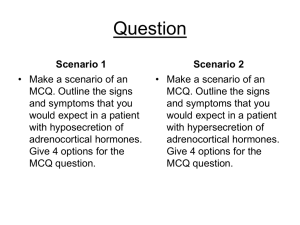
Cushing disease/ syndrome
• Description
– Cortisol excess
Cushing disease/ syndrome
• Pathyophysiology
– Diurnal rhythm
• h in AM
– Normal secretion of cortisol h in times of stress
– In Cushing's, cortisol is hypersecreted without regard to stress or time of day .
Cushing disease/ syndrome
• Etiology
– h secretions ACTH
– Pituitary CA
– Lung tumor
– **#1 prolonged use of glucocorticoid meds for inflammatory disorders
• Rheumatoid arthritis
• COPD
Cushing disease/ syndrome
• Etiology
– Iatrogenic
• Caused by treatment or diagnostic procedure
– Females > Male
Cushing disease/ syndrome
• Signs & Symptoms
– Adiposity
• Deposits of adipose tissue in the face, neck & trunk
• Moon shaped face
• Buffalo hump
Cushing disease/ syndrome
• S&S
– Weight gain
– Na & H20 retention
– K+ is lost
• Hypokalemia
– Purple striae on the abdomen
– Hirsutism
–
Cushing disease/ syndrome
• S&S
– This extremities d/t muscle wasting
– Boys = early onset of puberty
– Girls = masculine characteristics
– C/O fatigue, muscle weakness, sleep disturbance, amenorrhea, i libido, irritability, emotional labiality
Cushing disease/ syndrome
• S&S
– Could be:
• Petechiae
• Eccymoses
• i wound healing
• Swollen ankles
Cushing disease/ syndrome
Complications
• h calcium reabsorption from the bone leading to osteoporosis & pathologic fractures
• Cortisol causes insulin resistance and
• ↑ hepatic gluconeogenesis and insulin resistance
• Leads to glucose intolerance and diabetes mellitus
Cushing disease/ syndrome
Complications
• Frequent infections & slow wound healing
– Suppressed inflammatory response can mask severe infections
– Cortisol is an immunosuppressive
• Deceased ability to handle stress
– Psych problems i.e. mood swings
Cushing disease/ syndrome
• Diagnosis
– Plasma Corticol level
– ACTH level
– Adrenalangiography
Cushing disease/ syndrome
Medical management
• Early dectection key
• #1 goal = restore hormonal balance
• Usually meds.
Cushing disease/ syndrome
Med. Management
• Tx based on causative factor
• If adrenal cancer
– Surgery
• If caused by steroid meds
– Change regiment
– Risk to benefit analysis
Cushing disease/ syndrome
• Surgical management
• If pituitary gland
– Hypophysectomy
• If adrenal tumor
– Adrenalectomy
Cushing disease/ syndrome
• Aminoglutethimide
(cytadren)
– Action
• Inhibits synthesis of adrenal steroids
– S/E
• Dizziness or drowsiness
– Nrs.
• Instruct to avoid activities that need mental alertness
Cushing disease/ syndrome
• Ketoconazole (Nizoral)
– Action
• Antifungal
• Inhibits adrenal steroidogenesis
Cushing disease/ syndrome
Diet
• High in protein
• High K+
• Low sodium
• Reduces carbs & calories
Cushing disease/ syndrome
Nursing Management
• Rx history
• VS
• Lung auscultation
– Crackles
• Edema
• Skin integrity
• Glucose levels
• S&S of infection
Adrenalectomy
• Pre-op
– Electrolyte imbalance
– Hyperglycemia
– Prevent adrenal crisis
• Administer glucocorticoids!
• Sudden drop in hormones crisis
Adrenalectomy
• Post-op
– Fluid & electrolyte changes
– Replace glucocorticoids, mineralocorticoids for life
– Bilateral???
Addison’s Disease
• Description
– i corticol
– Adrenal hypofunction
– Adrenal insufficiency
– Adrenalcortical insufficiency
Addison’s Disease
• Pathophysiology
– 90% of adrenal gland destroyed
– Autoimmune disease
– Primary
• ACTH may be high
– Secondary
• ACTH will be low
Addison’s Disease
Etiology
• Primary
– Bilateral adrenalectomy
• Secondary
– i ACTH from pituitary
– i hypothalamus stimulation
Addison’s Disease
Etiology
• Prolonged use of coticosteroid Rx
• i ACTH
• i hormonal release from adrenal gland
• *** esp. at risk if drugs abruptly DC’ed
– Taper dose
Addison’s Disease:
Signs & Symptoms
• Hypotension
– Lack of aldosterone
– Na+ & H2O loss
– K+ reabsorption
• Tachycardia
• Orthostatic hypotension
Addison’s Disease:
Signs & Symptoms
• Bronze coloration of skin
• Hypoglycemia
• Vitiglio
• Fatigue, muscle weakness
• Weight loss
• Crave salty foods
Addison’s Disease:
Signs & Symptoms
• i tolerance for stress
– Anxious
– Irritable
– Confused
• Pulse
– Weak
• GI upset
– N/V
– Anorexia
Addison’s disease:
Complications
• Adrenal crisis
– Acute Addison’s dis
– May occur
• Trauma
• Surgery
• Stress
• Abrupt withdrawl of cortisone meds
Addison’s disease:
Complications
• Adrenal Crisis
– S&S
• Na+ & H20 loss
• Hypotension
• Dehydration
• Tachycardia
– IV & administer hydrocortisone
Addison’s disease:
Medical Management
• Restore fluid and electrolyte balance
• Replacement of deficient adrenal hormones
– Glucocorticoids
(hydrocortisone)
– Mineralocorticoids
(fludrocortisone)
Addison’s disease:
Pharmacological
• Lifetime steroids
• Glucocorticoids
– Hydrocortisone
(hydrocortone)
• Mineralocorticoids
– Fludrocortisone acetate (Florinef)
• Diurnal rhythm
– 2/3 AM
– 1/3 PM
• High in Na+
• Low in K+
Addison’s disease:
Diet
Addison’s disease:
Nursing Management
• Diagnosis???
• Fluid volume deficit
– r/t
• i Na+ level
• Vomiting
• h renal losses
– A.M.B.
• Poor skin turgor
• Weight loss
• Orthostatic hypotension
Addison’s disease:
Nursing Management
• qDay wts
• I&O
• Glucose
• K+ & Na+
• Skin turgor
• Orthostatic hypotension
Hypofunction Hyperfunction
Disorder
Addison’s disease
Cushing syndrome
S&S Na+ & H20 loss
Hypotension
Hypoglycemia
Fatigue
Hyperkalemia
Na+ & H20 retention
Wt. gain
Hyperglycemia
Buffalo hump
Moon face
Hypokalemia
Hypofunction Hyperfunction
Usual tx Glucocorticoids
Meneralocorticoid
Restore fluid
Nrs Dx
Alter steroid Rx
Surgery
Fluid volume deficit Fluid volume excess
Glucose intolerance
Diet h
Na+ i
K+ i
Na+ h
K+
Pheochromocytoma:
Description
• AKA chromaffin cell tumor
• Rare disease
• Characterized by paroxysmal or sustained hypertension
– d/t excess secretion of epi and norepi
Pheochromocytoma:
Pathophysiology
• Caused by a tumor
– Usually Rt. adrenal
• Etiology
– Idiopathic
• Stress can bring on an attack
Pheochromocytoma:
Signs & Symptoms
• HTN
– > 115 mmHG diastolic
– Intermittent
– Unstable
• Tachycardia
• Unrelenting H/A
• Profuse diaphoresis
• Palpitations
Pheochromocytoma:
Signs & Symptoms
• Visual disturbances
• N/V
• Feeling of apprehension
• Elevated blood glucose levels
Pheochromocytoma:
Complications
• Stroke
• Retinopathy
• Heart disease
• Kidney damage
Pheochromocytoma:
Medical Management / Surgical
• Treatment of choice is…
– Surgery
• Stable a surgery
• Adrenal gland removed
• BP
Pheochromocytoma:
Pharmacological
• Phentolamine mesylate (Regitine)
• Nitroprusside sodium
(Nipride)
– HTN
Pheochromocytoma:
Diet
• h protein
• Avoid caffeine
Pheochromocytoma:
Nursing Management
• Monitor BP
• VS
• Na+ levels